Medical expert of the article
New publications
Examination of cranial nerves. Pair XII: hyoid nerve (n. hypoglossus)
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
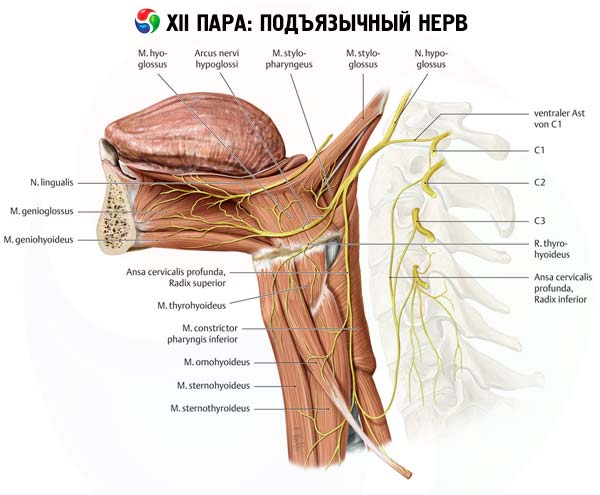
The hypoglossal nerve innervates the muscles of the tongue (with the exception of the palatoglossus m., supplied by the X pair of cranial nerves).
Inspection
The examination begins with an examination of the tongue in the oral cavity and when it is protruded. Attention is paid to the presence of atrophy and fasciculations. Fasciculations are vermiform rapid irregular twitching of the muscle. Atrophy of the tongue is manifested by a decrease in its volume, the presence of grooves and folds of its mucous membrane. Fascicular twitching in the tongue indicates the involvement of the hypoglossal nerve nucleus in the pathological process. Unilateral atrophy of the tongue muscles is usually observed with tumor, vascular or traumatic damage to the trunk of the hypoglossal nerve at or below the level of the base of the skull; it is rarely associated with an intramedullary process. Bilateral atrophy most often occurs with motor neuron disease ( amyotrophic lateral sclerosis (ALS) ) and syringobulbia. To assess the function of the tongue muscles, the patient is asked to stick out his tongue.
Normally, the patient easily shows the tongue; when protruding, it is located along the midline. Paresis of the muscles of one half of the tongue leads to its deviation to the weak side (i.e., the genioglossus of the healthy side pushes the tongue toward the paretic muscles). The tongue always deviates toward the weak side, regardless of what kind of lesion - supranuclear or nuclear - is the cause of the weakness of the tongue muscle. It is necessary to make sure that the deviation of the tongue is real and not imaginary.
A false impression of tongue deviation may arise with facial asymmetry caused by unilateral weakness of the facial muscles. The patient is asked to perform quick movements of the tongue from side to side. If the weakness of the tongue is not entirely obvious, the patient is asked to press the tongue on the inner surface of the cheek and the strength of the tongue is assessed by counteracting this movement. The force of tongue pressure on the inner surface of the right cheek reflects the strength of the left m. genioglossus, and vice versa. The patient is then asked to pronounce syllables with frontal lingual sounds (e.g., "la-la-la"). If the tongue muscle is weak, the patient cannot pronounce them clearly. To detect mild dysarthria, the subject is asked to repeat complex phrases, such as: "administrative experiment", "episodic assistant", "large red grapes ripen on Mount Ararat", etc.
Combined damage to the nuclei, roots or trunks of the IX, X, XI, XII pairs of cranial nerves causes the development of bulbar paralysis or paresis. Clinical manifestations of bulbar paralysis are dysphagia (difficulty swallowing and choking when eating due to paresis of the muscles of the pharynx and epiglottis ); nasolalia (nasal voice associated with paresis of the muscles of the soft palate); dysphonia (loss of sonority of the voice due to paresis of the muscles involved in narrowing/widening the glottis and tension/relaxation of the vocal cord); dysarthria (paresis of the muscles that ensure correct articulation); atrophy and fasciculations of the muscles of the tongue; fading of the palatal, pharyngeal and cough reflexes; respiratory and cardiovascular disorders; sometimes flaccid paresis of the sternocleidomastoid and trapezius muscles.
The IX, X, and XI nerves exit the cranial cavity together through the jugular foramen, so unilateral bulbar palsy is usually observed when these cranial nerves are affected by a tumor. Bilateral bulbar palsy can be caused by poliomyelitis and other neuroinfections, ALS, Kennedy's bulbospinal amyotrophy, or toxic polyneuropathy (diphtheria, paraneoplastic, with GBS, etc.). Damage to neuromuscular synapses in myasthenia or muscle pathology in some forms of myopathies can cause the same disorders of bulbar motor functions as in bulbar palsy.
Pseudobulbar paralysis, which develops with bilateral damage to the upper motor neuron of the corticonuclear tracts, should be distinguished from bulbar paralysis, which affects the lower motor neuron (the nuclei of the cranial nerves or their fibers). Pseudobulbar paralysis is a combined dysfunction of the IX, X, XII pairs of cranial nerves caused by bilateral damage to the corticonuclear tracts leading to their nuclei. The clinical picture resembles the manifestations of bulbar syndrome and includes dysphagia, nasal speech, dysphonia, and dysarthria. In pseudobulbar syndrome, unlike bulbar syndrome, the pharyngeal, palatine, and cough reflexes are preserved; reflexes of oral automatism appear, the mandibular reflex increases; forced crying or laughter (uncontrolled emotional reactions) are observed, hypotrophy and fasciculations of the muscles of the tongue are absent.
What do need to examine?

