Medical expert of the article
New publications
MRI of the cervical spine with and without contrast: indications, technique of performance
Last reviewed: 03.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
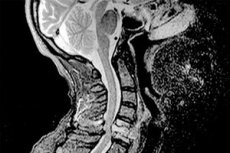
Modern diagnostic studies based on recording the electromagnetic response of the nuclei of atoms that make up the structures of the internal organs of the human body (magnetic resonance imaging) are in many cases the most informative non-invasive options for visualizing pathologies that are invisible during external examination. During the study, the surface of thin sections (sometimes up to 1 mm) is scanned in successive multiple angles, so the idea of the internal structure is the most accurate, making it possible to reconstruct a three-dimensional image of the examined area of the body on a computer. In addition, this method of research does not use X-rays - there is no radioactive irradiation, and the effect of electromagnetic waves on the human body, placed in a magnetic field created by high-voltage direct currents, is considered to be practically insignificant. MRI of the cervical spine allows visualizing muscle, nerve, vascular cartilaginous and articular tissue. As a result of the examination, it is possible not only to assume, but also to accurately detect tumors, ischemic foci, hernias, dissections and inflammations, that is, structures and pathologies about which conventional methods based on the use of X-rays do not provide comprehensive information.
Indications for the procedure
Patients complain of discomfort or pain in the collar zone; tingling, sensory disturbances, disturbing in some areas of the face, neck, shoulder girdle, hands; motor incoordination; headaches, dizziness, pre-fainting and fainting conditions; hearing and vision disorders.
The basis for the recommendation for examination is the assumption of the presence of congenital anomalies, neoplasms (MRI with contrast is the most informative), cerebral circulation disorders, inflammatory or degenerative and dystrophic processes in muscle, vascular and nerve tissues, fractures (dislocations, sprains) in the specified section of the spinal column.
Often, such complaints are the basis for recommending a magnetic resonance imaging study of not only the neck area, but also brain structures.
Preparation
There is no need for any preliminary preparation before performing an MRI of the cervical spine.
If an examination using a contrast agent is planned, it is carried out on an empty stomach or five to six hours after eating.
Immediately before the procedure, the patient removes all metal objects, including earrings, clothing from the upper body, and changes into a disposable gown, which will be given to him before being placed in the device.
 [ 8 ]
[ 8 ]
Technique MRI of the cervical spine
After changing, the patient lies down on a movable table. If necessary (if the patient is not sure that he will be able to remain still for about half an hour), the doctor fixes parts of his body, in this case the head, chest and upper limbs, with clamps and/or belts. After that, the table moves into the ring contour and stops when it is at the level of the armpits. The patient must lie still throughout the procedure to obtain clear, informative images.
The doctor goes into the next room, turns on the device and monitors the process on the computer monitor. It is possible for the patient to communicate with the doctor via an intercom.
During the procedure, the patient hears soft clicks and feels slight heat flows in the examination area. There is no pain during magnetic resonance imaging.
For small children who cannot be taught to remain still, the procedure is performed under general anesthesia. The same procedure can be used for patients with claustrophobia.
The direction may indicate various structures to be studied. Suspecting atherosclerosis, thrombosis, strictures of the arteries of this localization, the doctor recommends doing an MRI of the vessels of the cervical spine. Magnetic resonance angiography can be done without the introduction of a contrast substance and with its use. In 10-15 minutes, the device will take the required number of images from different angles with a section of 1 mm and subsequent volumetric reconstruction of the main arteries that provide blood flow in the cerebral vessels.
Patient complaints indicating cerebrovascular dysfunction are the basis for recommendations to perform a simultaneous MRI of the brain and cervical spine, which will provide the most detailed three-dimensional complex image of the structures of the head and neck, which will show the craniovertebral junction - a structure formed by the occipital bone of the base of the skull and two (first and second) cervical vertebrae.
Sometimes, according to indications, MRI of the craniovertebral junction is performed in isolation, but much more often this area is examined together with the cervical spine.
To specify the visualization in areas with a branched network of vessels, MRI of the cervical spine with intravenous administration of a contrast agent is recommended for clearer visualization of the object. This method is especially effective in detecting neoplasms, since their growth and development require increased blood supply.
The contrast substance, administered intravenously, accumulates in areas supplied with an extensive vascular network. The presence of contrast also helps to conduct an angiographic examination more effectively.
Magnetic resonance imaging uses a contrast agent based on gadolinium, a soft, highly soluble lanthanide metal. It is positioned as absolutely safe, however, everything is not so clear-cut, and modern studies indicate its ability to accumulate in brain tissue, causing intoxication.
The duration of an MRI of the cervical spine is on average 15-20 minutes, with the use of a contrast agent – a little more than half an hour.
The results of the study can be collected in approximately one hour on paper or electronic media.
Contraindications to the procedure
Magnetic resonance imaging is not performed on patients with any electronic or metal implants, except titanium, and fixed prostheses. Severe mental illnesses and severe claustrophobia also prevent the patient from remaining motionless.
Patients with dentures and braces may undergo an MRI of the cervical spine, but their presence must be disclosed to the doctor.
Temporary contraindications are the first three months of pregnancy, decompensated heart failure, pre-comatose and comatose state of the patient, intoxication with psychoactive substances, delirium, non-metallic implants, devices and prostheses (insulin pumps, clips that stop bleeding, valve prostheses, etc.); tattoos applied with metal-containing paints - due to the possibility of burning.
Additionally: magnetic resonance imaging with contrast is not performed on patients with allergies to contrast agents, hemolytic anemia, impaired renal function, and expectant mothers.
