Medical expert of the article
New publications
Neurosyphilis
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Neurosyphilis is a form of syphilis, an infectious disease caused by the bacterium Treponema pallidum. This form is characterized by damage to the nervous system by the bacterium and can develop at any stage of the disease. Neurosyphilis can manifest in a variety of ways, including meningitis, spinal cord and brain damage, and nerve damage.
The infection proceeds in several stages, starting with primary syphilis, which is characterized by the appearance of a hard, painless ulcer at the site of entry of the bacterium. Secondary syphilis can be manifested by a skin rash, mucosal lesions and other symptoms. If left untreated, syphilis can progress to a latent stage that can eventually lead to tertiary syphilis with damage to the heart, blood vessels, eyes, bones, and nervous system, including the development of neurosyphilis. [1]
Symptoms of neurosyphilis can range from mild to severe and include headaches, dizziness, behavioral changes, paralysis, weakness in the limbs, visual disturbances, memory and coordination problems, and mental changes. Diagnosis of neurosyphilis includes analysis of cerebrospinal fluid, serologic tests for syphilis, and neurologic examination.
Treatment for neurosyphilis usually includes antibiotics, mainly intravenous penicillin, for several weeks. Early detection and treatment of syphilis can prevent the development of neurosyphilis and other serious consequences of the disease.
Epidemiology
Before the advent of antibiotics, neurosyphilis was common, occurring in 25-35 percent of patients with syphilis. It now occurs more often in patients with human immunodeficiency virus (HIV) infection, especially in those who are untreated, have low CD4+ counts, or detectable levels of HIV RNA. Despite this, early forms of neurosyphilis are more common than later forms. Risky sexual behavior makes people vulnerable to syphilis as well as HIV. Thus, neurosyphilis is more common among people who are also at high risk for HIV. [2], [3]
The risk of neurosyphilis is 2 to 3 times higher in whites than in blacks and 2 times more common in men than in women.
In some parts of Africa, the incidence may be approximately 2,300 cases per 100,000 population. [4]
Pathogenesis
The pathogenesis of neurosyphilis involves several key steps, from the invasion of the Treponema pallidum bacterium into the body to the development of neurologic lesions. Here are the main aspects of the pathogenesis of neurosyphilis:
Treponema pallidum invasion
- Entry through mucous membranes or skin: Primary contact with the bacterium usually occurs through microtrauma on mucous membranes or skin during sexual contact.
- Spread through the body: Once invaded, T. Pallidum spreads rapidly through the bloodstream and lymphatic system, allowing it to reach the central nervous system (CNS). [5]
CNS penetration
- Early penetration: T. Pallidum is able to penetrate the CNS early in the infection, which can lead to asymptomatic neurosyphilis or early forms of symptomatic neurosyphilis. [6]
- Immune system bypass: The bacterium has unique mechanisms that allow it to avoid the host immune response, which favors its survival and multiplication in the CNS.
Inflammatory response
- Immune response: Infiltration of the CNS by T. Pallidum induces an immune response characterized by inflammation of the cerebral membranes, cerebral vessels and brain parenchyma.
- Gum formation: In the later stages of neurosyphilis, gumma formation, granulomatous nodules that can cause tissue destruction and CNS dysfunction, may occur.
CNS damage
- Meningovascular neurosyphilis: Inflammation of the blood vessels of the brain can lead to ischemia and strokes.
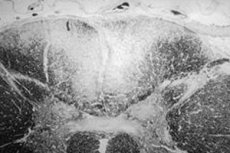
- Parenchymatous neurosyphilis (progressive paralysis and tabes dorsalis): Direct damage to nerve tissue by bacterium and inflammatory response leads to nerve cell degeneration, changes in brain parenchyma and spinal cord.
- Neurodegeneration: Chronic inflammation and damage to nerve tissue can lead to neurodegenerative changes similar to those in neurodegenerative diseases.
