Medical expert of the article
New publications
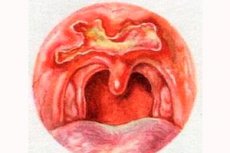
Syphilis of the pharynx
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
If in the first half of the 20th century syphilis of the pharynx was extremely rare, then in the last decade of the last century and at the beginning of the 21st century the number of this localization of syphilis has been steadily growing, as has the total number of genital forms of this venereal disease.
Due to the large morphological diversity of tissues that make up the pharynx, its lesions with syphilis are distinguished by a number of features that are not inherent in other localizations of this disease. In addition, many saprophytes and opportunistic microorganisms vegetate in the oral cavity and pharynx, which significantly modify the classic picture of syphilides and often serve as sources of secondary infection. It should also be noted that both primary and secondary manifestations of syphilis have a special tropism for the lymphadenoid formations of the pharynx, in particular, the palatine tonsils.
Cause of syphilis of the pharynx
The causative agent of syphilis is the pale treponema, which looks like a thin spiral thread 4 to 14 microns long with small uniform curls. Infection occurs during close contact between a healthy person and a sick person who has one or another infectious form of syphilis at the time of contact. Patients in the primary and secondary periods of syphilis are most contagious. Manifestations of the late (tertiary) period are practically not contagious due to the insignificant number of treponemas in the lesions.
The primary period of syphilis is characterized by the appearance of a primary chancre, which is primarily localized on the palatine tonsils, then on the soft palate and palatine arches. In rare cases, it can occur in the area of the nasopharyngeal opening of the auditory tube as an infection introduced during its catheterization; in extremely rare cases, with syphilis of the pharynx, a primary chancre can be found in two different places in the pharynx. Often, the primary chancre remains unnoticed against the background of a secondary infection. The most common infection with syphilis of the pharynx occurs through kissing and oral sex. Infection through an infected object (a glass, spoon, toothbrush, etc.) occurs extremely rarely, if this route of infection is possible at all. In addition to the sexual and household route of infection with syphilis, in rare cases there is a transfusion route, when the infection is transmitted by transfusion of infected blood.
Hard chancre occurs in the primary period of syphilis 3-4 weeks after infection at the site of penetration of pale treponema with the simultaneous appearance of regional lymphadenitis. Hard chancre, or primary syphiloma, is a small painless erosion (0.5-1 cm) or ulcer of a round or oval shape, with smooth edges and a dense infiltrate at the base, with a smooth shiny surface of red color. Inflammatory phenomena in its circumference are absent. When palpating the edges of the ulcer on both sides under the fingers, a cartilaginous density is felt, which is typical for primary syphilid. However, in the pharynx, manifestations of primary syphilis have features and can manifest themselves in various clinical forms.
Lesions of the pharynx in congenital syphilis
A distinction is made between early and late manifestations.
Early signs appear no later than 5-6 months after the birth of the child and are similar to those pathomorphological elements that occur in the secondary period of acquired syphilis. In addition, the newborn develops persistent syphilitic rhinitis, pseudomembranous lesions of the mucous membrane, pharynx, simulating diphtheria, skin stigmas resembling pemphigus of the palmar and plantar surfaces with lamellar desquamation of the epidermis, deep cracks in the lip area, which subsequently transform into radial scars in the corners of the mouth characteristic of congenital syphilis, and other signs of congenital syphilis.
Late signs appear in adolescence or youth. They are manifested by signs characteristic of pharyngeal lesions of tertiary syphilis, to which are added congenital syphilitic lesions of the nose, ear, teeth, eyes, internal organs, as well as various kinds of functional disorders of the senses and movements.
Symptoms of syphilis of the throat
The anginal form manifests itself as acute unilateral prolonged tonsillitis with a rise in body temperature to 38°C and moderate pain in the throat when swallowing. The affected tonsil is sharply hyperemic and enlarged. The primary chancre is usually hidden behind the triangular fold or in the subtonsillar fossa. Regional lymphadenitis develops simultaneously.
