Medical expert of the article
New publications
Mycoplasma chominis: what is it, how to treat?
Last reviewed: 03.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The intracellular microorganism, mycoplasma hominis, does not always cause disease, but sometimes provokes the development of such a pathology as mycoplasmosis. Pathogenic microbes often act as causative agents of infections and inflammatory reactions, in which healthy cells are damaged by both the microbes themselves and the toxic products of their vital activity.
Mycoplasma hominis can develop outside the cell, which makes it difficult for the immune system to detect it. The microorganism has a three-layer membrane, DNA, RNA, and has a pronounced effect on the immune system, causing respiratory and urogenital tract diseases.
Pathogenesis
The microorganism Mycoplasma hominis is a conditionally pathogenic microbe that can live in the body of even healthy people, and this is considered absolutely normal. That is, a person throughout his life may not suspect that his body contains mycoplasma, and the microbe does not cause any harm under normal conditions.

If certain conditions are created inside the body, under which the development and reproduction of mycoplasma accelerates, then in such a situation we can already talk about a deviation from the norm - namely, about the development of the disease. For this to happen, it is necessary to create certain conditions, which are facilitated by the following risk factors:
- weakened immunity;
- change in hormonal balance;
- chronic alcohol intoxication;
- chronic dysbacteriosis;
- post-infectious and post-operative conditions, exhaustion of the body.
Among other reasons for the increased pathogenicity of mycoplasma, the following can be distinguished:
- unsatisfactory social and living conditions, failure to comply with sanitary and hygienic standards;
- unprotected sexual intercourse with a patient with mycoplasmosis;
- frequent or chronic diseases of the urogenital system;
- promiscuous sexual intercourse;
- early sexual activity.
Mycoplasma hominis often appears in women:
- with promiscuous sexual life;
- with long-term use of hormonal or immunosuppressant drugs, antibiotics;
- after abortions, pregnancies;
- as a result of weakening of the immune system under the influence of stress;
- after chemotherapy and radiation treatment.
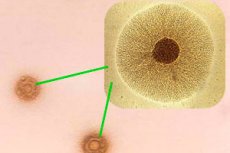
The microorganism Mycoplasma hominis is small in size and is surrounded by a cytoplasmic membrane.
Mycoplasma lacks a distinct cell wall, but shows a tendency toward polymorphism. Such features determine the microbe's relative resistance to antibiotic therapy.
When certain conditions optimal for mycoplasma are combined, the microbe begins to multiply rapidly, which entails the development of an infectious reaction. The number of mycoplasmas can reach 10 thousand/ml, or even more. In such a situation, male patients develop prostatitis, urethritis, epididymitis, and women develop inflammatory processes in the reproductive and urinary systems.
Mycoplasmas settle on eukaryotic membranes, which in case of pathology leads to the development of a local inflammatory reaction. Microbes "stick" to epithelial cells using receptors, change the functionality of cells and stimulate autoimmune reactions. As a result, hemostasis is disrupted, vascular endothelium is affected, platelet adhesion is observed, and DIC syndrome develops.
How is Mycoplasma hominis transmitted?
Mycoplasma hominis can be transmitted in several ways:
- Sexual transmission is possible through promiscuous unprotected sexual intercourse. In some cases, the patient may not even know that he or she is a carrier of the infection – but this does not exclude the possibility of infection.
- A child can become infected from the mother during childbirth if the mother is a carrier of mycoplasma.
- The household transmission mechanism involves the use of common personal hygiene items: for example, if several people, including the carrier of the infection, use the same towel.
The most common route of transmission of mycoplasma is considered to be sexual intercourse.
Epidemiology
Mycoplasma hominis is widely distributed in the natural environment: the microbe constantly resides inside living organisms. Mycoplasma hominis and genitalium live and develop in the genitourinary system, and under certain conditions cause the appearance of urogenital disease.
As of today, mycoplasma is diagnosed in 30-70% of women against the background of inflammatory genitourinary diseases, and in 20-40% of men.
The most common way of infection is unprotected sex.