The impact of HIV
- Accelerated pathogenesis: Neurosyphilis may progress more rapidly in patients with HIV infection due to reduced immune defenses, which increases the risk of developing severe disease.
The pathogenesis of neurosyphilis is complex and involves interaction between the pathogen, the host immune system, and the neurologic system. Effective treatment requires timely detection and adequate antibiotic therapy to prevent further CNS damage.
Symptoms of the neurosyphilis
Neurosyphilis is categorized into early and late syphilis. Cerebrospinal fluid (CSF), cerebral membranes and vascular structures are affected in the early stages of neurosyphilis, and in the late stage; brain tissue and spinal cord parenchyma are affected. Thus, neurosyphilis can present with many different symptoms.
Neurosyphilis can present with a variety of symptoms depending on the stage of the disease. Here are some typical symptoms based on recent research:
-
Neurological symptoms:
- Headache.
- Tinnitus (ringing in the ears).
- Visual impairment.
- Ataxia (impaired coordination of movements).
- Leg weakness.
- Anal incontinence (Chang et al., 2011).
-
Psychiatric and cognitive symptoms:
- Personality changes.
- Paranoid delusions.
- Auditory and visual hallucinations.
- Memory impairments and abstract thinking abilities (Crozatti et al., 2015; Kambe et al., 2013).
-
Symptoms of late neurosyphilis may include dementia, tabes dorsalis (lesions of the posterior columns of the spinal cord), general paralysis, sensory ataxia, or bowel/bladder dysfunction (Marra, 2009).
Specific diagnostic methods include serologic tests (RPR and TPPA tests) and cerebrospinal fluid (CSF) analysis to confirm the diagnosis of neurosyphilis. Treatment usually involves antibiotics such as benzylpenicillin, which can be successful in about 75% of cases (Chang et al., 2011).
It is important to note that neurosyphilis can mimic many psychiatric disorders and should be considered as a possible diagnosis in patients with unexpected psychiatric symptoms, especially with rapidly progressive cognitive decline (Sobhan et al., 2004).
Lenin had neurosyphilis
Information about the health of historical figures, including Vladimir Lenin, is often based on anecdotal evidence, conjecture, and speculation. Whether Lenin suffered from neurosyphilis is a matter of debate among historians and medical professionals. Some sources claim that Lenin had symptoms that could indicate the presence of neurosyphilis, including his serious health problems in the last years of his life, such as several strokes and partial paralysis.
However, there is little evidence for this, and many researchers dispute this theory, suggesting other causes for his medical problems, including possible poisoning, genetic diseases, or other neurological conditions. There are no official medical documents or conclusive evidence to support Lenin's diagnosis of neurosyphilis, and much of what is available is based on limited medical information and postmortem analysis of his health.
It is important to note that medical diagnoses of historical figures should be viewed with caution, especially when they are based on limited data and not supported by reliable medical records. Thus, any claims of Lenin's illnesses, including neurosyphilis, should be considered hypothetical and not conclusively confirmed.
Stages
Untreated syphilis develops in four stages: primary, secondary, latent and tertiary. Primary syphilis is characterized by a typical painless syphilitic ulcer, called a chancre, which appears in the area of inoculation after an incubation period lasting 2-3 weeks.Secondary syphilis appears weeks or months later in nearly 25% of untreated patients, and lymphadenopathy, gastrointestinal disturbances, and central nervous system changes are observed.At the end of the latent period, tertiary syphilis develops in 25% of untreated patients. Tertiary syphilis is seen 1-30 years after primary infection. This inflammatory disease slowly progresses as neurosyphilis or gummosis syphilis. [7], [8]
The stages of neurosyphilis are closely related to the general stages of syphilis because neurosyphilis can develop at any of these stages if Treponema pallidum infection penetrates the central nervous system. Here is a brief description of the stages of syphilis and the potential neurologic manifestations associated with them:
Primary syphilis
At this stage, a hard, painless ulcer (chancre) forms at the site of entry of the bacterium. In rare cases, primary syphilis may be accompanied by meningitis, which is an early form of neurosyphilis. [9]
Secondary syphilis
This stage is characterized by an extensive rash, mucosal lesions, and lymphadenopathy. Neurosyphilis at this stage may manifest as meningitis, meningovascular neurosyphilis, and early signs of parenchymatous neurosyphilis, such as mild cognitive impairment or behavioral changes.