The erosive form is characterized by the appearance of a superficial erosion on one of the tonsils with ridge-shaped rounded edges, covered with gray exudate. When palpated, a sensation of cartilaginous density of the bottom of the erosion, specific to the primary syphilitic affect, is created.
The ulcerative form is manifested by the appearance of a round ulcer on the surface of the tonsils, the bottom of which is covered with a false gray film (syphilitic diphtheroid). This form is characterized by a rise in body temperature to 38 ° C and above, severe dysphagia, spontaneous and swallowing pain in the throat, unilateral, corresponding to the side of the lesion, otalgia, contracture of the temporomandibular joint, salivation. In its manifestations, this form is very similar to a peritonsillar abscess.
The pseudophlegmonous form resembles the clinical course of peritonsillar phlegmon, and this often misleads the ENT doctor. Diagnostic puncture of the suspected phlegmon or its trial opening does not bring results, the body temperature continues to remain high (39-40°C), subjective and one-sided objective signs of "phlegmon" increase, and then resort to the use of massive doses of penicillin, which, of course, in syphilis quickly improves the general condition of the patient and leads to a visible normalization of the inflammatory process in the throat. In fact, in this case, if we are talking about a syphilitic infection, this is only an apparent recovery, while the specific process continues.
The gangrenous form occurs with superinfection with fusospirillum microbiota. In this case, granulation growths (very rare) appear on the surface of the tonsil or tonsil gangrene develops: the patient's condition deteriorates sharply, signs of a general septic state appear, the body temperature reaches 39-40.5 ° C, chills, profuse sweats occur, the tonsil and surrounding tissues undergo gangrenous decay caused by the symbiosis of anaerobes with opportunistic aerobes and pale treponema. A feature of syphilitic chancre of the pharyngeal localization is its long course and the absence of the effect of any symptomatic treatment. After 4-6 weeks, the primary chancre of the palatine tonsils undergoes scarring, but the syphilitic process continues for many months in the form of roseola scattered throughout the mucous membrane and generalized adenopathy.
All the above-mentioned pharyngeal manifestations of primary syphilis are accompanied by characteristic unilateral regional lymphadenitis: a sharp increase in one lymph node with many smaller nodes in its circumference, absence of peri-adenitis, increased density and painlessness of the nodes. All other lymph nodes of the neck are quickly involved in the process, which will create the impression of infectious mononucleosis.
Diagnosis of syphilis of the pharynx
Diagnosis of pharyngeal syphilis is quick and easy if the doctor suspects the presence of a hard chancre in the patient from the very beginning. However, the polymorphism of syphilitic manifestations in the pharynx and the lack of experience in diagnosing syphilides ad oculus often leads to diagnostic errors, which may include diagnoses such as vulgar angina, diphtheritic angina, Vincent's angina, etc. Hard chancre can be confused with chancre-like amygdalitis of Mure, tuberculous ulcer and enthelioma of the tonsil and many other ulcerative and productive processes developing in the palatine tonsils. The most effective method for early diagnosis of syphilis with hard chancre, wherever it occurs, is electron microscopy of pathological material to detect in situ pale treonema, which is especially important given that known serological reactions (for example, Wasserman) become positive only 3-4 weeks after the appearance of hard chancre.
The secondary period of syphilis lasts 3-4 years and occurs if the primary period has passed unnoticed. Generalization of the process with damage to the skin and mucous membrane in the form of characteristic rashes (syphilides: roseola, papules, pustules containing pale treponemas), disruption of the general condition of the body (malaise, weakness, subfebrile temperature, headaches, etc.), changes in the blood (leukocytosis, anemia, increased ESR, positive serological reactions) is noted; damage to internal organs and bones is possible.
On the oral mucosa, soft palate, tonsils and especially on the palatine arches, sharply demarcated erythematous and papular syphilides appear against the background of healthy mucosa, while the posterior pharyngeal wall remains intact. They soon acquire an onal-white color due to swelling and maceration of the epithelium and resemble slight burns of the mucous membrane that occur when it comes into contact with a concentrated solution of silver nitrate. Papules are surrounded by a bright red rim. In smokers or in people with dental diseases (caries, periodontitis, chronic stomatitis, etc.), due to the presence of pathogenic microbiota in the oral cavity, papules quickly ulcerate, become painful and can transform into condyloma-like formations. Secondary syphilides of the mucous membrane of the upper respiratory tract and genitals are extremely contagious.