 [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
[ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
Symptoms
Mycoplasma can cause an infectious disease with all the corresponding symptoms, or remain in a "dormant" state for a long time, without showing any signs. Clear first signs of the disease are detected only when the number of pathogenic microorganisms reaches 104-106 CFU/ml or more.
The incubation period of an infection caused by mycoplasma may vary. It depends on the following factors:
- from the number of microbes inside the body;
- from the degree of decreased immunity, the general condition of the body;
- depending on the location of the lesion - for example, with respiratory mycoplasmosis, the incubation period can be from several days to a month, and with damage to the genitourinary organs - from two to three weeks.
The first signs of mycoplasma damage to the respiratory system are manifested by the development of pharyngitis, nasopharyngitis, laryngopharyngitis, bronchitis - while the clinical picture corresponds to the listed pathologies. General signs of intoxication are usually moderate. This may be a slight increase in temperature, weakness, headache, a feeling of aches. Additional symptoms are dry cough, rhinitis. Visually, you can pay attention to conjunctivitis, submandibular and cervical lymphadenopathy, redness of the oropharynx. Auscultation in the lungs reveals wheezing and harsh breathing.
The clinical picture of urogenital mycoplasmosis should be considered separately for patients of different sexes.
Mycoplasma hominis in women manifests itself with signs of vaginitis, vaginosis, salpingo-oophoritis, thrush, endometritis, etc. The infection reveals itself with perineal itching, the presence of massive discharge with an unpleasant odor, a burning sensation at the end of urination or sexual intercourse, suprapubic pain. Adhesions, ectopic pregnancy, difficulties with conception, etc. may occur as secondary manifestations.
Mycoplasma hominis in men affects the mucous tissues of the prostate gland, urethra, kidneys. Characteristic signs may include:
- colorless small discharge in the morning;
- burning sensation in the urethra;
- pulling, painful sensations in the groin;
- swelling;
- problems with potency.
If the problem is not addressed in time, mycoplasma can lead to diseases such as prostatitis, urethritis, and male infertility caused by spermatogenesis disorders.
Secondary symptoms of mycoplasmosis may include unmotivated attacks of nausea and vomiting, and a slight increase in temperature.
Mycoplasma hominis in pregnant women
Increased reproduction of mycoplasma hominis in a woman's body during pregnancy can become a provoking factor for the development of premature labor, spontaneous abortion, uterine bleeding, and early placental abruption. Such troubles are related to the intrauterine inflammatory process.
If a newborn baby gets infected during labor, then the risk of developing meningitis or mycoplasma pneumonia increases. In advanced cases, the child may even die.
There is evidence that mycoplasma, which causes acute inflammation during pregnancy, can cause problems in the intrauterine development of the child - primarily due to intoxication and circulatory problems in the fetus.
Mycoplasma hominis in children
Babies become infected with mycoplasma mainly during childbirth if the mother is sick or a carrier of the infection. Mycoplasma hominis is often the primary cause of chorioamnionitis, postpartum infectious lesions, pyelonephritis - after all, during childbirth, microbes get not only on the skin, but also on the mucous membranes, into the respiratory organs and even into the stomach of the newborn.
The consequences of infection getting to the baby may be:
- inflammation of the walls of the ventricles of the brain ventriculitis;
- inflammation of the membranes of the brain - meningitis;
- abscesses (both external abscesses and those with brain damage);
- lymphadenitis, general intoxication of the body.
The survival rate for such infants is considered extremely low, and it largely depends on the state of the baby's immune system. If there is a chance of recovery, it usually proceeds slowly, against the background of difficult and long-term treatment.
Mycoplasma hominis and gardnerella
Often, the difficulties in treating mycoplasmosis are that the infection in most cases is not isolated. In many patients, mycoplasma coexists simultaneously with ureaplasma, chlamydia, trichomonas, gardnerella. That is why the diagnostics of infectious inflammations should be as comprehensive as possible so that the prescribed treatment is adequate and does not lead to a new wave of combined infection.
Gardnerella occupies one of the leading places among inflammatory pathologies of the urogenital system and often becomes the cause of inflammatory processes in the genitals and urinary tract. Mycoplasma in combination with gardnerella is difficult to cure and shows a tendency to repeated episodes of the disease.
