Medical expert of the article
New publications
Liver failure syndrome
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Liver failure syndrome (LFS) is a collection of clinical symptoms and laboratory values that result from deterioration of liver function. Liver failure means that the liver does not perform its normal functions adequately. This condition can be temporary or chronic and can have a variety of causes.
Symptoms of liver failure syndrome can vary depending on the degree of deterioration in liver function and include:
- Jaundice: Jaundice is manifested by yellowing of the skin and the sclera of the eyes and may also be accompanied by itching.
- Ascites: This is swelling of the abdomen caused by a buildup of fluid in the abdominal cavity.
- Symptoms of Designorrhea: These include confusion, impaired consciousness, tremors, changes in mental status, and other symptoms associated with brain dysfunction due to toxin buildup.
- Digestive Disorders: Liver failure can lead to a decrease in the body's ability to absorb nutrients, which can lead to weight loss and malnutrition.
- Bleeding syndrome: Deterioration of liver function may lead to clotting disorders and bleeding.
- Anorexia and nausea: Loss of appetite, nausea and vomiting may be symptoms of liver failure syndrome.
- Liver cachexia: This is a condition in which patients lose muscle mass and optimal nutrition.
Liver failure syndrome requires medical intervention and treatment to improve liver function and eliminate or reduce symptoms. Treatment may include drug therapy, diet, blood purification procedures (hemodialysis), liver transplantation, and other interventions, depending on the cause and severity of the liver failure.
Causes of the hepatic failure syndrome
Liver failure can occur for a variety of reasons, including the following:
- Liver cirrhosis: Cir rhosis is a chronic liver disease in which healthy liver tissue is gradually replaced by fibrous desiccation. Cirrhosis can be caused by alcohol, viral hepatitis, fatty hepatosis, and other causes. The gradual destruction of liver tissue leads to impaired liver function.
- Viral hepatitis: Viral infections such as hepatitis B, hepatitis C and others can cause inflammation and damage to the liver which, if prolonged, can lead to liver failure.
- Alcoholic liver disease: Prolonged and excessive alcohol consumption can cause alcoholic hepatitis and cirrhosis, resulting in decreased liver function.
- Fattyliver disease: Fatty hepatosis (or non-alcoholic fatty liver disease) can occur with obesity, diabetes and other metabolic disorders. In prolonged cases, this condition can progress to cirrhosis.
- Autoimmunediseases: Autoimmune diseases can cause inflammation and damage to liver tissue, which can eventually lead to liver failure.
- Medications and toxins: Some medications and toxins can cause damage to the liver, which can lead to impaired liver function. This can be caused by taking certain medications for a long time or by contact with poisonous substances.
- Genetic disorders: Rare genetic disorders such as hemochromatosis, tyrosinemia, and others can lead to liver dysfunction from childhood.
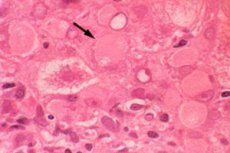
Pathogenesis
The pathogenesis of liver failure syndrome is complex and can be caused by a variety of reasons, but it is usually related to chronic liver damage. Here are some of the key aspects of the pathogenesis of liver failure syndrome:
- Damage to liver cells (hepatocytes): The most common cause of liver failure is damage to hepatocytes, the main functional cells of the liver. This damage can be caused by a variety of factors such as viruses (hepatitis), alcoholic liver disease, fatty liver disease, toxins or medications.
- Decreased protein synthesis: The liver plays an important role in the synthesis of proteins, including blood proteins such as albumin and clotting factors. In liver failure, the synthesis of these proteins can be impaired, which can lead to clotting disorders and edema.
- Ammonia Metabolism Disorder: Normally, the liver is involved in the metabolism of ammonia, a product of amino acid metabolism. In liver failure, blood ammonia levels can rise, which can cause neurologic symptoms known as "portosystemic encephalopathy."
- Toxin Processing Disorder: The liver is the organ of detoxification, and in liver failure, it may be unable to adequately process and remove toxins from the blood, which can lead to impaired function of other organs and systems.
