Medical expert of the article
New publications
Needle electromyography
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Needle electromyography includes the following main methods:
- standard needle EMG;
- Single muscle fiber EMG;
- macroEMG;
- scanning EMG.
Standard needle electromyography
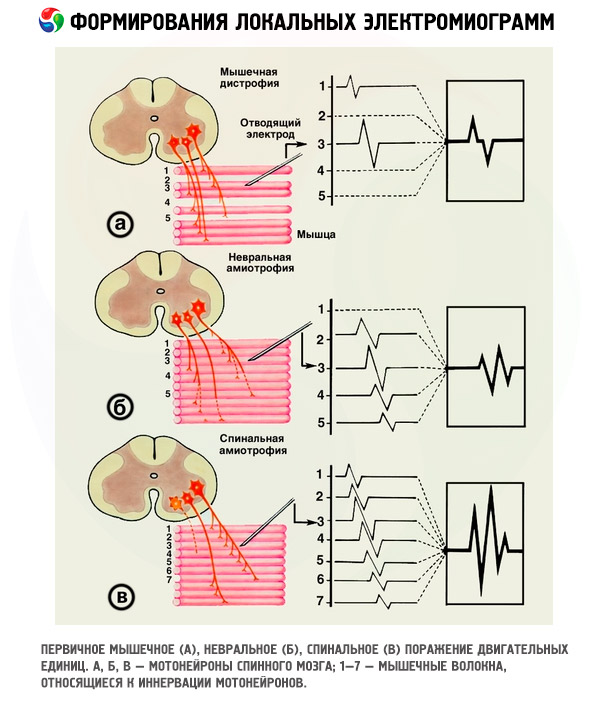
Needle electromyography is an invasive method of examination, carried out with the help of a concentric needle electrode inserted into the muscle. Needle electromyography allows to evaluate the peripheral neuromotor apparatus: morphofunctional organization of skeletal muscle motor units, the state of muscle fibers (their spontaneous activity), and in case of dynamic observation - to evaluate the effectiveness of treatment, the dynamics of the pathological process and the prognosis of the disease.
Diagnostic value
Standard needle electromyography occupies a central place among electrophysiological research methods in various neuromuscular diseases and is of decisive importance in the differential diagnosis of neurogenic and primary muscular diseases.
This method is used to determine the severity of denervation in the muscle innervated by the affected nerve, the degree of its recovery, and the effectiveness of reinnervation.
Needle electromyography has found its application not only in neurology, but also in rheumatology, endocrinology, sports and occupational medicine, pediatrics, urology, gynecology, surgery and neurosurgery, ophthalmology, dentistry and maxillofacial surgery, orthopedics and a number of other medical fields.
Indications for the procedure
Diseases of the spinal cord motor neurons ( ALS, spinal amyotrophies, poliomyelitis and post-polio syndrome, syringomyelia, etc.), myelopathies, radiculopathies, various neuropathies (axonal and demyelinating), myopathies, inflammatory muscle diseases ( polymyositis and dermatomyositis ), central movement disorders, sphincter disorders and a number of other situations when it is necessary to objectify the state of motor functions and the movement control system, to assess the involvement of various structures of the peripheral neuromotor apparatus in the process.
 [ 6 ]
[ 6 ]
Preparation
The patient does not need any special preparation for the examination. Needle electromyography requires complete relaxation of the muscles being examined, so it is performed with the patient lying down. The patient is exposed to the muscles being examined, laid on his back (or stomach) on a comfortable soft couch with an adjustable headrest, informed about the upcoming examination and explained how he should tense and then relax the muscle.
 [ 7 ]
[ 7 ]
Technique needle electromyography
The study is conducted using a concentric needle electrode inserted into the motor point of the muscle (the permissible radius is no more than 1 cm for large muscles and 0.5 cm for small ones). The potentials of the MU (PMU) are recorded. When choosing PMU for analysis, it is necessary to follow certain rules for their selection.
Reusable needle electrodes are pre-sterilized in an autoclave or by other sterilization methods. Disposable sterile needle electrodes are opened immediately before muscle examination.
After inserting the electrode into a completely relaxed muscle and each time it is moved, the possible appearance of spontaneous activity is monitored. The PMU is recorded with minimal voluntary muscle tension, allowing individual PMU to be identified. 20 different PMU are selected, observing a certain sequence of electrode movement in the muscle.
When assessing the muscle condition, a quantitative analysis of the spontaneous activity detected is performed, which is especially important when monitoring the patient's condition over time, as well as when determining the effectiveness of therapy. The parameters of the recorded potentials of various motor units are analyzed.
