Medical expert of the article
New publications
Study of the glomerular filtration rate
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
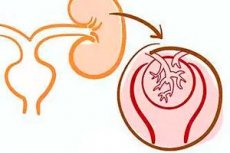
To measure the glomerular filtration rate (GFR), the clearance of substances that are only filtered during transport through the kidneys, without being reabsorbed or secreted in the tubules, are well soluble in water, freely pass through the pores of the glomerular basement membrane and do not bind to plasma proteins are used. Such substances include inulin, endogenous and exogenous creatinine, urea. In recent years, ethylenediaminetetraacetic acid and glomerulotropic radiopharmaceuticals such as diethylenetriaminepentaacetate or iothalamate labeled with radioisotopes have become widely used as marker substances. Unlabeled contrast agents (unlabeled iothalamate and iogexol) have also come into use.
Glomerular filtration rate is the main indicator of kidney function in healthy and sick people. Its determination is used to assess the effectiveness of therapy aimed at preventing the progression of chronic diffuse kidney diseases.
Inulin, a polysaccharide with a molecular weight of 5200 daltons, can be considered an ideal marker for determining the glomerular filtration rate. It is freely filtered through the glomerular filter, is not secreted, is not reabsorbed, and is not metabolized in the kidneys. In this regard, inulin clearance is used today as the "gold standard" for determining the glomerular filtration rate. Unfortunately, there are technical difficulties in determining inulin clearance, and this is an expensive study.
The use of radioisotope markers also allows determining the glomerular filtration rate. The results of the determinations closely correlate with the clearance of inulin. However, radioisotope research methods are associated with the introduction of radioactive substances, the presence of expensive equipment, as well as the need to comply with certain standards for the storage and administration of these substances. In this regard, studies of the glomerular filtration rate using radioactive isotopes are used in the presence of special radiological laboratories.
In recent years, a new method using serum cystatin C, a protease inhibitor, has been proposed as a marker of SCF. Currently, due to the incompleteness of population studies evaluating this method, information on its effectiveness is lacking.
Until recent years, endogenous creatinine clearance was the most widely used method for determining the glomerular filtration rate in clinical practice. To determine the glomerular filtration rate, daily urine collection (for 14-40 min) is performed or urine is obtained for separate intervals (usually for 2 intervals of 2 hours) with a preliminary water load to achieve sufficient diuresis. Endogenous creatinine clearance is calculated using the clearance formula.
Comparison of the SCF results obtained in the study of creatinine clearance and inulin clearance in healthy individuals revealed a close correlation of the indicators. However, with the development of moderate and, especially, severe renal failure, the SCF calculated from the clearance of endogenous creatinine significantly exceeded (by more than 25%) the SCF values obtained from the clearance of inulin. With an SCF of 20 ml/min, creatinine clearance exceeded inulin clearance by 1.7 times. The reason for the discrepancy in the results was that, under conditions of renal failure and uremia, the kidney begins to secrete creatinine by the proximal tubules. Preliminary (2 hours before the start of the study) administration of cimetidine to the patient, a substance that blocks the secretion of creatinine, at a dose of 1200 mg helps to level out the error. After pre-administration of cimetidine, creatinine clearance in patients with moderate and severe renal insufficiency did not differ from insulin clearance.
Currently, calculation methods for determining SCF, taking into account the concentration of creatinine in the blood serum and a number of other indicators (gender, height, body weight, age), are widely introduced into clinical practice. Cockcroft and Gault proposed the following formula for calculating SCF, which is currently used by most practicing physicians.
The glomerular filtration rate for men is calculated using the formula:
(140 - age) x m: (72 x R cr ),
Where P cr is the concentration of creatinine in blood plasma, mg%; m is body weight, kg. SCF for women is calculated using the formula:
(140 - age) x mx 0.85: (72 x R cr ),
Where P cr is the concentration of creatinine in blood plasma, mg%; m is body weight, kg.
Comparison of the SCF calculated using the Cockcroft-Gault formula with the SCF values determined using the most accurate clearance methods (inulin clearance, 1,125 - iothalamate) revealed a high comparability of the results. In the vast majority of comparative studies, the calculated SCF differed from the true value by 14% or less in the negative direction and by 25% or less in the positive direction; in 75% of cases, the differences did not exceed 30%.