- Increased pressure in the portal vein: Liver failure can lead to impaired blood flow in the liver and increased pressure in the portal vein (portal hypertension), which can cause complications such as dilated veins in the esophagus (varicose veins) and bleeding.
- Carbohydrate and fat metabolism disorders: The liver also plays a role in regulating blood sugar levels and fat metabolism. Liver failure can cause disturbances in these processes.
The term "hepatic cell failure syndrome" is used to describe a condition in which the function of liver cells (hepatocytes) is reduced or lost, resulting in severe liver dysfunction.
Liver failure can be acute or chronic and can have varying degrees of severity.
Symptoms of the hepatic failure syndrome
The symptoms of liver failure syndrome can be varied and depend on the degree of deterioration in liver function. Here are some of the most common symptoms:
- Jaundice (icterus): This is one of the most characteristic signs of liver failure. Jaundice is manifested by yellowing of the skin and whites of the eyes, and it is usually associated with impaired processing and excretion of bilirubin, which is formed when red blood cells break down.
- Ascites (fluid in the abdomen): In patients with liver failure, fluid may accumulate in the abdomen, resulting in abdominal swelling.
- Hepatic encephalopathy: This is a condition in which toxic substances accumulate in the blood that should normally be metabolized by the liver. This can cause mental disorders such as drowsiness, confusion, aggression and even coma.
- Contractive abdominal pain: Patients may experience pain or discomfort in the upper abdomen.
- Swelling(leg swelling): Liver failure can cause fluid and sodium retention in the body, leading to swelling in the legs and shins.
- Blood clotting disorders: The liver also plays an important role in the blood clotting process. With liver failure, patients may have an increased risk of bleeding and decreased platelet counts.
- Enlargement of the spleen (splenomegaly): Splenomegaly may be a consequence of liver failure.
- Decrease in body weight and appetite: Patients may lose their appetite and begin to lose weight.
Liver failure syndrome in children
It is a condition in which a child's liver function is reduced or lost. It is a serious and dangerous condition that can be caused by different reasons and have different manifestations. Below are some of the main causes and symptoms of liver failure syndrome in children:
Reasons:
- Viral Hepatitis: Viral infections such as hepatitis B and hepatitis C can cause inflammation and liver damage in children.
- Liver cirrhosis: Chronic liver damage caused by various causes (e.g., alcohol, viruses, autoimmune diseases) can lead to cirrhosis, which is a major cause of liver failure.
- Autoimmune diseases: Children can develop autoimmune liver diseases such as autoimmune hepatitis, which leads to chronic inflammation and liver damage.
- Genetic disorders: Rare genetic metabolic disorders such as tyrosinemia or galactosemia can cause liver failure in children from birth.
- Poisoning and medications: ingestion of toxins, poisonous substances, or long-term use of certain medications can damage the liver and cause liver failure.
Symptoms:
Symptoms of liver failure syndrome in children may include:
- Jaundice (yellowing of the skin and sclerae)
- Swelling (especially around the eyes and in the abdomen)
- Abdominal pain
- Disorders of consciousness (confusion, drowsiness)
- Digestive disorders (nausea, vomiting, diarrhea)
- Deterioration of growth and development
- Bleeding and bruising
Treatment for liver failure syndrome in children may include drug therapy, diet, supportive therapy to manage symptoms and sometimes liver transplantation, especially in cases of severe failure. Treatment depends on the cause and extent of liver damage and should be carefully monitored by a pediatrician and a hepatologist (liver disease specialist).
Stages
Liver failure syndrome can develop gradually and its severity can range from mild to severe. The stages of liver failure syndrome can be categorized as follows:
-
Compensated liver failure:
- In this stage, the liver is still able to perform most of its functions despite the presence of pathologic changes.
- Symptoms may be mild and may include mild jaundice, weakness and fatigue.
-
Subcompensated liver failure:
- In this stage, liver function deteriorates more significantly.
- Symptoms become more severe and may include jaundice, ascites (swelling of the abdomen), enlarged spleen, nausea and vomiting, impaired consciousness, tremors, and other symptoms.
-
Decompensated liver failure:
- In this stage, liver function is severely impaired and the liver is unable to perform many of its normal functions.