Needle electromyography in synaptic diseases
In synaptic diseases, needle electromyography is considered an additional method of examination. In myasthenia, it allows to assess the degree of "blocking" of muscle fibers in the MU, determined by the degree of decrease in the average duration of the MU in the examined muscles. However, the main goal of needle electromyography in myasthenia is to exclude possible concomitant pathology (polymyositis, myopathy, endocrine disorders, various polyneuropathies, etc.). Needle electromyography in patients with myasthenia is also used to determine the degree of response to the introduction of anticholinesterase drugs, that is, to assess the change in the MU parameters when neostigmine methyl sulfate (proserin) is administered. After the introduction of the drug, the duration of the MU in most cases increases. The absence of a reaction may indicate so-called myasthenic myopathy.
The main electromyographic criteria of synaptic diseases:
- reduction of the average duration of PDE;
- decrease in the amplitude of individual PMUs (may be absent);
- moderate polyphasia of the PDE (may be absent);
- absence of spontaneous activity or the presence of only isolated PF.
In myasthenia, the average duration of the MUAP is usually reduced slightly (by 10-35%). The majority of MUAPs have normal amplitude, but in each muscle several MUAPs of reduced amplitude and duration are recorded. The number of polyphasic MUAPs does not exceed 15-20%. Spontaneous activity is absent. If pronounced PF is detected in a patient, one should consider a combination of myasthenia with hypothyroidism, polymyositis or other diseases.
Needle electromyography in primary muscular diseases
Needle electromyography is the main electrophysiological method for diagnosing primary muscular diseases (various myopathies). Due to the decreased ability of the motor units to develop sufficient force to maintain even minimal effort, a patient with any primary muscular pathology has to recruit a large number of motor units. This determines the peculiarity of electromyography in such patients. With minimal voluntary muscle tension, it is difficult to isolate individual motor units; such a multitude of small potentials appears on the screen that it makes their identification impossible. This is the so-called myopathic pattern of electromyography.
In inflammatory myopathies (polymyositis), a reinnervation process occurs, which can cause an increase in the parameters of the MUAP.
The main electromyographic criteria of primary muscular diseases:
- reduction in the average duration of PDE by more than 12%;
- decrease in the amplitude of individual PMUs (the average amplitude can be either reduced or normal, and sometimes increased);
- polyphasia of PDE;
- pronounced spontaneous activity of muscle fibers in inflammatory myopathy (polymyositis) or PMD (in other cases it is minimal or absent).
A decrease in the average duration of the MUAP is a cardinal sign of any primary muscular disease. The reason for this change is that in myopathies, muscle fibers undergo atrophy, some of them fall out of the composition of the MU due to necrosis, which leads to a decrease in the MUAP parameters. A decrease in the duration of most MUAPs is detected in almost all muscles of patients with myopathies, although it is more pronounced in the clinically most affected proximal muscles.
The histogram of the distribution of PMU by duration shifts towards smaller values (stage I or II). The exception is PMD: due to the sharp polyphasia of PMU, sometimes reaching 100%, the average duration can be significantly increased.
Single muscle fiber electromyography
Single muscle fiber electromyography allows the study of the electrical activity of individual muscle fibers, including determining their density in muscle motor units and the reliability of neuromuscular transmission using the jitter method.
To conduct the study, a special electrode with a very small discharge surface of 25 µm in diameter, located on its lateral surface 3 mm from the end, is required. The small discharge surface allows recording the potentials of a single muscle fiber in a zone with a radius of 300 µm.
Muscle Fiber Density Study
The determination of the density of muscle fibers in the MU is based on the fact that the zone of the microelectrode for recording the activity of a single muscle fiber is strictly defined. The measure of the density of muscle fibers in the MU is the average number of potentials of single muscle fibers recorded in the zone of its recording during the study of 20 different MU in different zones of the muscle. Normally, this zone can contain only one (rarely two) muscle fiber belonging to the same MU. Using a special methodical technique (trigger device), it is possible to avoid the appearance on the screen of potentials of single muscle fibers belonging to other MU.
The average fiber density is measured in conventional units by calculating the average number of potentials of individual muscle fibers belonging to different MUs. In healthy people, this value varies depending on the muscle and age from 1.2 to 1.8. An increase in the density of muscle fibers in MUs reflects a change in the structure of MUs in the muscle.
Research into the jitter phenomenon
Normally, it is always possible to position the electrode for recording a single muscle fiber in a muscle so that the potentials of two adjacent muscle fibers belonging to one motor unit are recorded. If the potential of the first fiber is activated by the trigger device, the potential of the second fiber will slightly mismatch in time, since the impulse takes different times to pass through two nerve terminals of different lengths. This is reflected in the variability of the interpeak interval, i.e. the recording time of the second potential fluctuates in relation to the first, defined as the potential "dance" or "jitter", the value of which is normally 5-50 μs.
Jitter reflects the variability of neuromuscular transmission time in two motor end plates, so this method allows us to study the stability of neuromuscular transmission. When it is disrupted by any pathology, jitter increases. Its most pronounced increase is observed in synaptic diseases, primarily in myasthenia.