Complications and consequences
Mycoplasma often leads to the start of an infectious inflammatory reaction of the genitourinary organs. Some of the undesirable consequences are:
- difficulties in conceiving a child, both for men and women;
- adhesive processes, chronic inflammatory processes;
- disorders during pregnancy;
- anomalies of intrauterine fetal development;
- serious illnesses in a newborn baby, death;
- periodic febrile conditions.
Diagnostics
Since mycoplasma infection has no specific symptoms, this makes diagnosis somewhat difficult. Laboratory tests and collection of epidemiological anamnesis are mandatory. However, not all diagnostic methods for mycoplasma are informative. For example, light microscopy will not help to detect mycoplasma, since this microorganism does not have a membrane.
If the presence of mycoplasma is suspected, the following diagnostic procedures and tests are preferred:
- Mycoplasma hominis culture: a smear is taken from the vaginal walls, or discharge from the cervical canal or urethra. This method only detects mycoplasma hominis in the smear, but not mycoplasma genitalium. The disadvantages of this method are as follows: it is not easy to choose the right nutrient medium for high-quality cultivation, and the growing period can be quite long.
- Immunological analysis for mycoplasma hominis allows to detect antibodies to microbes in the blood. Blood is taken in the morning on an empty stomach. The disadvantage of this method: it is not always informative. For example, with weakened antigenicity and a significant immunodeficiency state, the indicators may become erroneous.
- The polymerase chain reaction method is considered the most informative in terms of determining the presence of mycoplasma. The method allows detecting such structures as DNA mycoplasma hominis - both in blood and in a smear. The main difference between the method and other types of research is that the indicators are not distorted even after antibiotic therapy. The disadvantage of this method: there is a possibility of confusion between the detected DNA of dead microbes and the DNA of active microorganisms.
When conducting an enzyme immunoassay, a negative indicator or the norm of mycoplasma hominis is considered when two indicators of antibodies IgG and IgM are indicated under the minus sign. If the value of mycoplasma hominis IgG is positive, and IgM is negative, then it should be understood that the patient has already formed his own immune response to the infection.
If both values are positive, treatment for mycoplasmosis is necessary.
A complete recovery is considered when a blood test shows that Mycoplasma hominis IgA, IgG and IgM are absent.
Mycoplasma hominis IgG is detected in the blood 2-3 weeks after the onset of the disease: it can also be detected for 1-2 years after clinical recovery. IgM antibodies are detected somewhat earlier. Thus, the titers of antibodies to mycoplasma hominis class IgG increase approximately a week later than those of IgM antibodies, but they remain elevated for a longer period of time.
Quantitative analysis for Mycoplasma hominis is determined by the following reference values:
- IgG:
- less than 0.8 – result (-);
- from 0.8 to 1.1 – the result is questionable;
- from 1.1 and above – result (+).
- IgM:
- less than 0.8 – result (-);
- from 0.8 to 1.1 – the result is questionable;
- from 1.1 and above – result (+).
- IgA:
- less than 0.8 – result (-);
- from 0.8 to 1.1 – the result is questionable;
- from 1.1 and above – result (+).
Instrumental diagnostics is usually limited to the listed types of research. Additional diagnostic procedures may be prescribed only if other diseases are suspected or complications occur.
Differential diagnostics of mycoplasma infection is often very difficult due to the lack of typical symptoms for this infection. Therefore, laboratory tests should become the main diagnostic method. As a rule, mycoplasmosis is differentiated from gonorrhea, vaginal candidiasis, etc.
The test results often raise a lot of questions for patients. For example, mycoplasma hominis and genitalium: what is the difference?
Mycoplasma hominis is a conditionally pathogenic microbe that can be present in the body both normally and in pathological conditions - the only difference is in the quantity of this microorganism.
Mycoplasma genitalium is considered to be an initially pathogenic microbe with a high degree of pathogenicity and contagiousness. Fortunately, mycoplasma genitalium is less common, but differential diagnostics between these two types of mycoplasma is mandatory.