In the secondary period of syphilis, the following forms of pharyngeal lesions are distinguished.
The erythematous-opalescent form of syphilitic pharyngitis is characterized by hyperemia of the mucous membrane of the pharynx, palatine tonsils and the free edge of the palatine arches and soft palate. Enanthem may be of a bright diffuse nature, as in scarlet fever, sometimes it affects only individual areas of the mucous membrane or is not expressed at all, causing only soreness in the throat at night, without a temperature reaction. The resulting syphilitic enanthem does not respond to any symptomatic treatment, as well as headaches that are not relieved by analgesics.
The hypertrophic form concerns the lymphoid apparatus of the pharynx and completely captures the entire lymphadenoid ring of the pharynx. The lingual and palatine tonsils are most susceptible to damage. Damage to the lymphoid apparatus of the pharynx and larynx causes the development of an uncontrollable cough and leads to dysphonia (hoarseness of voice) and aphonia. At the same time, regional adenopathy develops with damage to the submandibular, cervical, occipital and pretracheal lymph nodes. The indicated pathological changes continue for a long time (unlike banal inflammatory processes) and do not respond to conventional therapeutic effects.
Diagnosis of pharyngeal syphilis in the secondary period, carried out only on the basis of an endoscopic picture, is not always an easy task, since a large number of diseases of the oral cavity and pharynx of a non-specific nature can compete in their appearance with the same number of atypical oropharyngeal forms of the second period of syphilis. Such diseases, from which syphilitic lesions of the pharynx that occur in the second period of syphilis should be differentiated, may include vulgar angina, angina of herpetic (viral) etiology, aphthous bucopharyngeal processes, some specific (non-luetic) diseases of the tongue (tuberculosis, complicated forms of "geographical" tongue, malignant tumors and banal inflammatory reactions), aphthous stomatitis, leukoplakia, drug-induced stomatitis, etc. An important diagnostic sign of syphilitic lesions of the pharynx is the manifestation of an inflammatory reaction only along the edges of the palatine arches or soft palate. The main rule for diagnosing syphilis is to conduct serological reactions for all diseases of the mucous membrane of the oral cavity and pharynx, regardless of their seemingly "favorable" appearance.
The tertiary period of syphilis develops after 3-4 years (rarely after 10-25 years) in patients who did not receive adequate treatment during the secondary period. This period is characterized by lesions of the skin, mucous membrane, internal organs (visceral syphilis, most often manifested by syphilitic aortitis), bones, and the nervous system - neurosyphilis (syphilitic meningitis, tabes dorsalis, progressive paralysis, etc.). A typical morphological element for this period of syphilis is the appearance on the skin, mucous membrane and other tissues of dense small formations (tubercles) or large ones (gummas), prone to decay and ulceration. The tertiary period of syphilis of the pharynx can occur in three clinical and pathomorphological forms: classical gummatous, diffuse syphilomatous, and early ulcerative-serpeptiform.
The gummatous form goes through 4 stages:
- the stage of formation of a dense, painless syphilid, well differentiated by palpation and not fused with surrounding tissues, the size of a pea seed to a nut;
- the softening stage, during which, over the course of 2-3 weeks or several months, a zone of necrosis forms in the center of the syphilis (gumma), creating a feeling of fluctuation;
- the stage of ulceration of the gumma and the rupture of its contents to the outside; the ulcer is a deep round cavity with steep edges, an uneven bottom, covered with the remains of decayed tissue;
- stage of scarring through the formation of granulation tissue.
Gumma can be located on the back wall of the pharynx, on the tonsils, on the soft palate, leaving behind a tissue defect.