With a significant deterioration in neuromuscular transmission, a condition occurs when a nerve impulse cannot excite one of two adjacent fibers and so-called impulse blocking occurs.
A significant increase in jitter and instability of individual components of the PMU are also observed in ALS. This is explained by the fact that the terminals and immature synapses newly formed as a result of sprouting operate with an insufficient degree of reliability. In this case, the most pronounced jitter and impulse blocking are observed in patients with rapid progression of the process.
Macroelectromyography
Macroelectromyography allows us to judge the size of the motor units in skeletal muscles. Two needle electrodes are used simultaneously during the study: a special macroelectrode inserted deep into the muscle so that the abductor lateral surface of the electrode is in the thickness of the muscle, and a regular concentric electrode inserted under the skin. The macroelectromyography method is based on studying the potential recorded by a macroelectrode with a large abductor surface.
A conventional concentric electrode serves as a reference electrode, inserted under the skin at a distance of at least 30 cm from the main macroelectrode into the zone of minimal activity of the muscle being studied, that is, as far as possible from the motor point of the muscle.
Another electrode for recording potentials of single muscle fibers, mounted in the cannula, registers the potential of the muscle fiber of the studied MU, which serves as a trigger for averaging the macropotential. The signal from the cannula of the main electrode also enters the averager. 130-200 pulses are averaged (epoch of 80 ms, a period of 60 ms is used for analysis) until a stable isoline and a stable amplitude macropotential of the MU appear. Registration is carried out on two channels: on one, a signal from one muscle fiber of the studied MU is recorded, which triggers averaging, on the other, the signal between the main and reference electrodes is reproduced.
The main parameter used to evaluate the macropotential of the motor unit is its amplitude, measured from peak to peak. The duration of the potential is not important when using this method. It is possible to evaluate the area of the macropotentials of the motor unit. Normally, there is a wide range of values of its amplitude, with age it increases somewhat. In neurogenic diseases, the amplitude of the macropotentials of the motor unit increases depending on the degree of reinnervation in the muscle. In neuronal diseases, it is the highest.
In the late stages of the disease, the amplitude of the MU macropotentials decreases, especially with a significant decrease in muscle strength, which coincides with a decrease in the MU parameters recorded by standard needle electromyography.
In myopathies, a decrease in the amplitude of the macropotentials of the motor units is noted, however, in some patients their average values are normal, but nevertheless, a certain number of potentials of reduced amplitude are still noted. None of the studies that examined the muscles of patients with myopathy revealed an increase in the average amplitude of the macropotentials of the motor units.
The macroelectromyography method is very labor-intensive, so it has not become widely used in routine practice.
Scanning electromyography
The method allows studying the temporal and spatial distribution of the electrical activity of the motor unit by scanning, i.e. stepwise movement of the electrode in the area of the location of the fibers of the motor unit being studied. Scanning electromyography provides information on the spatial location of muscle fibers throughout the entire space of the motor unit and can indirectly indicate the presence of muscle groups that are formed as a result of the process of denervation of muscle fibers and their repeated reinnervation.
At minimum voluntary tension of the muscle, the electrode inserted into it for recording a single muscle fiber is used as a trigger, and with the help of the output concentric needle (scanning) electrode, the PMU is recorded from all sides in a diameter of 50 mm. The method is based on the slow step-by-step immersion of a standard needle electrode into the muscle, accumulation of information on the change in the parameters of the potential of a certain MU and the construction of a corresponding image on the monitor screen. Scanning electromyography is a series of oscillograms located one under the other, each of which reflects the oscillations of the biopotential recorded at a given point and captured by the output surface of the concentric needle electrode.
Subsequent computer analysis of all these MUAPs and analysis of their three-dimensional distribution provides insight into the electrophysiological profile of motor neurons.
When analyzing scanning electromyography data, the number of main peaks of the MUAP, their shift in time of appearance, the duration of intervals between the appearance of individual fractions of the potential of a given MU are assessed, and the diameter of the fiber distribution zone in each of the examined MUs is calculated.
In DRP, the amplitude and duration, as well as the area of potential oscillations on scanning electromyography, increase. However, the cross-section of the fiber distribution zone of individual DE does not change significantly. The number of fractions characteristic of a given muscle does not change either.
Contraindications to the procedure
There are practically no contraindications to needle electromyography. A limitation is considered to be the unconscious state of the patient, when he cannot voluntarily tense the muscle. However, even in this case it is possible to determine the presence or absence of the current process in the muscles (by the presence or absence of spontaneous activity of muscle fibers). Needle electromyography should be carried out with caution in those muscles that have pronounced purulent wounds, non-healing ulcers and deep burn lesions.