In recent years, the MDRD (Modification of Diet in Renal Disease Study) formula has been widely introduced into practice to determine the SCF:
SCF+6.09x(serum creatinine, mol/L) -0.999x (age) -0.176x (0.762 for women (1.18 for African Americans)x(serum urea, mol/L) -0.17x (serum albumin, g/L) 0318.
Comparative studies have shown the high reliability of this formula: in more than 90% of cases, the deviations of the calculation results using the MDRD formula did not exceed 30% of the measured SCF values. Only in 2% of cases did the error exceed 50%.
Normally, the glomerular filtration rate for men is 97-137 ml/min, for women - 88-128 ml/min.
Under physiological conditions, the glomerular filtration rate increases during pregnancy and when consuming high-protein foods and decreases with aging. Thus, after 40 years, the rate of decline in GFR is 1% per year, or 6.5 ml/min per decade. At the age of 60-80 years, the GFR decreases by half.
In pathology, the glomerular filtration rate often decreases, but can also increase. In diseases not associated with kidney pathology, a decrease in GFR is most often due to hemodynamic factors - hypotension, shock, hypovolemia, severe heart failure, dehydration, and taking NSAIDs.
In kidney diseases, a decrease in the filtration function of the kidneys is mainly associated with structural disorders that lead to a decrease in the mass of active nephrons, a decrease in the filtering surface of the glomerulus, a decrease in the ultrafiltration coefficient, a decrease in renal blood flow, and obstruction of the renal tubules.
These factors cause a decrease in the glomerular filtration rate in all chronic diffuse kidney diseases [chronic glomerulonephritis (CGN), pyelonephritis, polycystic kidney disease, etc.], kidney damage in the context of systemic connective tissue diseases, with the development of nephrosclerosis against the background of arterial hypertension, acute renal failure, obstruction of the urinary tract, severe damage to the heart, liver and other organs.
In pathological processes in the kidneys, an increase in SCF is detected much less frequently due to an increase in ultrafiltration pressure, ultrafiltration coefficient or renal blood flow. These factors are important in the development of high SCF in the early stages of diabetes mellitus, hypertension, systemic lupus erythematosus, in the initial period of nephrotic syndrome. Currently, long-term hyperfiltration is considered as one of the non-immune mechanisms of renal failure progression.
Load tests to determine glomerular filtration reserve
The glomerular filtration rate under physiological conditions changes during the day depending on the physical and psychological state of the individual, the composition of the food consumed, and the administration of drugs. Maximum values are detected after eating a large amount of meat protein. The ability of the kidneys to increase the SCF in response to a stimulus was used as the basis for determining the glomerular filtration reserve or renal functional reserve (RFR).
To assess the PFR, a single (acute) load of protein or amino acids or the administration of small doses of dopamine is usually used.
Acute protein loading
The test involves eating 70-90 g of meat protein (1.5 g of protein per 1 kg of body weight, which corresponds to 5 g of boiled beef per 1 kg of body weight), 100 g of vegetable protein, or intravenous administration of a set of amino acids.
In healthy individuals, in response to an acute protein load or the introduction of amino acids, the SCF increases by 20-65% in the next 1-2.5 hours after the load. The average SCF is 20-35 ml/min.
The calculation of the Pension Fund is made according to the formula:
PFR = (SCF 2 - SCF 1 ): SCF 1,
Where SCF 1 is the SCF under basal conditions (in the morning, on an empty stomach), SCF 2 is the SCF after the introduction of meat or amino acids (stimulated SCF). The result is expressed as a percentage.
In kidney diseases, the PFR may remain at a normal level or decrease. A sharp decrease (less than 10%) or the absence of a reserve (less than 5%) indirectly reflect the state of hyperfiltration in the functioning nephrons. Low PFR values can be observed both with a normal SCF value (in the early stages of diabetic nephropathy, with nephrotic syndrome) and with suppression of SCF in patients with renal failure.


 [
[