Treatment
Therapy for mycoplasma hominis infection must be comprehensive and include antibiotics, antifungal drugs, and immunomodulators. Macrolide drugs are most often used for antibiotic therapy - these are Clarithromycin, Sumamed, Fromilid, etc. Tetracyclines also have a similar effect. The duration of therapy for mycoplasma is usually 1-3 weeks. However, the doctor can make his own adjustments depending on the course of the disease, the degree of weakness of the immune system, the age and general health of the person.
Enzyme therapy is used mainly in chronic mycoplasmosis, and only in combination with basic antibiotic therapy.
Complex treatment may also include physiotherapy and the use of external medications (for washing, irrigation, suppositories, douching).
Do I need to treat mycoplasma hominis?
Mycoplasma hominis is considered a microbe that can be present in the normal flora of a healthy person, including pregnant women, without causing any troubles or diseases. Under normal conditions, if mycoplasma does not cause painful symptoms, there is no need to treat it. Treatment is prescribed only if there are complaints from the patient. An important difference: if the analysis indicates the presence of mycoplasma genitalium, then treatment must be carried out.
The treatment regimen for mycoplasma hominis is always designed to provide a comprehensive effect. The following medications are usually used:
- Broad-spectrum antibiotics:
- tetracyclines – Doxycycline;
- macrolides – Azithromycin, Clarithromycin;
- fluoroquinolones – Ciprofloxacin, Tsifran.
- Antiprotozoal drugs – Trichopolum.
- External antibacterial and antiseptic agents – Metronidazole suppositories, Oflokain ointment, Hexicon suppositories.
- Antifungal drugs that must be prescribed during antibiotic therapy are Nystatin, Fluconazole, Clotrimazole, as well as Livarol suppositories or others.
- Probiotics that maintain flora balance – Vaginorm, Lactonorm.
- Immunostimulating drugs – Immunal, Immunorix.
- Painkillers for severe pain, non-steroidal anti-inflammatory drugs.
- Complex vitamins – Vitrum, Undevit, Alphabet.
- Douching, irrigation with decoctions of medicinal herbs, Miramistin.
Antibiotics for Mycoplasma Hominis
Dosage and method of administration |
Side effects |
Special instructions |
|
Sumamed |
Take 1 g of the drug once a day, between meals. |
Headache, temporary visual impairment, nausea, abdominal pain. |
Sumamed in capsules cannot be prescribed to children weighing less than 45 kg. |
Clarithromycin |
Take 500 mg twice a day for 3-4 weeks. |
Abdominal pain, diarrhea, nausea, changes in taste. |
Clarithromycin is not used to treat children under 12 years of age. |
Tsifran |
It is used in the form of injections for severe cases of mycoplasmosis, in individually selected dosages. |
Body rash, nausea, diarrhea, transient increase in transaminase activity. |
Tsifran is not recommended for use during pregnancy, breastfeeding, or in pediatrics. |
Oflokain cream |
Used to treat men with mycoplasmosis of the external genitalia. Apply to the skin 2 times a day. |
Itching, redness of the skin, rash, swelling. |
For mycoplasma, Oflokain cream is used only for men. For women, suppositories are appropriate. |
Doxycycline |
Take 100 mg capsules twice a day for at least a week. |
Hypersensitivity reactions, tinnitus, digestive disorders. |
Doxycycline is contraindicated during pregnancy. It is used in children from the age of 12. |
 [ 30 ], [ 31 ], [ 32 ], [ 33 ]
[ 30 ], [ 31 ], [ 32 ], [ 33 ]
Physiotherapy treatment
Physiotherapeutic procedures are prescribed only in case of confirmed mycoplasmosis, as an auxiliary type of treatment. Such procedures will help stop the development of the inflammatory process, prevent the formation of adhesions.
Usually used:
- Electrotherapy (improves blood flow in tissues, relieves pain);
- Magnetic laser treatment (enhances the effect of drugs);
- Ultrasound therapy (improves blood circulation, relieves pain).
Ozone therapy can be used as part of the general treatment plan, which allows for a reduction in the duration of the treatment course by increasing the effect of antibiotics and the ozone’s own antibacterial effect.