- Symptoms may include severe jaundice, ascites, encephalopathy (impaired consciousness), bleeding syndrome, and other serious manifestations.
-
Liver coma:
- This is the most severe stage of liver failure syndrome in which liver function is completely lost.
- The patient may be in a state of profound unconsciousness, and this condition is extremely dangerous and requires immediate medical attention.
Forms
Liver failure syndrome can have different forms and manifest with a variety of symptoms and clinical signs. Depending on the nature and extent of liver damage, liver failure syndrome may have the following forms:
- Chronic form of liver failure: This form develops slowly and may be caused by chronic liver disease such as cirrhosis, chronic hepatitis or fatty liver disease. The chronic form may present with gradual symptoms such as fatigue, weakness, morning swelling, jaundice, impaired appetite and lack of concentration.
- Acuteliver failure: This form develops rapidly and is usually associated with acute liver damage such as acute hepatic necrosis or liver intoxication. Symptoms of the acute form may include severe jaundice, impaired consciousness (hepatic encephalopathy), bleeding, ascites (fluid in the abdomen), and other severe complications.
- Subclinical: In some cases, liver failure syndrome may have minimal or subclinical manifestations and symptoms may be easily missed. This may occur with a gradual deterioration of liver function.
- Functional form: Sometimes liver failure syndrome can occur against a background of relatively preserved anatomical structure of the liver, but with impaired liver function. This may be due to physiologic changes or drug exposure.
Complications and consequences
Liver failure syndrome can be accompanied by serious complications and systemic organ complications, as the liver plays an important role in many biological processes in the body. Some of the major complications of liver failure syndrome include:
- Encephalopathy: One of the most dangerous complications is hepatic encephalopathy, which is associated with impaired brain function due to the accumulation of toxins in the blood. This condition can manifest as disorientation, forgetfulness, tremors, drowsiness and, in severe cases, coma.
- Gastrointestinal bleeding: Liver failure can lead to impaired blood clotting and increase the risk of bleeding from the digestive tract. This may manifest as blood in the stool or vomiting.
- Ascites: A buildup of fluid in the abdomen, known as ascites, can cause an enlarged abdomen, difficulty breathing, and discomfort.
- Hepatorenal dysfunction syndrome: This complication is characterized by simultaneous impairment of liver and kidney function, which may lead to renal failure.
- Hepatocellular carcinoma: Patients with long-term liver failure may be at increased risk of developing a liver cancer called hepatocellular carcinoma.
- Acute infections: A weakened immune system with liver failure can make the body more vulnerable to infections.
- Acute and chronic kidney disease: Liver failure may cause renal dysfunction and the development of acute or chronic renal failure.
- Weight loss and cachexia: Liver failure may lead to impaired nutrition and weight loss.
Diagnostics of the hepatic failure syndrome
Diagnosing liver failure syndrome involves a number of laboratory and instrumental tests that help determine the degree of deterioration in liver function and its cause. Here are some of the main methods for diagnosing this condition:
- Clinical Exam: The doctor will perform a physical exam and evaluate symptoms such as jaundice, ascites, splenomegaly (enlarged spleen), impaired consciousness, etc.
- Blood tests:
- Measurement of blood bilirubin levels to determine if jaundice is present.
- Measurement of liver enzymes (AST, ALT, ALP) and albumin to assess liver function.
- Performing a coagulogram (coagulation study) to assess the liver's ability to produce clotting proteins.
- Abdominal ultrasound: Ultrasound can help detect changes in the size and structure of the liver, the presence of ascites and other changes.
- Computed tomography (CT) or magnetic resonance imaging (MRI): These methods can provide more detailed information about the condition of the liver and other organs in the abdomen.
- Liver biopsy: Sometimes a sample of liver tissue needs to be taken to better diagnose and determine the cause of liver failure. This can be done by biopsy or puncture.
- Investigations for viral hepatitis: Because viral infections can be a cause of liver failure, special tests may be performed to detect antibodies or viral load.
- Other investigations: Depending on the clinical presentation, other investigations such as angiography, radioisotope techniques, endoscopy, etc. May be required.
