Medical expert of the article
New publications
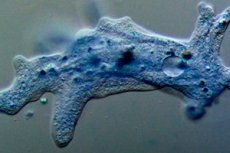
Intestinal amoeba in humans: structure of cysts, life cycle
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Intestinal amoeba is a non-pathogenic microorganism that lives in the lumen of the lower small intestine and upper large intestine. It is a permanent parasitic organism, but can also exist outside of it.
In the external environment, the intestinal amoeba survives well, and in some cases can reproduce, but still, a favorable place for it is the intestines of a person or another living organism. It uses non-living organic substrates (bacteria, remains of various foods) as food, and the amoeba does not secrete an enzyme that breaks down proteins into amino acids. Due to this, in most cases, it does not penetrate the intestinal wall, which means it does not harm the host. This phenomenon is called carriage. When the immune system is weakened and other circumstances coincide, the amoeba penetrates under the intestinal mucosa and begins to multiply intensively.
Structure intestinal amoeba
The intestinal amoeba belongs to the protozoa type. The structure of the intestinal amoeba consists of a body and a nucleus. The body contains protoplasm (a liquid substance with specialized living structures) and one, two, rarely several nuclei. Protoplasm has two layers: internal (endoplasm) and external (ectoplasm). The nucleus resembles a bubble.
There are two phases of the intestinal amoeba's existence: a vegetative individual (trophozoites) and a cyst. Trophozoites have a clearly distinguishable nucleus with a diameter of 20-40 microns. The amoeba constantly changes its shape due to the appearance of pseudopods, with the help of which movement and capture of food occurs. Thanks to the shape of pseudopodia, nuclei, their number, one or another type of amoeba is identified. Its movements are slow, reminiscent of trampling on the spot. Reproduction occurs by division of nuclei first, then protoplasm.
Life cycle intestinal amoeba
The intestinal amoeba life cycle begins with infection of the host organism via the fecal-oral route. With unwashed hands, vegetables, fruits, and various carriers (flies, cockroaches), amoeba cysts enter the human body. Thanks to their shell, they pass through the aggressive environment of the stomach and duodenum intact, entering the intestine. Its enzymes dissolve the shell, allowing the intestinal amoeba to exit.
The vegetative stage of development has the following forms: tissue, lumen and pre-cyst. Of these, the tissue phase is the most mobile, and it is at this time that the amoeba is most invasive. The other two are slightly mobile. From the lumen form, some amoebas pass into the pre-cyst form, while others penetrate under the intestinal mucosa, forming a pathogenic tissue form. As a result of its vital activity, the latter secretes cytolysins that melt tissue and create conditions for reproduction. The cyst is immobile, and leaves the intestines during defecation. In severe infections, up to 300 million individuals leave the body per day.
Intestinal amoeba cysts
After several reproduction cycles, when unfavorable conditions for the vegetative individual occur, it is covered with a membrane, forming a cyst. The cysts of the intestinal amoeba are round or oval, 10-30 microns in size. Sometimes they contain a supply of nutrients. At different stages of development, cysts have a different number of nuclei: from two to eight. They come out with feces, in large quantities in case of severe infection, and have the ability to survive for a long time. Getting back into a living organism, they burst, turning into an amoeba.
Symptoms
A large accumulation of intestinal amoeba, which occurs when a person's immunity is reduced after stress, viral infections, respiratory diseases, causes a disease called amebiasis. It is most often intestinal and extraintestinal. Intestinal leads to ulcerative lesions of the large intestine and, as a consequence, a protracted course. In this case, the amoeba penetrates into other internal organs, most often the liver, along with the blood and damages them, causing extraintestinal abscesses.
Symptoms of amoebiasis are primarily loose stools, which may be crimson in color. Painful sensations occur in the upper right part of the abdomen, since the localization of these organisms occurs in the upper part of the large intestine. Temperature may rise, chills may occur, and jaundice may appear.