Latent syphilis
At this stage, the infection does not manifest clinically, but the bacterium remains in the body. Neurosyphilis can still develop at this stage, often without obvious symptoms, making it difficult to diagnose without specific tests.
Tertiary syphilis
This is a late stage of the disease that may develop many years after the initial infection. Neurosyphilis at this stage may manifest as gummatous neurosyphilis, progressive paralysis (General's palsy), and tabes dorsalis.
It is important to note that neurosyphilis can develop at any stage of syphilis and does not always follow the progressive order of the stages of the overall disease. Early diagnosis and treatment of syphilis is critical to prevent the development of neurosyphilis and other serious complications.
Forms
Neurosyphilis can manifest itself in different forms, depending on the parts of the nervous system affected and the extent of the disease. Here are the main forms of neurosyphilis:
1. Asymptomatic neurosyphilis.
- This is the most common form, occurring before the development of symptomatic syphilis.
- Patients are unaware that they are affected and have no signs of neurologic disease.
- It is defined by the presence of cerebrospinal fluid abnormalities in a patient with serologic signs of syphilis but without neurologic symptoms.
- Before the advent of penicillin, the diagnosis of VNS was important in predicting prognosis and patient outcomes with respect to the neurologic sequelae of syphilis.
2. Meningovascular neurosyphilis
Meningovascular neurosyphilis is a rare form of early neurosyphilis that causes infectious arteritis and ischemic infarction. This condition can manifest in young patients with few cases of cerebral hemorrhage, especially in patients infected with HIV (Sekikawa & Hongo, 2023). Meningovascular neurosyphilis can be diagnosed based on clinical signs and blood and cerebrospinal fluid analysis. Magnetic resonance angiography may show irregularities of the basilar artery, which is characteristic of this condition (Gállego et al., 1994).
Interestingly, the incidence of meningovascular syphilis has increased (38.5% of all neurosyphilis cases), and ischemic stroke with a peculiar clinical presentation is a well-known complication of meningovascular syphilis (Pezzini et al., 2001). High-resolution vessel wall imaging (HR-VWI) is one of the techniques used to directly visualize the vessel wall. In a rare case of meningovascular neurosyphilis where vasculitis of intracranial arteries was evaluated using HR-VWI, the patient's symptoms gradually improved after treatment with intravenous penicillin G and oral antiplatelet agents (Inui et al., 2021).
Meningovascular neurosyphilis is a differential diagnosis in young patients with cerebral infarction, especially in patients infected with HIV. Correct and timely treatment can halt progression and possibly improve symptomatology. Diagnosis and monitoring of improvement can be monitored with intracranial arterial wall imaging using contrast-enhanced MRI (Pérez Barragán et al., 2017).
3. Parenchymatous neurosyphilis
Parenchymatous neurosyphilis is a form of neurosyphilis in which the parenchyma of the brain and spinal cord is affected. This form of the disease may manifest several years or even decades after the primary syphilis infection. Parenchymatous neurosyphilis falls into two main categories: progressive paralysis (General's palsy) and tabes dorsalis.
Progressive paralysis (General's palsy).
Progressive paralysis is the most severe form of parenchymatous neurosyphilis. It affects the brain and is characterized by a gradual deterioration of cognitive function, leading to dementia. Among the symptoms of progressive paralysis are:
- Mental changes including personality changes, loss of critical thinking, apathy or mania.
- Speech disorders such as stuttering, difficulty in formulating thoughts.
- Tremor of the hands and face, especially the characteristic "paralytic tremor".
