Medical expert of the article
New publications
Osteoporosis and back pain
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
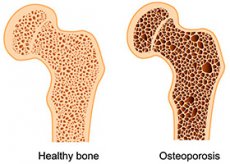
Osteoporosis is a systemic metabolic disease of the skeleton, characterized by decreased bone mass and microarchitectural changes in bone tissue, which in turn leads to bone fragility and a tendency to fracture (WHO, 1994).
Pathogenetic classification of osteoporosis
- Primary osteoporosis
- postmenopausal osteoporosis (type 1)
- senile osteoporosis (type 2)
- juvenile osteoporosis
- idiopathic osteoporosis
- Secondary osteoporosis
- endocrine system diseases
- rheumatic diseases
- diseases of the digestive system
- kidney disease
- blood diseases
- genetic disorders
- other conditions (oophorectomy, COPD, alcoholism, anorexia, eating disorders)
- medications (corticosteroids, anticonvulsants, immunosuppressants, aluminum-containing antacids, thyroid hormones)
Risk factors for osteoporosis: genetic
- Race (white, asian)
- Old age
- Heredity
- Low body weight (<56kg) hormonal
- Female gender
- Late onset of menstruation
- Amenorrhea
- Infertility
- Early menopause lifestyle
- Smoking
- Alcohol
- Caffeine
- Physical activity:
- low
- excessive
- Calcium and vitamin D deficiency in food
- Medicines
- Glucocorticoids
- Heparin
- Anticonvulsants
- Thyroid hormones
- Other diseases
- Endocrine
- Rheumatic
- Tumors
- Hematological
- Livers
- Kidneys
- Radiation therapy
- Oophorectomy
Risk factors for fractures:
- internal factors (various diseases or age-related decline in neuromotor regulation, decreased stability, muscle weakness, hearing loss, senile dementia, use of barbiturates, tranquilizers, antidepressants);
- environmental factors (ice, loose rugs, slippery floors, poor lighting in public places, lack of handrails on stairs).
Instrumental diagnostics of osteoporosis:
- X-ray of the spine:
- - late diagnosis (loss of more than 30% of bone mass is diagnosed)
- - detection of fractures (X-ray morphometry)
Quantitative computed tomography
- Ultrasound densitometry (screening method)
- Dual Energy X-ray Absorptiometry, Standard Method: Early Diagnosis (1-2% Bone Loss)
The main symptom of osteoporosis is a decrease in bone mineral density (BMD) that develops in all areas of the musculoskeletal system, but to a greater extent and at earlier stages of development, pathological changes affect the spinal column, which allows us to consider it as a diagnostic "object" with which we can identify the earliest manifestations of osteoporosis.
One of the characteristic clinical signs of osteoporosis are vertebral fractures. Clinical signs of vertebral fractures (back pain and decreased growth) are observed only in 1/3 of patients, while the rest show osteoporotic deformation of the vertebrae without clinical manifestations. Reformation can be most accurately identified by assessing lateral radiographs at the level of Th1V-ThXII, LII-LIV.
Roentgenomorphometric examination consists of changing the height of the vertebral bodies from ThIV to LIV on a lateral radiograph in three of their sections: anterior (value A), middle (value M) and posterior (value P). Considering the fact that the sizes of the vertebral bodies can change depending on the patient's gender, age, body size, height, it is advisable to analyze not the absolute values of the obtained sizes, but their ratios - vertebral body indices, for greater reliability. According to the three absolute sizes, the following indices are distinguished:
- A/P index - anterior/posterior index (ratio of the height of the anterior edge of the vertebral body to the height of the posterior)
- M/R index - middle/posterior index (ratio of the height of the middle part of the vertebra to the height of the posterior edge of the vertebra)
- index P/P1 - posterior/posterior index (the ratio of the height of the posterior edge of the vertebra to the height of the posterior edge of the two overlying and two underlying vertebrae).
The degree of deformation is determined by the Felsenberg method - by the ratio of the height of individual parts of the vertebral bodies in percent. Normally, the index is 100%, that is, all dimensions of the vertebral body have equal values. Minimal osteoporotic deformation is characterized by an index of 99-85% (provided there are no inflammatory and non-inflammatory diseases of the spine).
Symptoms of osteoporosis consist of three main groups of signs:
- Non-painful manifestations associated with structural changes in the vertebrae and skeletal bones (changes in posture, decreased height, etc.)
- A non-specific, but almost always occurring pain syndrome, from minor to intense, of varying localization and severity.