The gumma of the soft palate has the form of a hemisphere, quickly ulcerates and leaves behind a rounded through perforation of the soft palate at the base of the uvula, often destroying it as well. In this case, open nasal speech and the ingress of liquid food into the nose occur. The gumma of the hard palate develops more slowly and leads to the destruction of the palatine bones, leaving behind a wide passage into the nasal cavity. The defeat of the palatine tonsils leads to its total destruction with the capture of surrounding tissues and subsequent significant cicatricial deformation of the pharynx. In the tertiary period, specific adenopathy is absent, but if regional lymphadenitis occurs, it indicates a secondary infection of the affected areas of the pharynx.
Gumma of the hard and soft palate is most often found in the form of a diffuse infiltrate, less often - in the form of a limited gummatous tumor. The process of gummatous infiltrate formation begins unnoticed and painlessly with thickening and compaction of the soft palate, which loses mobility, becomes rigid and does not respond with a typical movement when pronouncing the sound "L". The infiltrate acquires a bluish-red color and clearly stands out against the background of the rest of the unchanged mucous membrane. Subsequently, the gumma of the soft palate quickly disintegrates with the formation of deep, sharply defined ulcers and perforations. Damage to the bones of the hard palate occurs in the form of diffuse or limited syphilitic osteoperiostitis, leading to necrosis and melting of bone tissue and perforation of the palate. Destructive changes in the soft and hard palate lead to a number of functional disorders, which primarily include swallowing disorders, open nasal speech and impaired locking function of the soft palate.
In the absence of timely treatment, further destruction of the soft tissues and bone formations of the pharynx occurs: total destruction of the bottom of the nasal cavity, palatine tonsils, palatine arches, root of the tongue, etc. The capture of large vessels by the necrotic process (for example, the lingual artery, internal and external carotid, ascending palatine arteries, as well as the tonsillar artery) leads to nephrotic, often fatal bleeding.
After healing of gummatous-ulcerative lesions, dense scars and adhesions are formed in various directions between the walls of the pharynx, pharynx and soft palate, which often lead to pharyngeal stenosis or its complete atresia, resulting in gross functional disorders that require further plastic surgical interventions. Scars after deep ulcers that form on the back wall of the pharynx have a characteristic star-shaped form and are the cause of the development of severe atrophic pharyngitis. Fusion of the soft palate with the back wall of the pharynx leads to partial or complete separation of the oropharynx from the nasopharynx, resulting in impaired nasal breathing, swallowing and dysphonia in the form of closed nasal twang. The occurrence of scars in the area of the nasopharyngeal opening of the auditory tube causes dysfunction of its function and corresponding hearing disorders.
The diffuse syphilitic form is the most common form of pharyngeal lesions in the tertiary period of syphilis. It is characterized by multiple lesions of the pharynx, which are in various stages of their development, and subsequent multiple cicatricial processes. In the initial stage, this form can be mistaken for granulomatous hypertrophic pharyngitis or Isambert's disease, observed in patients with advanced forms of laryngeal tuberculosis. This form occurs with an increase in body temperature and regional lymphadenitis. A more extensive syphilitic ulcer can be mistaken for pharyngeal carcinoma, in which early metastasis to the cervical lymph nodes is observed.
The early form of syphilis of the pharynx (Syphylis tubero-ulcerosa serpiginosa) occurs very rarely and is characterized by the simultaneous occurrence of syphilides, characteristic of secondary and tertiary syphilis, in which case an extensive creeping shallow ulcer occurs, located mainly along the edge of the uvula and soft palate.
All of the above-mentioned forms of syphilis of the pharynx leave behind extensive cicatricial changes, which entail pronounced functional impairments both in relation to the act of swallowing and voice and speech formation.
What do need to examine?
How to examine?
What tests are needed?
Who to contact?
Treatment of syphilis of the throat
Treatment of syphilis of the pharynx is carried out in combination with general specific treatment in the dermatovenereology department using special methods in accordance with the instructions approved by the Ministry of Health of Ukraine.
Prognosis for syphilis of the pharynx
The prognosis for fresh forms of syphilis and timely treatment is favorable for life, but its consequences for many vital functions, especially for the nervous system and internal organs, the damage of which is directly determined by syphilitic infection, can lead to profound disability of patients and their premature death.


 [
[