- Movement disorders, weakness.
- Changes in vision, possibly the development of Argyll-Robertson syndrome, in which the pupil is unresponsive to light but the proximity response is preserved.
Tabes dorsalis
Tabes dorsalis affects the posterior columns of the spinal cord and the roots of the posterior nerves, resulting in degeneration of the nervous system. Symptoms of tabes dorsalis include:
- Severe pain in the legs, lower back, abdomen, which can be attack-like.
- Sensory disturbance, especially in the lower extremities, resulting in loss of sensation of pain and temperature.
- Ataxia - impaired coordination of movements, especially in the dark.
- Absence of knee and Achilles reflexes.
- Pelvic organ dysfunction.
- Development of arthropathy (joint destruction) due to loss of sensation.
Diagnosis of parenchymatous neurosyphilis includes serologic tests for syphilis, analysis of cerebrospinal fluid, and neurologic examination. Treatment usually consists of prolonged courses of antibiotics, predominantly intravenous penicillin. Early diagnosis and treatment can slow the progression of the disease, but damage to the nervous system that has already occurred is often irreversible.
4. Focal neurosyphilis.
- Damage to specific parts of the nervous system, which can result in focal neurological symptoms such as paralysis, visual impairment, hearing impairment, and so on.
5. Early neurosyphilis
Early neurosyphilis is an infection of the central nervous system by Treponema pallidum that can occur at any stage of syphilis, including the earliest stages. The early form of neurosyphilis mainly involves the cerebral membranes, cerebrospinal fluid, and vessels of the brain or spinal cord. Clinical manifestations may include asymptomatic neurosyphilis, acute syphilitic meningitis, meningovascular syphilis, and syphilis-associated uveitis, which may also accompany early neurosyphilis (Marra, 2009). The incidence of neurosyphilis is increased among patients infected with HIV, especially among men who have sex with men (MSM), making this group particularly vulnerable to developing early neurosyphilis (Flood et al., 1998).
Diagnosis of neurosyphilis requires clinical, serologic, and cerebrospinal fluid analysis, while treatment involves antibiotic therapy, usually intravenous penicillin. It is important to note that even with adequate therapy in the early stages of syphilis, neurosyphilis may develop in some patients, especially those living with HIV (Johns, Tierney, & Felsenstein, 1987).
Given the increase in syphilis cases in recent years, especially among HIV-infected MSM, syphilis prophylaxis and early diagnosis of neurosyphilis are critical to prevent the development and progression of this disease. It is important to thoroughly evaluate patients with syphilis for neurologic, ophthalmologic, and audiologic symptoms and signs, as well as a low threshold for diagnostic lumbar puncture to exclude the diagnosis of neurosyphilis to ensure adequate and timely treatment.
6. Late-onset neurosyphilis
Late neurosyphilis is a form of neurosyphilis that can occur at any stage of syphilis disease, including the earliest stages. Early forms of neurosyphilis mainly affect the brain membranes, cerebrospinal fluid, and blood vessels of the brain or spinal cord. Late forms of neurosyphilis predominantly affect the parenchyma of the brain and spinal cord. Uveitis and hearing loss associated with syphilis are most common in the early stages of the disease and may accompany early neurosyphilis. The treatment of eye disease and hearing loss associated with syphilis is the same as that of neurosyphilis. Neurosyphilis is more common in patients infected with HIV, and much of the recent literature concerns this at-risk group. This article provides a critical review of the recent literature on the diagnosis, clinical findings, risk factors, and management of neurosyphilis (Marra, 2009).
Cases of neurosyphilis in a population with high rates of co-infection with syphilis and HIV in San Francisco from 1985 to 1992 are described. Neurosyphilis was defined by the new cerebrospinal fluid reactivity VDRL; 117 patients with neurosyphilis were identified. The mean age was 39 years, 91% were male, 74 (63%) were white, and 75 (64%) were HIV-infected. Thirty-eight (33%) presented with early symptomatic neurosyphilis syndromes. Six (5%) had late neurosyphilis (Flood et al., 1998).