Folk remedies
For successful treatment of mycoplasmosis, it is necessary to use a comprehensive approach, with mandatory antibiotic therapy. Doctors unanimously state that it will not be possible to get rid of mycoplasma using folk remedies alone. However, folk remedies will really help eliminate the unpleasant symptoms of mycoplasmosis, and will also effectively complement the traditional conservative treatment prescribed by the doctor.
Fresh garlic for mycoplasma hominis is recommended to be eaten every day, several cloves (at least 2 pieces). You can make garlic salad sauce, and then add it not only to salads, but also pour it over other dishes. To prepare the sauce, you need to mix chopped garlic, lemon juice, a little vegetable oil and salt.
Mycoplasma will leave the body faster if you drink tea brewed from blue cornflower herb three times a day. To make such tea, you need to pour boiling water (250 ml) over two tablespoons of dry herb and keep it under the lid for 50-60 minutes.
St. John's wort and meadowsweet flowers have a good effect against mycoplasma. Two full tablespoons of the equilibrium mixture of these plants are poured with a liter of water and boiled on low heat for 8-10 minutes, then infused under a lid for another 2 hours. Then the medicine is filtered and drunk in a glass three times a day, about a quarter of an hour before meals.
As a supplement, it is recommended to enrich the diet with vitamins to properly support the immune system. It is necessary to include plant products in the menu, as well as decoctions of rose hips, currants, and chamomile.
 [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ]
[ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ]
Herbal treatment
In case of mycoplasma hominis infection of the female reproductive system, it is recommended to douche with the following infusion: take one tablespoon of the herb of the orthilia secunda and two tablespoons of crushed oak bark, pour 400 ml of boiling water, leave for 40 minutes. Cool the resulting infusion, filter it well through gauze and use for douching, morning and night.
Herbal treatment for mycoplasma also includes drinking herbal teas enriched with vitamins, which helps strengthen and support the immune system. Rose hips, cranberries, and pine needles can be used as a base for tea - 2 tablespoons of the ingredients are poured into 0.5 liters of boiling water and left to brew for six hours. The resulting medicine should be drunk every day, 1-2 glasses (with honey).
It is recommended to include a lot of greens (dill, celery stalks, cilantro), seasonal vegetables and citrus fruits in the daily menu.
Homeopathy
Homeopathic remedies for mycoplasma hominis infection can only be used as an adjunctive therapy, as these medications will not be able to remove the infection from the body. However, they can stop the inflammatory process and eliminate the unpleasant symptoms of the disease.
In acute inflammatory processes, the following homeopathic remedies may be useful:
- Aconite;
- Belladonna;
- Coloncite;
- Staphysagria;
- Mercurius corrosivus.
- In the subacute course of the disease, the following is often prescribed:
- Acidum benzoicum;
- Equisetum;
- Nitricum acidum.
In case of frequent relapses of the disease the following will help:
- Thuja;
- Lycopodium;
- Calcarea carbonica.
At the beginning of treatment, it is recommended to use low dilutions (potency) of homeopathic medicines. Later, the dosage can be adjusted depending on how effective the drug is.
Surgical treatment
Surgical intervention for the treatment of Mycoplasma hominis lesions is not practiced.
Prevention mycoplasma chominis
In order to prevent the respiratory variant of mycoplasma infection, special attention should be paid to personal hygiene. It is unacceptable to use other people's dishes for eating, to put on other people's clothes, to dry yourself with other people's towels.
In order to avoid urogenital mycoplasmosis, it is necessary to carefully choose sexual partners and avoid promiscuous sexual relations. Sex with a stranger must be protected.
It is worth noting that mycoplasma infection diagnosed at an early stage has every chance of being completely cured.
Humans do not develop immunity to mycoplasma, so there are no special vaccinations against mycoplasmosis: responsibility for prevention lies entirely with each individual.
Forecast
If the approach to treating mycoplasmosis was competent, and the probability of recurrence of infection is reduced to zero, then several courses of medication usually lead to a cure. It is impossible to cure the disease on your own, without the help of a doctor.
In addition, for complete recovery, it is necessary to be examined for other infectious diseases that may be present in the body along with mycoplasma hominis. If mycoplasma hominis is not the only pathogen, then the treatment may be longer, but it is also completely curable.