- Changes in the psycho-emotional sphere
Clinically significant non-painful signs of osteoporosis are thoracic kyphosis, often causing shortening, compression of the patient's trunk, low position of the ribs, almost on the iliac crests. Lumbar lordosis increases or flattens. Changes in physiological curves and posture lead to shortening of the spinal muscles, the occurrence of pain from muscle strain (the predominant localization of such pain is paravertebral, increased pain with prolonged vertical position, decreased intensity when walking). An important diagnostic criterion is a decrease in the patient's height by more than 2.5 cm per year or 4 cm during life. The head-symphysis and symphysis-foot distances are normally the same, a decrease in the first distance to the second by more than 5 cm indicates osteoporosis. When measuring height accurately, a decrease in it by 6 mm may indicate a compression fracture of the vertebral body.
Back pain is the most common complaint presented to a doctor by patients with osteoporosis. Acute and chronic pain are distinguished. Acute pain syndrome is usually associated with the development of a compression fracture of the vertebra due to minimal trauma (occurring spontaneously or when falling from a height no higher than (the person's own height), caused by coughing, sneezing, or sudden movement). The pain can radiate along the radicular type to the chest, abdomen, thigh, and sharply limit motor activity. Intense pain decreases after 1-2 weeks until it stops within 3-6 months against the background of increased lumbar lordosis or thoracic kyphosis, or becomes chronic.
Chronic pain can be episodic, associated with lifting weights, uncoordinated movement, or constant, aching, accompanied by a feeling of fatigue, heaviness in the back, in the interscapular region. In this case, pain increases with prolonged walking, after being forced to stay in one position. The intensity decreases after resting in a lying position. NSAIDs in most cases do not relieve pain, or reduce its intensity slightly. The degree of pain varies from insignificant to severe in the same patient.
In addition to a compression fracture, pain may be caused by a partial fracture with periosteal hemorrhage, shortening of the paravertebral muscles, compression of muscles and ligaments. Violation of the rib arrangement, thoracic kyphosis can lead to pressure on the iliac crests, intervertebral joints with the appearance of pain in the back, ribs, pelvic bones, pseudoradicular pain in the chest. Less common with osteoporosis are joint pain, gait disturbance, and lameness.
Often, pain occurs when the chest is compressed, less often diffuse pain in the bones is observed. There is a test of indirect load on the spine: the doctor presses from above on the patient's outstretched arms. With osteoporosis, the patient feels severe pain in the spine. Sometimes patients complain of pain in the thoracolumbar spine when suddenly lowering from a "on tiptoe" position.
There are frequent complaints of decreased performance, increased fatigue, irritability, agitation, and sometimes complaints of a depressive nature.
A characteristic feature of the course of osteoporosis is the absence of a characteristic clinical picture until the development of significant changes in the density and architecture of bone tissue, provoking the development of osteoporotic fractures.
Treatment of osteoporosis
Treatment of osteoporosis depends on the value of the t-criterion determined by dual-energy densitometry, reflecting the number of standard deviations (SD) above and below the mean of the peak bone mass of young women aged 30-35 years and the presence of osteoporotic fractures
Treatment of osteoporosis is divided into three aspects:
- etiotropic
- symptomatic
- pathogenetic.
Etiotropic treatment of osteoporosis involves treating the underlying disease in secondary osteoporosis and correcting or discontinuing iatrogenic drugs for osteoporosis. Symptomatic therapy methods are mandatory in the treatment and prevention of osteoporosis. They include various schools, educational programs, maximum impact on modifiable risk factors, quitting bad habits, physical exercises according to a special program developed for patients with osteoporosis. If necessary, the possibility of wearing hip protectors for people with a high risk of developing hip fractures (thin people, people who have already had hip fractures in their history, who have a high tendency to fall) is considered, even if this group of people does not have a reliably confirmed diagnosis of osteoporosis. Also included in this group are the use of painkillers during periods of exacerbation of pain, massage, surgical methods of treating terelomas. A number of authors attribute calcium therapy to symptomatic therapy, without denying its indisputable preventive value, especially in adolescence, during the period of peak bone mass formation.
The goal of pathogenetic treatment is to restore the normal process of bone remodeling, including suppression of increased bone resorption and stimulation of decreased bone formation. Osteoporosis therapy is carried out both as mono- and combined therapy, depending on the etiology, severity of osteoporosis, somatic status.
Pathogenetic therapy involves taking the following medications:
- slowing bone resorption: bisphosphonates (alendronate, alendronate and vitamin D, zoledronic acid), calcitonin, selective estrogen receptor modulators, estrogens, estrogen-progestogen drugs, strontium ranelate.
- primarily those that enhance bone formation: PTH, fluorides, anabolic steroids, androgens, growth hormone, strontium ranelate.
- having a multifaceted effect on bone tissue: vitamin D and its active metabolites, osteogenon, ossein-hydroxyapatite complex
- Calcium salts: used as part of combination therapy or for primary prevention of osteoporosis.


 [
[