Cases of neurosyphilis with severe neuropsychiatric symptoms in uncompromised patients are presented, demonstrating that even with early antibiotic treatment it is possible to develop late forms of the disease, requiring careful choice of treatment and diagnosis in late stages (Jantzen et al., 2012).
These studies emphasize the need for awareness of late-onset neurosyphilis as a possible diagnosis in patients with an appropriate clinical presentation, especially in persons infected with HIV, and the importance of early diagnosis and treatment to prevent serious sequelae.
7. Latent neurosyphilis
Latent neurosyphilis is a form of syphilis that affects the central nervous system (CNS) without overt clinical symptoms. This condition can develop in people with latent syphilis, including those infected with HIV. It is important to note that neurosyphilis can develop at any stage of the disease, even in the early stages. Diagnosis and treatment of latent neurosyphilis requires careful attention, including analysis of cerebrospinal fluid (CSF) to confirm the diagnosis. Here are some key points from current research on this topic:
- A study showed that in HIV-infected patients with latent syphilis, the prevalence of confirmed neurosyphilis (Venereal Disease Research Laboratory (VDRL) reactive test in cerebrospinal fluid) was 9.1%. This emphasizes the need for careful screening and diagnosis of neurosyphilis in this group of patients (Holtom et al., 1992).
- Cases of neurosyphilis following treatment of latent syphilis with benzathinpenicillin have been described. This supports the data that standard doses of neither benzathinpenicillin nor procainpenicillin provide treponemicidal concentrations of penicillin in the CSF. Effective treatment of neurosyphilis can be achieved by the administration of intravenous benzylpenicillin (Jørgensen et al., 1986).
- The current clinical spectrum of neurosyphilis in patients without immunodeficiency includes meningovascular, meningeal, and general paralytic forms. Compared to the preantibiotic era, there is a decrease in the incidence of late forms of neurosyphilis, mainly tabes dorsalis. The nonspecific neuroimaging findings and better outcome for early forms emphasize the importance of early diagnosis and treatment (Conde-Sendín et al., 2004).
These studies emphasize the importance of careful monitoring and diagnosis of neurosyphilis, especially in patients with latent syphilis and those infected with HIV. Early detection and adequate treatment can prevent the development of serious and irreversible neurological sequelae.
8. Gummous neurosyphilis.
Gummose neurosyphilis is a form of tertiary syphilis characterized by slowly progressive inflammation and granuloma formation, ranging from microscopic lesions to large tumor-like masses. Although cutaneous, mucosal, and bony gummose lesions are not uncommon, neurosyphilis in the form of gummas is rare. The use of F18-2-fluoro-2-deoxy-D-glucose (FDG) positron emission tomography (PET) is effective in assessing the metabolic activity of brain masses, particularly for guiding biopsy and grading of gliomas. However, the inflammatory nature of lesions such as neurosyphilitic gummas poses challenges to diagnostic modalities including CT, MRI, and PET. Because FDG is not a specific marker for malignancy, neurosyphilitic gumma may mimic a high-grade glioma by showing intense FDG uptake, which is a potential diagnostic error (Lin et al., 2009).
A case of gummatous neurosyphilis lesion of the third cranial nerve, confirmed by MR findings, has also been described. A 44-year-old woman presented with double vision and right-sided headaches. MRI showed contrast enhanced lesions of the upper brainstem and third cranial nerve. Serologic tests and lumbar puncture revealed the presence of active syphilis. After intravenous penicillin G treatment, control MRIs showed a reduction in lesion size with complete resolution within 3 months (Vogl et al., 1993).
Diagnosis and treatment of neurosyphilis in the form of gummas requires a comprehensive approach, including serologic testing, MRI and, in some cases, PET to assess the metabolic activity of the lesions. The need for early detection and adequate treatment is emphasized in these studies, as neurosyphilis can mimic other diseases and cause serious neurological complications.
