Medical expert of the article
New publications
Meningococci
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
N. meningitidis, the causative agent of purulent cerebrospinal meningitis, was first discovered in 1884 by E. Marchiafava and E. Celli, and isolated in 1887 by A. Weichselbaum.
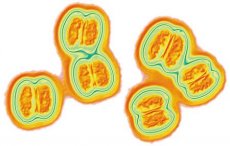
Meningococci are gram-negative spherical cells with a diameter of 0.6-0.8 µm. In smears prepared from material taken from a patient, they have the shape of a coffee bean, are often located in pairs or tetrads, or randomly, often inside leukocytes - incomplete phagocytosis. In smears from cultures, meningococci have a regular round shape, but different sizes, are located randomly or in tetrads, along with gram-negative, there may be gram-positive cocci. They do not form spores, do not have flagella. All meningococci, except for group B, form a capsule. The content of G + C in DNA is 50.5-51.3 mol %. Meningococci are strict aerobes, do not grow on ordinary media. For their growth, the addition of serum is required, the optimal pH for growth is 7.2-7.4, the temperature is 37 °C, at a temperature below 22 "C they do not grow. Colonies on dense media are delicate, transparent, 2-3 mm in size. On the serum broth they form turbidity and a small sediment at the bottom. A film appears on the surface after 2-3 days. When sowing from patients, meningococci are most often isolated in the S-form, however, when cultivated on nutrient media, they often turn into R-forms and lose a number of biological properties, including some antigens, which must be taken into account.
The biochemical activity of meningococci is low. They ferment glucose and maltose to form acid without gas, do not liquefy gelatin, and are oxidase-positive.
Antigenic structure of meningococci
Meningococci have four antigen systems.
Capsular polysaccharide antigens; depending on their specificity, meningococci are divided into the following groups: A, B, C, Y, X, Z, D, N, 29E, W135, H, I, K, L. The chemical composition of specific polysaccharides has been determined for most known serogroups, for example, for serogroup A - N-acetyl-3-O-acetyl-mannose aminophosphate.
- Outer membrane protein antigens. They are divided into 5 classes. Class 2 and 3 proteins define 20 serotypes, and class 1 proteins define subtypes.
- A protein antigen common to the entire species N. meningitidis.
- Lipopolysaccharide antigens - 8 serotypes.
Accordingly, the antigen formula of meningococci is as follows: serogroup: protein serotype: protein subtype: LPS serotype. For example, B:15:P1:16 - serogroup B, serotype 15, subtype 16. The study of the antigen structure is important not only for differentiating meningococci, but also for identifying those antigens that have the greatest immunogenicity.
 [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ]
[ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ]
Resistance of meningococci
Meningococci are extremely unstable to environmental factors. They quickly die under the influence of direct sunlight, die from drying out in a few hours, and when heated to 80 °C - in 2 minutes. Conventional chemical disinfectants kill them in a few minutes. Unlike many other bacteria, they quickly die at low temperatures, which should be taken into account when delivering material from patients in winter.
Pathogenicity factors of meningococci
Meningococci have pathogenicity factors that determine their ability to adhere and colonize cells, invade and protect against phagocytosis. In addition, they are toxic and allergenic. The adhesion and colonization factors are pili and proteins of the outer membrane. The invasiveness factors are hyaluronidase and other enzymes that depolymerize the substrates of the host tissue. The main factor of meningococcal pathogenicity is capsular polysaccharide antigens that protect them from phagocytosis. In acapsular meningococci of serogroup B, polysaccharide antigen B also provides protection from phagocytosis. Suppression of phagocyte activity promotes the unimpeded spread of meningococci in the body and the generalization of the infectious process.
The toxicity of meningococci is due to the presence of lipopolysaccharide, which, in addition to toxicity, has a pyrogenic, necrotic and lethal effect. The presence of such enzymes as neuraminidase, some proteases, plasma coagulase, fibrinolysin, as well as the manifestation of hemolytic and antilysozyme activity can also be considered as pathogenicity factors, although they are detected and manifested to varying degrees in different serogroups.
 [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ]
[ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ]
Post-infectious immunity
After the disease, including in a mild form, a strong long-term antimicrobial immunity against all serogroups of meningococci is formed. It is caused by bactericidal antibodies and immune memory cells.
Epidemiology of meningococcal infection
The source of infection is only humans. A feature of the epidemiology of meningococcal infections is the fairly widespread distribution of the so-called "healthy" carriage, i.e. carriage of meningococci by practically healthy people. Such carriage is the main factor supporting the circulation of meningococci among the population and therefore creating a constant threat of outbreaks of the disease. The ratio of patients with meningococcal infection and "healthy" carriers can vary from 1: 1000 to 1: 20,000. The reason for the "healthy" carriage of meningococci requires clarification.
All major outbreaks of meningococcal infections have been associated with meningococci of serogroups A and, less commonly, C. After the creation of effective vaccines against these serogroups, meningococci of serogroup B began to play a major role in the epidemiology of meningitis. Meningococci of other serogroups cause sporadic diseases.
Symptoms of meningococcal infection
Infection occurs by airborne droplets. The entry point for infection is the nasopharynx, from where meningococci penetrate the lymphatic vessels and blood. Meningococci can cause the following clinical forms of the disease: nasopharyngitis (the mildest form of the disease); meningococcemia (meningococcal sepsis); as a result of overcoming the blood-brain barrier, meningococci can penetrate the cerebrospinal fluid and cause the most severe form of the disease - epidemic cerebrospinal meningitis - purulent inflammation of the meninges of the spinal cord and brain. In such patients, the cerebrospinal fluid is cloudy, contains many leukocytes and flows out in a stream during puncture due to high pressure. In some cases, meningococcal endocarditis develops. With meningococcemia, the adrenal glands and the blood coagulation system are affected. The diversity of clinical manifestations of the disease is apparently determined by the state of specific immunity, on the one hand, and the degree of virulence of the meningococcus, on the other. Mortality in severe forms of meningitis before the use of sulfanilamide drugs and antibiotics reached 60-70%. It remains quite high to this day, to a large extent this depends on the emergence of resistance in meningococci to sulfanilamide drugs and antibiotics.
Laboratory diagnostics of meningococcal infection
The following methods are used.
Bacteriological - a pure culture of the pathogen is isolated and its sensitivity to sulfanilamide drugs and antibiotics is tested. The material for the study is cerebrospinal fluid, blood, exudate, mucus from the pharynx and nasopharynx.
It is not always possible to isolate the pathogen from a sick person, therefore serological reactions are of great importance, with the help of which either specific meningococcal antigens or antibodies to them are detected in patients.
The following serological reactions can be used to detect antigens: coagglutination, latex agglutination, counter immunoelectrophoresis reaction, enzyme immunoassay and erythroimmunoassorption micromethod.
To detect antibodies in the blood of patients and those who have recovered from the disease, RPGA and IFM are used, in which group-specific polysaccharides are used as antigens.
Specific prophylaxis of meningococcal infection
Vaccines obtained from highly purified polysaccharides of serogroups A, C, Y and W135 have been proposed to create artificial immunity against meningitis, but each of them forms only group-specific immunity. The polysaccharide of serogroup B turned out to be non-immunogenic. Since immunity develops against all serogroups of meningococci after the disease, the search for such antigens (including those of serogroup B) that would create reliable immunity against all serogroups, including serogroup B, has resumed.