Normal performance
The DE is a structural and functional element of the skeletal muscle. It is formed by a motor neuron located in the anterior horn of the gray matter of the spinal cord, its axon emerging as a myelinated nerve fiber as part of the motor root, and a group of muscle fibers that form a contact with the numerous branches of this axon, deprived of the myelin sheath - terminals, using a synapse.
Each muscle fiber of a muscle has its own terminal, is part of only one motor unit, and has its own synapse. Axons begin to branch intensively at the level of several centimeters before the muscle to provide innervation of each muscle fiber that is part of this motor unit. The motor neuron generates a nerve impulse that is transmitted along the axon, is amplified in the synapse, and causes contraction of all muscle fibers belonging to this motor unit. The total bioelectric potential recorded during such contraction of muscle fibers is called the motor unit potential.
Motor unit potentials
An assessment of the state of the human skeletal muscle motor units is made based on an analysis of the parameters of the potentials they generate: duration, amplitude, and shape. Each motor unit is formed as a result of the algebraic addition of the potentials of all muscle fibers that make up the motor unit, which functions as a single entity.
When the excitation wave spreads along the muscle fibers towards the electrode, a three-phase potential appears on the monitor screen: the first deviation is positive, then there is a quick negative peak, and the potential ends with a third, again positive deviation. These phases can have different amplitudes, durations and areas, which depend on how the electrode's output surface is located in relation to the central part of the recorded DE.
The parameters of the PMU reflect the size of the DE, the quantity, mutual arrangement of muscle fibers and the density of their distribution in each specific DE.
Normal motor unit potential duration
The main parameter of the PDE is its duration, or length, measured as the time in milliseconds from the beginning of the signal deviation from the centerline until its complete return to it.
The duration of the PMU in a healthy person depends on the muscle and age. With age, the duration of the PMU increases. In order to create unified criteria for the norm in the study of the PMU, special tables of normal average values of duration for different muscles of people of different ages have been developed. A fragment of such tables is given below.
The measure of the assessment of the state of the MU in the muscle is the average duration of 20 different MUAPs recorded at different points of the muscle being studied. The average value obtained during the study is compared with the corresponding indicator presented in the table, and the deviation from the norm is calculated (in percent). The average duration of the MUAP is considered normal if it falls within the limits of ±12% of the value given in the table (abroad, the average duration of the MUAP is considered normal if it falls within the limits of ±20%).
 [ 14 ], [ 15 ], [ 16 ], [ 17 ]
[ 14 ], [ 15 ], [ 16 ], [ 17 ]
Duration of motor unit potentials in pathology
The main pattern of changes in the duration of the PDE in pathological conditions is that it increases in neurogenic diseases and decreases in synaptic and primary muscular pathology.
In order to more thoroughly assess the degree of change in the PMU in muscles with various lesions of the peripheral neuromotor apparatus, a histogram of the PMU distribution by duration is used for each muscle, since their average value can be within the limits of normal deviations with obvious muscle pathology. Normally, the histogram has the form of a normal distribution, the maximum of which coincides with the average duration of the PMU for a given muscle. With any pathology of the peripheral neuromotor apparatus, the shape of the histogram changes significantly.
Electromyographic stages of the pathological process
Based on the change in the duration of the MU in diseases of the motor neurons of the spinal cord, when all changes occurring in the muscles can be traced in a relatively short period of time, six EMG stages have been identified that reflect the general patterns of the restructuring of the MU during the denervation-reinnervation process (DRP), from the very onset of the disease to the almost complete death of the muscle.
All neurogenic diseases are characterized by the death of a greater or lesser number of motor neurons or their axons. The surviving motor neurons innervate the “foreign” muscle fibers deprived of nervous control, thereby increasing their number in their MU. On electromyography, this process is manifested by a gradual increase in the parameters of the potentials of such MU. The entire cycle of changes in the histogram of the distribution of MU by duration in neuronal diseases is conventionally divided into five EMG stages, reflecting the process of compensatory innervation in muscles. Although such a division is conventional, it helps to understand and trace all the stages of the development of DRP in each specific muscle, since each stage reflects a certain phase of reinnervation and the degree of its severity. It is inappropriate to present stage VI as a histogram, since it reflects the final point of the “reverse” process, that is, the process of decompensation and destruction of the muscle MU.
Among specialists in our country, these stages have become widespread in the diagnosis of various neuromuscular diseases. They are included in the computer program of domestic electromyographs, which allows for the automatic construction of histograms indicating the stage of the process. A change in the stage in one direction or another during a repeated examination of the patient shows what the further prospects for the development of DRP are.