Diagnostics of the neurosyphilis
Diagnosis of neurosyphilis is challenging, especially in patients infected with HIV. Detection of Treponema pallidum DNA in cerebrospinal fluid (CSF) by polymerase chain reaction (PCR) is an important aspect, although PCR does not always reliably detect neurosyphilis, even with the Venereal Disease Research Laboratory Reactive (VDRL) test for CSF (Marra et al., 1996). In addition, the diagnosis of neurosyphilis in HIV-infected patients with early syphilis involves evaluation of several laboratory tests, including Treponema pallidum particle agglutination (TPPA), fluorescent treponemal antibody absorbance (FTA-ABS), and INNO-LIA Syphilis linear immunoassay for analysis of CSF samples. Important predictors of neurosyphilis are headache, visual symptoms, CD4 count less than 500 cells/μL, and viremia as defined by HIV-1 RNA count ≥50 copies/mL (Dumaresq et al., 2013).
Despite the difficulties, the determination of serologic and CSF criteria remains key in the diagnosis of neurosyphilis. It is important to emphasize that the diagnosis of symptomatic neurosyphilis requires compliance with clinical, serologic, and SMW criteria, whereas serologic and SMW criteria are sufficient to diagnose asymptomatic neurosyphilis (Gonzalez et al., 2019). Neurosyphilis is more common in patients infected with HIV, and much of the current literature focuses on this at-risk group.
In patients with neurosyphilis, cerebrospinal fluid (CSF) is often abnormal with both pleocytosis and elevated protein concentrations.The Venereal Disease Research Laboratory (VDRL) cerebrospinal fluid assay is generally considered the gold standard for specificity but is recognized to have limited sensitivity. [10], [11]
Other cerebrospinal fluid tests including serologic assays such as rapid plasma reagin (RPR) [12], fluorescent treponemal antibody adsorption (FTA-ABS) [13] and Treponema pallidum hemagglutination assay[14] and molecular assays including PCR [15] have all been evaluated for cerebrospinal fluid and have varying specificity and sensitivity for the diagnosis of neurosyphilis.
In the setting of antibiotics and HIV co-infection, the clinical manifestations of neurosyphilis can be varied, making diagnosis particularly challenging. The advanced stage of the disease may be irreversible, so early detection and treatment are ideal. It is also important to consider the need for neuropenetrative antibiotics in treatment (Hobbs et al., 2018).
These data emphasize the need for high suspicion of neurosyphilis and routine serologic screening in patients with neurologic and psychiatric symptoms, especially in individuals [16] infected with HIV.
Puncture for neurosyphilis
Lumbar puncture (LP) plays a key role in the diagnosis of neurosyphilis, especially in patients with HIV infection and syphilis without neurologic symptoms. A study by Ghanem et al. (2009) showed that criteria based on rapid plasma reagin (RPR) titer and CD4 cell count, instead of criteria based on disease stage, improved the ability to identify asymptomatic neurosyphilis. Certain criteria, such as LP in patients with late latent syphilis or syphilis of unknown duration, regardless of CD4 cell count or RPR titer, may improve the diagnosis of asymptomatic neurosyphilis (Ghanem et al., 2009).
Libois et al. (2007) found that neurologic manifestations and serum RPR were associated with neurosyphilis. In multivariate analysis, log2RPR remained associated with neurosyphilis. In patients without neurologic manifestations, the risk of neurosyphilis increased progressively with increasing log2RPR. A serum RPR of 1/32 was identified as the best cut-off point for deciding whether to perform LP (sensitivity 100%, specificity 40%) (Libois et al., 2007).