Intestinal amoeba in children
The mechanism of infection of intestinal amoeba in children is the same as in adults, and the source is unwashed hands, flies, dirty toys and household items. Amebiasis can be asymptomatic, manifest, in acute or chronic form. Asymptomatic is unnoticeable for the child. Manifest form is indicated by deterioration of health, weakness, loss of appetite. Temperature can be normal or slightly increased. Diarrhea appears, defecation occurs several times a day, increasing to 10-20 times. Mucus with blood appears in foul-smelling liquid feces. The color of feces is not always crimson. Paroxysmal pains in the right side of the abdomen are noted, intensifying before defecation. Without treatment, the acute stage lasts for a month and a half, gradually subsiding. After the remission stage, it flares up with renewed vigor.
Diagnostics
Diagnosis of intestinal amoeba begins with finding out the patient's medical history: what symptoms, how long ago they appeared, whether the patient has been in countries with a hot, humid climate and poor sanitary culture. It is there that the amoeba is widespread and it is from there that it can be imported.
Blood, feces and urine tests are performed. Pathogens are detected in feces, and it is important to identify the vegetative form of amoeba. The test must be done no later than 15 minutes after defecation. Amoebas can also be detected in tissues during a rectoscopy - a visual examination of the rectal mucosa using a special device. A rectoscope makes it possible to see ulcers or fresh scars on its inner surface. Failure to detect traces of mucosal lesions does not mean that there is no amoebiasis, since they can be located in higher parts of the intestine. There is a blood test to detect antibodies to amoebas, it will confirm or refute the diagnosis.
Using ultrasound, fluoroscopy, and tomography, the localization of abscesses in extraintestinal amebiasis is determined. Intestinal amebiasis is differentiated from ulcerative colitis, and amoebic abscesses are differentiated from abscesses of a different nature.
The difference between intestinal amoeba and dysenteric amoeba
The difference between the intestinal amoeba and the dysenteric amoeba is in its structure: the dysenteric amoeba has a double-contour shell that refracts light, it has 4 nuclei (the intestinal amoeba has 8), located eccentrically, and it includes blood cells, which the intestinal amoeba does not. The dysenteric amoeba is more energetic in its movements.
Treatment
Treatment of intestinal amoeba is carried out depending on the severity and form of the disease. The drugs used to eliminate the disease are divided into universal action amoebicides (metronidazole, tinidazole) and direct, aimed at a specific localization of the pathogen: in the intestinal lumen (quiniofon (yatren), mexaform, etc.); in the intestinal wall, liver and other organs (emetine hydrochloride, dehydroemetine, etc.). Tetracycline antibiotics are indirect amoebicides that affect amoebae in the intestinal lumen and in its walls.
Asymptomatic intestinal amebiasis is treated with yatren. During an acute outbreak, metronidazole or tinidazole is prescribed. In severe cases, metronidazole is combined with yatren or tetracycline antibiotics, and dehydroemetine may be added. In the case of extraintestinal abscesses, metronidazole is treated with yatren or hingamine with dehydroemetine. Outpatient observation is carried out for a year.
Prevention intestinal amoeba
The best prevention of intestinal amoeba is personal hygiene - frequent washing of hands, raw vegetables and fruits under running water, not drinking tap water or open sources. These rules should be followed especially strictly when traveling to countries with hot and humid climates.
Isolation of sick people until they fully recover is another necessary preventive measure. If the pathogen is detected in a food service worker, the entire premises are disinfected.
Forecast
Early detection of intestinal amoeba gives a favorable prognosis for treatment. Long-term infection without treatment is complicated by the formation of adhesions in the intestine, perforation of amoebic ulcers, peritonitis, which is very dangerous.
After the disease is cured, there may be no re-infection or the disease may pass easily, as immunity is developed. In the case of extraintestinal abscesses and their late diagnosis, a fatal outcome is possible.


 [
[