- Stage I: the average duration of the MUAP is reduced by 13-20%. This stage reflects the very initial phase of the disease, when denervation has already begun, and the process of reinnervation is not yet manifested electromyographically. Some denervated muscle fibers, deprived of impulse influence due to pathology of either the motor neuron or its axon, fall out of the composition of some MU. The number of muscle fibers in such MUAPs decreases, which leads to a decrease in the duration of individual potentials. In stage I, a certain number of narrower potentials than in healthy muscle appear, which causes a slight decrease in the average duration. The histogram of the MUAP distribution begins to shift to the left, towards smaller values.
- Stage II: the average duration of the MUAP is reduced by 21% or more. In DRP, this stage is observed extremely rarely and only in cases where, for some reason, reinnervation does not occur or is suppressed by some factor (e.g., alcohol, radiation, etc.), while denervation, on the contrary, increases and massive death of muscle fibers in the MUAP occurs. This leads to the fact that most or almost all MUAPs become shorter in duration than normal, due to which the average duration continues to decrease. The MUAP distribution histogram shifts significantly towards smaller values. Stages I-II reflect changes in the MUAPs caused by a decrease in the number of functioning muscle fibers in them.
- Stage III: the average duration of the MUAP is within ±20% of the norm for a given muscle. This stage is characterized by the appearance of a certain number of potentials of increased duration, normally undetectable. The appearance of these MUAPs indicates the onset of reinnervation, i.e. denervated muscle fibers begin to be included in other MUAPs, due to which the parameters of their potentials increase. In the muscle, MUAPs of both decreased and normal, as well as increased duration are simultaneously recorded, the number of enlarged MUAPs in the muscle varies from one to several. The average duration of the MUAP in stage III may be normal, but the appearance of the histogram differs from the norm. It does not have the shape of a normal distribution, but is “flattened”, stretched and begins to shift to the right, towards larger values. It is proposed to divide stage III into two subgroups - IIIA and IIIB. They differ only in that at stage IIIA the average duration of the MUAP is reduced by 1-20%, and at stage IIIB it either completely coincides with the average value of the norm, or is increased by 1-20%. At stage IIIB, a slightly larger number of MUAPs of increased duration are recorded than at stage IIIA. Practice has shown that such a division of the third stage into two subgroups does not have much significance. In fact, stage III simply means the appearance of the first EMG signs of reinnervation in the muscle.
- Stage IV: the average duration of the MUAP is increased by 21-40%. This stage is characterized by an increase in the average duration of the MUAP due to the appearance, along with normal MUAPs, of a large number of potentials of increased duration. MUAPs of reduced duration are recorded extremely rarely at this stage. The histogram is shifted to the right, towards larger values, its shape is different and depends on the ratio of MUAPs of normal and increased duration.
- Stage V: the average duration of the MUAP is increased by 41% or more. This stage is characterized by the presence of predominantly large and "giant" MUAPs, while MUAPs of normal duration are practically absent. The histogram is significantly shifted to the right, stretched and, as a rule, open. This stage reflects the maximum volume of reinnervation in the muscle, as well as its effectiveness: the more giant MUAPs, the more effective the reinnervation.
- Stage VI: the average duration of the MUAP is within normal limits or is reduced by more than 12%. This stage is characterized by the presence of MUAPs (potentials of deteriorating MUs) that are altered in shape. Their parameters may formally be normal or reduced, but the shape of the MUAPs is altered: the potentials do not have sharp peaks, are stretched, rounded, the potential rise time is sharply increased. This stage is observed at the last stage of decompensation of the DRP, when most of the motor neurons of the spinal cord have already died and the rest are intensively dying. Decompensation of the process begins from the moment when the denervation process increases, and the sources of innervation become fewer and fewer. On the EMG, the decompensation stage is characterized by the following signs: MUAP parameters begin to decrease, giant MUAPs gradually disappear, the intensity of the PF increases sharply, giant POWs appear, which indicates the death of many adjacent muscle fibers. These signs indicate that in this muscle the motor neurons have exhausted their sprouting capabilities as a result of functional inadequacy and are no longer capable of fully controlling their fibers. As a result, the number of muscle fibers in the motor unit progressively decreases, the impulse conduction mechanisms are disrupted, the potentials of such motor units are rounded, their amplitude decreases, and their duration decreases. Plotting a histogram at this stage of the process is inappropriate, since it, as well as the average duration of the PMU, no longer reflects the true state of the muscle. The main sign of stage VI is a change in the shape of all PMUs.
EMG stages are used not only for neurogenic diseases, but also for various primary muscular diseases, to characterize the depth of muscle pathology. In this case, the EMG stage reflects not the DRP, but the severity of the pathology and is called the "EMG stage of the pathological process". In primary muscular dystrophies, sharply polyphasic PMUs with satellites that increase their duration may appear, which significantly increases its average value, corresponding to III or even IV EMG stage of the pathological process.
Diagnostic significance of EMG stages
- In neuronal diseases, different EMG stages are often detected in different muscles in the same patient - stages III to VI are detected very rarely - at the very beginning of the disease, and only in individual muscles.