Differential diagnosis
Differential diagnosis of liver failure syndrome is the process of excluding or establishing the underlying disease that caused liver failure, as well as identifying other conditions that may mimic its symptoms. The following methods and approaches can be used for differential diagnosis of liver failure syndrome:
- History and clinical examination: The physician gathers detailed information about the patient's medical and family history and performs a physical examination to look for signs and symptoms associated with liver failure.
- Laboratory tests: This includes blood tests, including biochemical measures of liver function (e.g., bilirubin, aminotransferase, albumin levels), blood clotting tests, and checking for viral markers (e.g., hepatitis virus).
- Imaging: Various imaging techniques such as ultrasound (ultrasound), computed tomography (CT) or magnetic resonance imaging (MRI) of the abdomen can be used to evaluate the liver and other organs in the abdomen.
- Liver biopsy: Sometimes a sample of liver tissue (liver biopsy) may need to be taken to evaluate the liver in more detail and to identify underlying disease.
- Functional Tests: Specific functional tests may be performed to assess the liver's ability to perform its functions, such as tests for ammonia metabolism, protein fragments, and others.
- Identifying the underlying disease: After ruling out other possible causes of liver failure, the doctor tries to identify the underlying disease such as cirrhosis, hepatitis, fatty liver dystrophy, liver tumor and others.
The differential diagnosis of liver failure can be challenging and requires collaboration between physicians from different specialties such as gastroenterologists, hepatologists, surgeons, and oncologists.
Who to contact?
Treatment of the hepatic failure syndrome
Treatment of liver failure syndrome depends on the cause of this condition, its severity and the general condition of the patient. It is important to carry out complex therapy, which may include the following measures:
- Treatment of the underlying disease: If liver failure syndrome is caused by a disease such as cirrhosis, hepatitis, or other liver disease, doctors focus on treating that underlying cause. This may include antiviral therapy, alcohol treatment, chronic disease management, and other interventions.
- Drug therapy: The doctor may prescribe medications to manage symptoms and alleviate some manifestations of liver failure, such as antiemetics, lactulose to treat hepatic encephalopathy, anticoagulants to manage bleeding risk, and others.
- Diet: Patients with liver failure may require a protein- and sodium-restricted diet. Controlling fluid intake may also be important to prevent ascites (fluid buildup in the abdomen).
- Detoxification Procedures: Detoxification procedures such as hemodialysis or plasmapheresis may be used to remove toxins from the body.
- Liver transplantation: In cases of severe liver failure that cannot be treated, a liver transplant may be necessary. This may be the only way to save the patient's life.
- Management of complications: Clinicians can take steps to manage complications such as bleeding, hepatitic encephalopathy, ascites, and others.
Treatment of liver failure syndrome requires an individualized approach, and the decision on treatment methods is made by the doctor based on the clinical picture and tests. It is also important to regularly monitor the patient's condition and follow all the doctor's recommendations.
Forecast
The prognosis of liver failure syndrome depends on many factors, including the cause of failure, the extent of liver damage, the effectiveness of treatment, and the patient's overall condition. In general, the prognosis can be quite serious and can range from favorable to critical.
Some factors that affect the prognosis include:
- Cause of liver failure: The prognosis may depend on what caused the failure. For example, some causes such as infections or poisonous substances may be reversible if treatment is started quickly, while chronic diseases such as cirrhosis may have a less favorable prognosis.
- Extent of liver damage: The prognosis also depends on how badly the liver is damaged. The more damage, the more severe the condition and the worse the prognosis.
- Timely access to medical care: The importance of seeking medical attention early cannot be underestimated. In the case of liver failure syndrome, timely initiation of treatment can significantly increase the chances of a favorable outcome.
- Treatment and medical interventions: Effective treatment, including drug therapy, diet, liver transplantation, and other procedures, can improve the condition and prognosis.
- Comorbidities: The presence of other medical problems can complicate treatment and affect prognosis.
The prognosis of liver failure syndrome can range from relatively favorable in case of timely treatment and effective treatment to critical in case of severe failure, especially if liver transplantation is not available. Therefore, it is important to seek medical attention when liver-related symptoms occur and get the necessary medical attention to evaluate and treat the condition.

