Medical expert of the article
New publications
Osteoarthritis: Effect of meniscectomy on articular cartilage
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
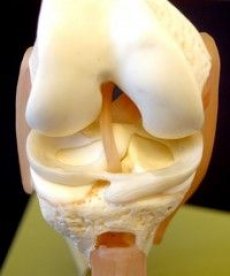
As stated earlier, the articular menisci play an important role in normal joint function. The menisci are structures that increase the congruence of the articular surfaces of the femur and tibia, enhance lateral stability, and improve the distribution of synovial fluid and the exchange of nutrients with the articular cartilage. Total or partial meniscectomy leads to a change in the direction of the load on the articular surface of the tibia, resulting in degeneration of the articular cartilage.
Many studies have been devoted to the study of the effect of meniscectomy on the biomechanics of the joint, as well as the induction of degenerative processes in the articular cartilage and subchondral bone in animals (usually dogs and sheep). Initially, researchers performed an ectomy of the medial meniscus of the knee joint, but it was later found that an ectomy of the lateral meniscus leads to a more rapid development of osteoarthritis.
Using lateral meniscectomy in sheep, Little et al. (1997) examined changes in articular cartilage and subchondral bone from several areas of the knee joint. Typical histological findings illustrating induced changes in articular cartilage 6 months after surgery were fraying of cartilage, decreased proteoglycan concentration, and decreased chondrocyte count. Under areas of altered cartilage in the subchondral bone, capillary growth into the calcified cartilage zone, outward displacement of the "wavy border," and thickening of the spongy substance of the subchondral bone were noted.
In the study by P. Ghosh et al. (1998) it was shown that 9 months after lateral meniscectomy in sheep there are signs of subchondral bone remodeling and an increase in its mineral density secondary to articular cartilage degeneration. In zones subject to abnormally high mechanical load due to removal of the lateral meniscus (lateral condyle of the femur and lateral plate of the tibia), increased synthesis of dermatan sulfate-containing proteoglycans was found, although increased synthesis of proteoglycans of the same type was also found in the cartilage of the medial plate. It turned out that dermatan sulfate-containing proteoglycans are represented mainly by decorin. Its highest concentration was found in the middle and deep zones of articular cartilage.
Along with the increase in the synthesis of dermatan sulfate-containing proteoglycans in the areas of cartilage bearing a high load due to the removal of the lateral meniscus, increased catabolism of aggrecan was detected, as evidenced by the release of its fragments into the nutrient medium from cartilage explants, as well as high activity of MMP and aggrecanases. Since inflammatory activity in this model of osteoarthrosis was minimal, the authors suggested that chondrocytes were the source of the enzymes.
Although many unanswered questions remain, the studies described above reveal a possible role for biomechanical factors in the pathogenesis of osteoarthritis. It is clear that chondrocytes are able to “sense” the mechanical properties of their environment, responding to changes by synthesizing ECM that can withstand greater loads and thus prevent cartilage damage. In young animals, moderate exercise induced the synthesis of aggrecan-rich ECM. This hypertrophic (or adaptive) phase of the chondrocyte response can last for several years, providing a stable level of mechanical load on articular cartilage. However, disruption of this balance due to increased intensity or duration of loading, or changes in normal joint biomechanics after injury or surgery, or a decrease in the ability of chondrocytes to enhance ECM synthesis in response to increased loading (during aging), the action of endocrine factors entails significant changes at the cellular and matrix levels: the synthesis of proteoglycans and type II collagen is inhibited, and the synthesis of decorin and collagen types I, III, and X is stimulated. Simultaneously with the change in biosynthesis, ECM catabolism increases, as well as the level of MMPs and aggrecanases. It is not known how mechanical loading promotes resorption of the surrounding ECM by chondrocytes; this process is probably mediated by prostanoids, cytokines (such as IL-1p or TNF-a, and free oxygen radicals). Here it is necessary to mention the role of synovitis in osteoarthritis, since the most likely source of the above-mentioned catabolism mediators may be macrophage-like synovocytes and leukocytes infiltrating the synovial membrane of the joint.
A study by OD Chrisman et al. (1981) showed that traumatic joint injury stimulates the production of a prostaglandin precursor, arachidonic acid. The membranes of damaged chondrocytes are considered to be the source of arachidonic acid. It is well known that arachidonic acid is rapidly converted into prostaglandins by the enzyme cyclooxygenase (COX). It has been demonstrated that prostaglandins, in particular PGE 2, interact with chondrocyte receptors, changing the expression of their genes. However, it remains unclear whether arachidonic acid stimulates or inhibits the production of proteinases and aggrecanases. Earlier studies have shown that PGE 2 increases MMP production and causes degradation of articular cartilage. According to the results of other studies, PGE 2 has an anabolic effect on the ECM, and also promotes the integrity of the ECM, inhibiting the production of cytokines by chondrocytes. It is possible that the conflicting findings of these studies are due to the different concentrations of PGE2 used in them.
A small amount of IL-1β (the main cytokine that stimulates the synthesis and release of MMPs, as well as inhibits the activity of their natural inhibitors) can be formed in response to damage to articular cartilage, which leads to further tissue degradation.
Thus, the studies described in this section have shown that maintaining a subthreshold dynamic load on the joint causes the proliferation of chondrocytes capable of enduring new mechanical conditions, which means the onset of the hypertrophic stage of osteoarthrosis. Hypertrophied chondrocytes are cells in the last stage of differentiation, which means that the expression of genes of the main matrix elements in them is altered. Therefore, the synthesis of aggrecan proteoglycans and type II collagen is inhibited, and the synthesis of decorin, collagens I, III and X types is increased.
A decrease in the content of aggrecan and type II collagen in the ECM, associated with an imbalance between the processes of synthesis and degradation, imparts to the articular cartilage the property of inadequately responding to mechanical stress. As a result, chondrocytes become unprotected, the process moves to the third, catabolic stage, characterized by excessive proteolytic activity and secretion of autocrine and paracrine regulatory factors. Morphologically, this stage is characterized by the destruction of the ECM of the articular cartilage; clinically, it corresponds to manifest osteoarthrosis. This hypothesis, of course, represents a simplified vision of all the complex processes occurring in osteoarthrosis, but it generalizes the modern concept of the pathobiology of osteoarthrosis.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]