- In axonal and demyelinating diseases, stages III and IV are most often detected, and stages I and II are less common. Stage V is detected when a significant number of axons die in individual, most affected muscles.
- In primary muscular diseases, there is a loss of muscle fibers from the composition of the MU due to some muscle pathology: a decrease in the diameter of muscle fibers, their splitting, fragmentation or other damage that reduces the number of muscle fibers in the MU or reduces the volume of the muscle. All this leads to a decrease (shortening) in the duration of the PMU. Therefore, in most primary muscular diseases and myasthenia, stages I and II are detected, in polymyositis - at first only I and I, and upon recovery - III and even IV stages.
Motor unit potential amplitude
Amplitude is an auxiliary but very important parameter in the analysis of the MUAP. It is measured "from peak to peak", that is, from the lowest point of the positive to the highest point of the negative peak. When registering MUAP on the screen, their amplitude is determined automatically. Both the average and maximum amplitude of the MUAP detected in the muscle being studied are determined.
The average values of the MUAP amplitude in the proximal muscles of healthy people in most cases are 500-600 μV, in the distal muscles - 600-800 μV, while the maximum amplitude does not exceed 1500-1700 μV. These indicators are very conditional and can vary to some extent. In children aged 8-12 years, the average MUAP amplitude, as a rule, is within 300-400 μV, and the maximum does not exceed 800 μV; in older children, these indicators are 500 and 1000 μV, respectively. In the facial muscles, the MUAP amplitude is significantly lower.
In athletes, an increased amplitude of the MUAP is recorded in trained muscles. Consequently, an increase in the average amplitude of the MUAP in the muscles of healthy individuals involved in sports cannot be considered a pathology, since it occurs as a result of the restructuring of the MU due to prolonged load on the muscles.
In all neurogenic diseases, the amplitude of the PMU, as a rule, increases in accordance with the increase in duration: the longer the duration of the potential, the higher its amplitude.
The most significant increase in the amplitude of the MUAP is observed in neuronal diseases, such as spinal amyotrophy and the consequences of poliomyelitis. It serves as an additional criterion for diagnosing the neurogenic nature of pathology in muscles. The increase in the amplitude of the MUAP is caused by the reorganization of the MU in the muscle, an increase in the number of muscle fibers in the electrode lead zone, synchronization of their activity, and an increase in the diameter of muscle fibers.
An increase in both the average and maximum amplitude of the MUAP is sometimes observed in some primary muscular diseases, such as polymyositis, primary muscular dystrophy, dystrophic myotonia, etc.
Motor unit potential waveform
The shape of the PDE depends on the structure of the DE, the degree of synchronization of the potentials of its muscle fibers, the position of the electrode in relation to the muscle fibers of the analyzed DE and their innervation zones. The shape of the potential has no diagnostic value.
In clinical practice, the shape of the MUAP is analyzed in terms of the number of phases and/or turns in the potential. Each positive-negative potential deviation that reaches the isoline and crosses it is called a phase, and a positive-negative potential deviation that does not reach the isoline is called a turn.
A potential is considered polyphase if it has five or more phases and crosses the axial line at least four times. The potential may have additional turns that do not cross the axial line. Turns can be in both the negative and positive parts of the potential.
In the muscles of healthy people, the MUAPs are usually represented by three-phase potential oscillations, however, when recording the MUAP in the end plate zone, it can have two phases, losing its initial positive part.
Normally, the number of polyphasic MUAPs does not exceed 5-15%. An increase in the number of polyphasic MUAPs is considered a sign of a disorder in the structure of the MU due to the presence of some pathological process. Polyphasic and pseudopolyphasic MUAPs are recorded in both neuronal and axonal diseases, as well as in primary muscular diseases.
 [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ]
[ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ]
Spontaneous activity
Under normal conditions, when the electrode is stationary in a relaxed muscle of a healthy person, no electrical activity occurs. In pathology, spontaneous activity of muscle fibers or DE appears. Spontaneous activity does not depend on the patient's will, he cannot stop it or cause it arbitrarily.
Spontaneous activity of muscle fibers
Spontaneous activity of muscle fibers includes fibrillation potentials (FP) and positive sharp waves (PSW). FP and PSB are recorded exclusively under pathological conditions when a concentric needle electrode is inserted into the muscle. FP is the potential of one muscle fiber, PSB is a slow oscillation that occurs after a rapid positive deflection, without a sharp negative peak. PSB reflects the participation of both one and several adjacent fibers.
The study of spontaneous activity of muscle fibers in the conditions of a clinical examination of a patient is the most convenient electrophysiological method, allowing one to judge the degree of completeness and stability of nerve influences on muscle fibers of a skeletal muscle in its pathology.