Normal performance
The medical report of magnetic resonance imaging fully illuminates the picture of pathological changes in a given area of the spine.
What does an MRI of the cervical spine show?
The tomogram shows osteochondrosis of the cervical spine, various deformations of the intervertebral discs, growths, displacements, fractures.
Congenital defects of the spinal column structure are well visualized, as well as acquired pathologies, consequences of diseases and injuries. It is possible not only to see the narrowing of the spinal canal, consequences of fractures, dislocations, but also often to establish the cause that led to the formation of defects.
A herniated disc in the cervical spine can only be accurately diagnosed with an MRI.
The tomogram shows blood flow disorders and their causes in the form of vascular lesions: hematomas, areas of ischemia, inflammation, neoplasms, atherosclerotic plaques, blood clots, pathological deformations of blood vessels - bends, loops, narrowing, delamination, divergence, dysplastic changes.
Inflammatory processes in the paravertebral and cervical soft tissues, including suppuration, are clearly visible.
Infections affecting the bony elements of the spinal column and spinal cord, degenerative modifications of nerve fibers (multiple sclerosis) can be diagnosed using magnetic resonance imaging.
Primary neoplasms of this localization, as well as metastatic ones, have a specific appearance and are determined by performing MRI.
Fresh bone fractures are also shown by the printout, however, it is better to use radiological diagnostics to visualize them.
 [ 14 ], [ 15 ], [ 16 ], [ 17 ]
[ 14 ], [ 15 ], [ 16 ], [ 17 ]
Decoding the MRI image of the cervical spine
In a person with a healthy spine, the examined bone elements (vertebrae, discs between them, joints) are visible on the computer monitor with a smooth surface, the same shape and height, without integrity violations, surface curvatures, symmetrically located in the corresponding normal places. The nerve fibers of the spinal cord are clearly traced, the endings of the spinal nerves are not pinched, there are no signs of inflammation (swelling, hematomas), and there are no other visible defects.
In case of violations of the integrity of the body or arches of the vertebrae, clear fracture lines, cracks or displacements of parts of the damaged vertebra are visible. In case of compression fractures, parts of the vertebrae are very rarely displaced; the origin of such a fracture can be determined by the tomogram. Osteoporosis is clearly visible - bone structures are not dense, sparse. Tumor origin of compression is also well differentiated on the tomogram.
The main advantage of magnetic resonance imaging over radiation methods is the clear visualization of nerve fibers, which makes it possible to detect destructive changes in the spinal cord that occur with dislocations, sprains, and fractures of the spine.
Herniated intervertebral discs are visualized as arcuate deformations extending beyond the vertebrae. Visible disruption of the outer fibrous wall, through which the contents of the nucleus are visible. Pinched nerve endings located nearby are clearly visible.
The image shows the characteristic unevenness of the narrowed spinal canal with dorsomedial disc protrusion, and an even more advanced stage is noticeable when the protrusion turns into a hernia. Paramedian hernia often interacts with the ends of the spinal nerves, causing their displacement, compression or fusion with structural elements localized nearby.
Primary and metastatic neoplasms, wherever they are located - in the spinal cord and on its membranes, bone structures, are clearly visible on printouts. Sometimes they grow into nearby tissues, can cause compression and displacement of both the spinal cord and its nerve endings, and are often complicated by serious destructive changes in the spine.
Complications after the procedure
If all conditions for diagnostics of the cervical spine using a method based on nuclear magnetic resonance phenomena are met, no negative consequences after the examination threaten you. At present, this method is considered the safest of all the most informative existing diagnostic procedures that allow visualization of the internal structure of the spine in the neck area and adjacent tissues.
Undesirable consequences may arise if contraindications are not followed, such as failure of implanted electronic devices, heating and displacement of metal particles of implants.
When a study involves the introduction of a contrast agent, an unexpected sensitization reaction may occur, but in a medical facility it is quickly stopped with the drugs available for such cases.
Violation of contraindications may lead to intoxication of the patient's body with diseased kidneys by the contrast agent due to its slow elimination.
Also, if a nursing mother neglects the recommendation to interrupt breastfeeding for a day (to remove the contrast from the body), the baby may be poisoned.
Other complications after the procedure are unlikely. No special care is required after the procedure.
Analogues
If the question is which diagnostic method to choose, X-ray or MRI, then you should be guided by the supposed diagnosis.
Radiological diagnostics are more informative if a diagnostic conclusion on the condition of the bone tissue of the spinal column is required. These are X-rays and computed tomography. They are preferable for fractures and dislocations, in addition, X-rays are the most accessible diagnostic method both in price and prevalence.
And magnetic resonance diagnostics is more suitable for solving the problem of visualization of muscle, nervous and vascular tissue - inflammation, degenerative-dystrophic modifications, tumors, primary and metastatic. In addition, the safety level of MRI of the cervical spine is much higher.
You can do an ultrasound of this part of the body. Visualization of internal organs using ultrasound waves is considered the safest, it is indicated even for pregnant women - an unborn child is subjected to ultrasound scanning. However, some tissues of the body remain partially inaccessible to ultrasound diagnostics, including bone tissue. Ultrasound scanning is available for hernias, protrusions, with its help you can detect narrowing of the spinal canal, curvature and age-related deformations, assess the condition of the surface of the spinal cord. However, this method, in addition to its main advantage - safety, also has a number of disadvantages. Ultrasound data often lead to hyperdiagnosis (can indicate a pathology that does not exist), so many doctors still require a more precise diagnosis using another method.

