Medical expert of the article
New publications
Cervical cancer vaccination
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

The cervical cancer vaccine is a vaccine that prevents infection with the dangerous human papillomavirus. Nowadays, medicine knows about a large number of HPV types (about 100), which cause the development of various diseases. In 70% of women, this virus is considered the main cause of oncology, including cervical cancer. The occurrence of a malignant tumor is provoked by about 15 types of HPV, of which the 16th and 18th types are the most oncogenic.
The basis of vaccines is a particle that does not contain a genome and consists only of the virus shell. By itself, it cannot cause the development of the disease or provoke its exacerbation, but it forms a stable immunity to all oncogenic types of HPV. It should be noted the importance of such a preventive measure, because often even the use of the most innovative methods of treating a malignant tumor does not give the desired result, which leads to death. Therefore, it is better to prevent the disease with the help of vaccination that prevents infection, which doctors recommend for girls from the age of 12.
Where can I get vaccinated against cervical cancer?
The cervical cancer vaccine can reliably protect a woman's body from the dangerous human papillomavirus, which provokes the development of many diseases.
Many women are interested in the question of where to get vaccinated against cervical cancer? It should be noted that both vaccines used for this purpose - Cervarix and Gardasil - are imported, which affects their price. There are currently no domestic analogues of these drugs. The HPV vaccine can be obtained in the gynecological department of a medical institution where the specified vaccines are available. This method is convenient because in one hospital you can undergo an examination (examination by a gynecologist), take a smear for cytology and get vaccinated.
Private clinics may also have vaccines to prevent cervical cancer. If desired, you can get vaccinated there, having first clarified the cost of this procedure. It may be much higher, which is due to the pricing policy of each individual medical institution.
In addition to the above options, vaccination against cervical cancer can be done at a city vaccination center or the immunology department of a medical institution. Only proven vaccines are used here, and the rules for storing the drugs are strictly observed. By the way, vaccination centers and many private clinics offer a special service for home vaccination. In this case, a team of doctors will come to your home, a qualified doctor will conduct an examination and, based on the results, will allow or prohibit vaccination. If the vaccination is done, medical specialists will monitor your condition for half an hour to provide quick assistance in case of an allergic reaction. The home vaccination method is considered the most optimal. In this case, contacts with other people are minimized, which eliminates the possibility of infection or the flu virus. Other advantages of this method include convenience and maximum attention from doctors.
When to get vaccinated against cervical cancer?
Many women are interested in the question of when to get vaccinated against cervical cancer. That is, what age period is optimal for this? First of all, it should be noted that such vaccination is recommended by doctors, but is not a mandatory preventive measure.
Vaccination against cervical cancer is recommended for girls (starting from the age of 12) and young women under the age of 25 (i.e. vaccination should be done before the onset of sexual relations and possible HPV infection). Unfortunately, the vaccine will not work if the virus is present in the body. It should be emphasized that the papillomavirus is not the only cause of cervical cancer. Therefore, vaccination does not provide a 100% guarantee that the disease can be avoided.
The best age to get this vaccination is 15-17 years, when the girl's body is formed and puberty is almost over. Young women who are sexually active should undergo a diagnostic examination to detect the human papillomavirus and clearly determine its type. For this purpose, the PCR method is used (taking a smear (biomaterial) from the vagina and cervix). Before vaccination, it is necessary to consult a doctor about contraindications for this procedure, as well as side effects, including the possibility of allergic reactions. The choice of drug remains with the woman, as is the decision to vaccinate.
Where do you get the cervical cancer vaccine?
The cervical cancer vaccine reliably protects the body from the most dangerous (oncogenic) types of HPV and is considered a recombinant vaccine, i.e. this drug does not contain the genetic material of the papillomavirus, but only protein antigens.
Many women are interested in the question of where to administer the cervical cancer vaccine. Based on the composition of the drug, the optimal method of administering the injection is determined - intramuscular. Since recombinant vaccines are characterized by low reactogenicity, they contain aluminum hydroxide. It enhances the effect of immunity in response to the entry of active elements of the vaccine into the blood, simultaneously performing two functions. The first is the active adsorption of protein antigens, and the second is to cause an inflammatory reaction at the injection site. That is why the most correct place for the injection will be a part of the body with developed muscle tissue - i.e. the thigh or shoulder.