Spontaneous activity of muscle fibers may occur in any pathology of the peripheral neuromotor apparatus. In neurogenic diseases, as well as in synapse pathology (myasthenia and myasthenic syndromes), spontaneous activity of muscle fibers reflects the process of their denervation. In most primary muscle diseases, spontaneous activity of muscle fibers reflects some damage to muscle fibers (their splitting, fragmentation, etc.), as well as their pathology caused by the inflammatory process (in inflammatory myopathies - polymyositis, dermatomyositis). In both cases, PF and POV indicate the presence of an ongoing process in the muscle; normally, they are never recorded.
- The duration of PF is 1-5 ms (it has no diagnostic value), and the amplitude fluctuates within very wide limits (on average 118±114 μV). Sometimes high-amplitude (up to 2000 μV) PF are also detected, usually in patients with chronic diseases. The timing of the appearance of PF depends on the location of the nerve lesion. In most cases, they occur 7-20 days after denervation.
- If for some reason the reinnervation of the denervated muscle fiber does not occur, it dies over time, generating POWs, which are considered by EMG to be a sign of the death of the denervated muscle fiber that did not receive the innervation it had previously lost. The number of PFs and POWs recorded in each muscle can be used to indirectly judge the degree and depth of its denervation or the volume of dead muscle fibers. The duration of the POW is from 1.5 to 70 ms (in most cases up to 10 ms). The so-called giant POWs lasting more than 20 ms are detected with prolonged denervation of a large number of adjacent muscle fibers, as well as with polymyositis. The amplitude of the POW usually fluctuates between 10 and 1800 μV. POWs of large amplitude and duration are more often detected in later stages of denervation ("giant" POWs). POVs are first recorded 16-30 days after the first appearance of PF; they can persist in the muscle for several years after denervation. As a rule, POVs are detected later in patients with inflammatory lesions of the peripheral nerves than in patients with traumatic lesions.
PF and POV respond most quickly to the start of therapy: if it is effective, the severity of PF and POV decreases after 2 weeks. On the contrary, if the treatment is ineffective or insufficiently effective, their severity increases, which allows using the analysis of PF and POV as an indicator of the effectiveness of the drugs used.
Myotonic and pseudomyotonic discharges
Myotonic and pseudomyotonic discharges, or high-frequency discharges, also refer to spontaneous activity of muscle fibers. Myotonic and pseudomyotonic discharges differ in a number of features, the main one being the high repeatability of the elements that make up the discharge, i.e. the high frequency of potentials in the discharge. The term "pseudomyotonic discharge" is increasingly being replaced by the term "high-frequency discharge".
- Myotonic discharges are a phenomenon detected in patients with various forms of myotonia. When listening to it, it resembles the sound of a "dive bomber". On the monitor screen, these discharges look like repeating potentials of gradually decreasing amplitude, with progressively increasing intervals (which causes a decrease in the pitch of the sound). Myotonic discharges are sometimes observed in some forms of endocrine pathology (for example, hypothyroidism). Myotonic discharges occur either spontaneously or after a slight contraction or mechanical irritation of the muscle with a needle electrode inserted into it or by simply tapping on the muscle.
- Pseudomyotonic discharges (high-frequency discharges) are recorded in some neuromuscular diseases, both associated and not associated with denervation of muscle fibers. They are considered to be a consequence of ephaptic transmission of excitation with a decrease in the insulating properties of the membrane of muscle fibers, creating a prerequisite for the spread of excitation from one fiber to the adjacent one: the pacemaker of one of the fibers sets the rhythm of impulses, which is imposed on the adjacent fibers, which causes the unique shape of the complexes. Discharges begin and stop suddenly. Their main difference from myotonic discharges is the absence of a drop in the amplitude of the components. Pseudomyotonic discharges are observed in various forms of myopathy, polymyositis, denervation syndromes (in the late stages of reinnervation), spinal and neural amyotrophies (Charcot-Marie-Tooth disease), endocrine pathology, injuries or compression of the nerve and some other diseases.
Spontaneous motor unit activity
Spontaneous activity of the motor unit is represented by fasciculation potentials. Fasciculations are spontaneous contractions of the entire motor unit that occur in a completely relaxed muscle. Their occurrence is associated with motor neuron diseases, its overload with muscle fibers, irritation of any of its sections, and functional and morphological restructuring.
The appearance of multiple fasciculation potentials in muscles is considered one of the main signs of damage to spinal cord motor neurons. An exception is "benign" fasciculation potentials, sometimes detected in patients who complain of constant twitching in muscles, but do not note muscle weakness or other symptoms.
Single fasciculation potentials can also be detected in neurogenic and even primary muscular diseases, such as myotonia, polymyositis, endocrine, metabolic and mitochondrial myopathies.
Fasciculation potentials have been described that occur in highly skilled athletes after exhausting physical exercise. They can also occur in healthy but easily excitable people, in patients with tunnel syndromes, polyneuropathies, and in the elderly. However, unlike motor neuron diseases, their number in the muscle is very small, and the parameters are usually normal.