These studies emphasize the need for LP to diagnose neurosyphilis, especially in patients with HIV infection and syphilis, even if they have no neurologic symptoms. Defining accurate criteria for performing LP may help in identifying asymptomatic neurosyphilis and preventing subsequent neurologic complications. [17]
Patients should be followed up after treatment at 3, 6, 9, 12 and 24 months with serial nontreponemal tests. A 4-fold decrease in these parameters indicates successful treatment. [18]
Differential diagnosis
The differential diagnosis of neurosyphilis includes consideration of a number of diseases whose symptoms and manifestations may overlap with those of neurosyphilis. This is necessary in order to make an accurate diagnosis and prescribe adequate treatment. Here are some of the conditions and diseases that should be considered in the differential diagnosis of neurosyphilis:
1. Viral encephalitis and meningitis
These conditions may have a similar clinical presentation to meningovascular neurosyphilis, including headaches, fever, impaired consciousness, and meningeal signs.
2. Multiple sclerosis (MS)
MS can mimic neurosyphilis by neurologic symptoms such as visual disturbances, ataxia, paresthesias, and weakness in the extremities.
3. Neurological manifestations of HIV infection
Especially in the late stages of HIV infection, when HIV-associated dementia or HIV encephalopathy may develop, the symptoms of which may resemble neurosyphilis.
4. Lyme disease (neuroborreliosis)
This disease, caused by Borrelia transmitted by ticks, can also manifest with meningitis, radiculoneuritis, and other neurologic symptoms.
5. Neurosyphilis in patients with latent syphilis
It is necessary to distinguish neurosyphilis from latent syphilis, in which antibodies to the pathogen are found in the patient's blood, but neurologic symptoms are absent.
6. Tuberculous meningitis
Characterized by chronic meningitis with lesions of the cerebral membranes, it can mimic meningovascular neurosyphilis.
7. Primary and metastatic brain tumors
Tumors may cause localized neurologic symptoms and behavioral changes, resembling some forms of neurosyphilis.
Methods of differential diagnosis:
Serologic tests for syphilis (such as RPR and TPHA), cerebrospinal fluid analysis, brain MRI, and specific tests to rule out other diseases (e.g., HIV tests, borreliosis testing) are used for differential diagnosis.
Thorough history taking, clinical examination and comprehensive examination allow to establish an accurate diagnosis and choose an appropriate treatment strategy.
Treatment of the neurosyphilis
Treatment of neurosyphilis usually involves antibiotic therapy, primarily intravenous penicillin, which is the antibiotic of choice for this disease. Recommendations may vary depending on regional protocols and individual patient characteristics, but general treatment guidelines include the following:
- Intravenous penicillin G: The standard treatment regimen includes intravenous penicillin G at high doses. For example, one commonly used regimen involves administering 18-24 million units of penicillin G per day, divided into 3-4 million units every 4 hours for 10-14 days. The exact dosage and duration of treatment may vary.
- Other antibiotics: For patients who are allergic to penicillin, alternative regimens including doxycycline or ceftriaxone may be considered, although penicillin remains the preferred option due to its high efficacy.
- Surveillance and follow-up evaluation: Serologic tests should be performed regularly after treatment to monitor response to therapy. This may include repeat blood and cerebrospinal fluid tests at intervals after treatment has been completed.
- Treatment of sexual partners: It is also important to ensure that the patient's sexual partners are examined and, if necessary, treated to prevent the spread of infection.
- HIV-infected patients: Patients with co-infection of HIV and syphilis may require special treatment recommendations and longer follow-up because HIV may affect the progression and treatment of syphilis.
Early detection and adequate treatment of neurosyphilis is critical to prevent long-term neurologic damage and improve patient outcomes. Consultation with an infectious disease or STD specialist is always recommended to determine the best treatment plan.
Clinical Guidelines
Highlights from the German guidelines for the diagnosis and treatment of neurosyphilis published by the German Society for Neurology (DGN) that may be useful in understanding approaches to the management of this disease:
- Diagnostic Criteria: Probable neurosyphilis can be diagnosed based on the presence of:
- Subacute or chronic neuropsychiatric symptoms.