When administering the drug, it is important to get it directly into the muscle – this way the vaccine will enter the blood at maximum speed, ensuring the formation of special antibodies to protect against HPV. Getting the vaccine into the fatty layer or skin will provoke a low release rate, which means the destruction of active particles and the ineffectiveness of the vaccination.
Injection of the vaccine into one of the buttocks is prohibited, as it can cause various complications, such as injury to the sciatic nerve with a syringe needle. The ineffectiveness of such vaccination is due to the deep location of muscle fibers in the buttock.
Names of vaccinations
The cervical cancer vaccine protects against the main pathogen of the disease – the papillomavirus. Statistics show that up to 60% of women worldwide are infected with this virus. It is not surprising that this diagnosis ranks third among the most common oncological diseases.
The names of HPV vaccines used in modern medicine are Gardasil (an American drug) and Cervarix (a Belgian vaccine). Both vaccines are administered once in a lifetime. Their effective action aimed at preventing the development of malignant tumors has been proven.
Gardasil is a mandatory vaccine in the United States and Australia, given to all girls aged 11-13. This vaccine contains components from 4 types of HPV – 6, 11, 16 and 18. Cervarix protects only against 2 types of HPV – 16 and 18.
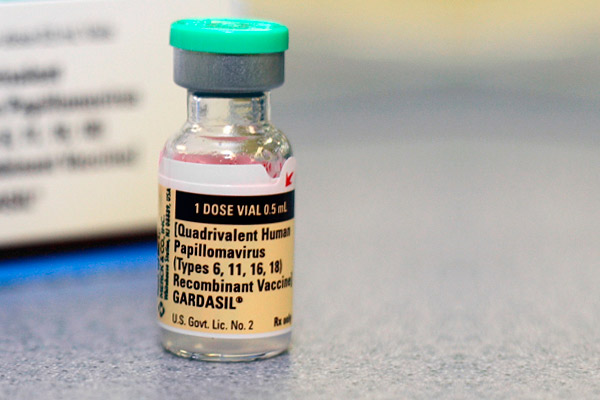
The active components of the vaccines contain only parts of the HPV protein shells, which guarantees their complete safety from the point of view of infection. Excipients are aluminum hydroxide, yeast elements, preservatives and antibacterial agents. The vaccines are produced in the form of suspensions, ready for use and poured into vials or disposable syringes with an exact dosage of the drug. In general, three doses must be administered according to specific schemes. The optimal temperature for storing vaccines is 2-8 °C. Vaccines cannot be replaced or alternated, i.e. the same drug must be used in a vaccination course consisting of 3 doses.
Complications after vaccination
The cervical cancer vaccine is completely safe and does not cause any serious side effects.
Complications after vaccination manifest themselves in the form of a local reaction - redness, pain, swelling, slight itching. Such symptoms do not require special treatment and go away on their own in a couple of days. If part of the vaccine got into the subcutaneous fat layer, and not into the muscle, a lump or bump may appear at the injection site. Do not worry, even if the absorption time takes several weeks.
In addition to a local reaction, vaccination may cause minor general symptoms: malaise, headache, fever (maximum - up to 38 °C), weakness. These symptoms may be observed for several days. High temperature can be brought down with antipyretic drugs (Paracetamol, Ibuprofen, Nise, etc.). If you are prone to allergic reactions, vaccination is done while taking 2-3 generation antihistamines (Fenistil, Erius, etc.), which do not provoke dryness of the mucous membranes.
Vaccination against cervical cancer is today considered one of the most effective preventive measures and is widely used in many countries around the world.


 [
[