The parameters of fasciculation potentials (amplitude and duration) correspond to the parameters of the MUAP recorded in a given muscle and can change in parallel with changes in the MUAP during the development of the disease.
Needle electromyography in diagnostics of diseases of motor neurons of the spinal cord and peripheral nerves
Any neurogenic pathology is accompanied by DRP, the severity of which depends on the degree of damage to the innervation sources and on the level of the peripheral neuromotor apparatus - neuronal or axonal - at which the damage occurred. In both cases, the lost function is restored due to the surviving nerve fibers, and the latter begin to branch intensively, forming numerous shoots directed to the denervated muscle fibers. This branching has received the name "sprouting" in the literature.
There are two main types of sprouting - collateral and terminal. Collateral sprouting is the branching of axons in the area of the nodes of Ranvier, terminal sprouting is the branching of the final, unmyelinated section of the axon. It has been shown that the nature of sprouting depends on the nature of the factor that caused the disruption of nervous control. For example, with botulinum intoxication, branching occurs exclusively in the terminal zone, and with surgical denervation, both terminal and collateral sprouting occur.
In electromyography, these states of the MU at various stages of the reinnervation process are characterized by the appearance of MUAP of increased amplitude and duration. The exception is the very initial stages of the bulbar form of ALS, in which the MUAP parameters are within the limits of normal variations for several months.
Electromyographic criteria for diseases of spinal cord motor neurons
- The presence of pronounced fasciculation potentials (the main criterion for damage to spinal cord motor neurons).
- An increase in the parameters of the PDE and their polyphasy, reflecting the severity of the reinnervation process.
- The appearance of spontaneous activity of muscle fibers in the muscles - PF and POV, indicating the presence of an ongoing denervation process.
Fasciculation potentials are a mandatory electrophysiological sign of damage to spinal cord motor neurons. They are detected already in the earliest stages of the pathological process, even before the appearance of signs of denervation.
Since neuronal diseases imply a constant ongoing process of denervation and reinnervation, when a large number of motor neurons die and a corresponding number of MUs are destroyed at the same time, the MUs become increasingly larger, their duration and amplitude increase. The degree of increase depends on the duration and stage of the disease.
The severity of PF and POV depends on the severity of the pathological process and the degree of muscle denervation. In rapidly progressing diseases (for example, ALS), PF and POV are found in most muscles, in slowly progressing diseases (some forms of spinal amyotrophies) - only in half of the muscles, and in post-poliomyelitis syndrome - less than a third.
Electromyographic criteria for diseases of peripheral nerve axons
Needle electromyography in diagnostics of peripheral nerve diseases is an additional but necessary examination method that determines the degree of damage to the muscle innervated by the affected nerve. The study allows to clarify the presence of signs of denervation (SF), the degree of loss of muscle fibers in the muscle (the total number of MUFs and the presence of giant MUFs), the severity of reinnervation and its effectiveness (the degree of increase in the MUF parameters, the maximum amplitude of the MUF in the muscle).
The main electromyographic signs of the axonal process:
- increase in the average value of the amplitude of the PDE;
- the presence of PF and POV (with current denervation);
- increase in the duration of PDE (the average value may be within normal limits, i.e. ±12%);
- polyphasia of PDE;
- single fasciculation potentials (not in each muscle).
In case of damage to axons of peripheral nerves (various polyneuropathies), DRP also occurs, but its severity is much less than in neuronal diseases. Consequently, MUAPs are increased to a much lesser extent. Nevertheless, the basic rule of MUAP change in neurogenic diseases also applies to damage to axons of motor nerves (i.e., the degree of increase in MUAP parameters and their polyphasy depend on the degree of nerve damage and the severity of reinnervation). An exception is pathological conditions accompanied by rapid death of axons of motor nerves due to trauma (or some other pathological condition leading to the death of a large number of axons). In this case, the same giant MUAPs (with an amplitude of more than 5000 μV) appear as in neuronal diseases. Such MUAPs are observed in long-term forms of axonal pathology, CIDP, neural amyotrophies.
If in axonal polyneuropathies the amplitude of the MUAP increases first of all, then in the demyelinating process with deterioration of the functional state of the muscle (decrease in its strength) the average values of the MUAP duration gradually increase; significantly more often than in the axonal process, polyphasic MUAPs and fasciculation potentials are detected and less often - PF and POV.
 [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ]
[ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ]
Needle electromyography in diagnostics of synaptic and primary muscular diseases
Synaptic and primary muscular diseases typically have a decrease in the average duration of the MUAP. The degree of decrease in the duration of the MUAP correlates with the decrease in strength. In some cases, the MUAP parameters are within the normal range, and in PMD they can even be increased.