- Increased cell counts in cerebrospinal fluid (CSF) or evidence of blood-CSF barrier disruption.
- Positive effect of antibiotic therapy against neurosyphilis on clinical course and CSF findings.
- A positive serum TPHA/TPPA or FTA test.
- Treatment recommendations: Intravenous penicillin or ceftriaxone for 14 days is recommended for the treatment of neurosyphilis. Clinical data, serum VDRL titer, and CSF cell counts should be used as indicators of therapeutic effect.
- Assessment of therapeutic effect: Normalization of serum rapid plasma reagin (RPR) titer can accurately predict treatment success in most cases, potentially avoiding the need for subsequent lumbar puncture in certain cases. However, it may be less accurate in predicting treatment success in patients infected with HIV who are not receiving antiretroviral therapy compared with those who are.
For more detailed recommendations and clinical management strategies, the full text of the guidelines should be consulted. Russia may also have its own national guidelines for the treatment of neurosyphilis, available through professional medical societies or on health care websites.
Forecast
The prognosis of neurosyphilis depends on several factors, including the stage of disease at the time of treatment initiation, the presence of co-infections (e.g., HIV), and the timeliness and adequacy of therapy. In general, early diagnosis and adequate treatment can significantly improve prognosis.
With early treatment.
- Early detection and treatment of neurosyphilis, especially in the asymptomatic or early symptomatic stage, usually results in complete cure or significant improvement in clinical symptoms.
- Recovery from treatment can be complete, but some patients may experience residual symptoms, especially if treatment is initiated late in the disease process.
With late treatment.
- Late initiation of treatment can lead to irreversible neurological damage, including dementia, personality changes, visual and auditory impairment, coordination and movement disorders. In such cases, the prognosis becomes less favorable.
- Tabes dorsalis and progressive paralysis are forms of late neurosyphilis that are difficult to treat and patients are often left with significant limitations.
HIV infection and neurosyphilis
- Patients with HIV and neurosyphilis may have a more severe course of disease and a worse prognosis due to immunosuppression. In such cases, careful medical monitoring and aggressive antibiotic therapy are important.
Importance of monitoring
- Regular monitoring of patients after treatment is necessary to assess the efficacy of therapy and early detection of possible relapses.
In general, the prognosis in neurosyphilis improves with early diagnosis and initiation of treatment. However, even with timely treatment, some forms of neurosyphilis can leave lasting or permanent neurologic sequelae.
List of studies related to the study of neurosyphilis
- "Neurosyphilis" - Authors: Hemil Gonzalez, I. Koralnik, C. Marra (2019). This article reviews the clinical presentation, diagnosis and treatment of neurosyphilis, and discusses the role of lumbar puncture in the early stages of infection.
- "Update on neurosyphilis" - By C. Marra (2009). This article provides a critical review of recent research on the diagnosis, clinical manifestations, risk factors and management of neurosyphilis.
- "Neurosyphilis and the impact of HIV infection.". - Authors: E Ho, S Spudich (2015). A review of the clinical presentation, diagnostic laboratory findings, treatment and management of neurosyphilis, with a focus on the impact of HIV infection.
- "Neurosyphilis in patients with HIV" - By E. Hobbs, J. Vera, M. Marks, A. Barritt, B. Ridha, David S. Lawrence (2018). A review of complications of syphilis, especially neurosyphilis, in patients with HIV.
- "An Updated Review of Recent Advances in Neurosyphilis" - Authors: Jia Zhou, Hanlin Zhang, K. Tang, Runzhu Liu, Jun Yu Li (2022). An up-to-date review of neurosyphilis, including epidemiology, clinical manifestations, laboratory findings, comorbidities, diagnosis, treatment, prognosis, and major studies.
Literature
- Butov, Y. S. Dermatovenerology. National guide. Brief edition / edited by Y. S. Butov, Y. K. Skripkin, O. L. Ivanov. - Moscow: GEOTAR-Media, 2020.

