Medical expert of the article
New publications
Huntington's disease
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Huntington's disease is an autosomal dominant neurodegenerative disorder characterized by progressive cognitive decline, involuntary movements, and impaired motor coordination beginning in middle age. Diagnosis is confirmed by genetic testing. Treatment is primarily symptomatic. Genetic testing may be recommended for blood relatives. George Huntington first described the condition in 1872, after studying a family case in Long Island residents.
The prevalence of Huntington's disease is approximately 10 cases per 100,000 population, and given its late onset, approximately 30 people out of 100,000 have a 50% risk of developing it in their lifetime. Although the disease most often appears between the ages of 35 and 40, the age range of onset is quite wide, with the earliest onset being at age 3 and the latest at age 90. Although the disease was originally thought to have 100% penetrance, this is now believed to be not always the case. In individuals who inherited the gene for the disease from their father, the disease manifests itself on average 3 years earlier than in those who inherited the pathological gene from their mother. In approximately 80% of patients who inherited the pathological gene from their father, the disease manifests itself before age 20. The phenomenon of earlier manifestation of a genetic defect in offspring is called anticipation.
 [ 1 ]
[ 1 ]
What causes Huntington's disease?
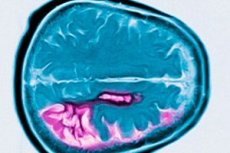
Huntington's disease has no gender preference. Atrophy of the caudate nucleus is shown, where small neurons degenerate and the level of neurotransmitters - gamma-aminobutyric acid (GABA) and substance P - falls.
A mutant gene with an increased number ("expansion") of CAG (cysteine-alanine-glycine) DNA sequences encoding the amino acid glutamine is responsible for the development of Huntington's disease. The product of this gene, the large protein huntingtin, contains an excessive amount of polyglutamine residues, which leads to the disease by an unknown mechanism. The more CAG repeats, the earlier the disease debuts and the more severe its course. From generation to generation, the number of repeats can increase, which over time leads to an aggravation of the family phenotype.
Despite considerable interest in the genetic and biochemical changes in Parkinson's disease, the search for a gene for the disease was unsuccessful until the late 1970s. At that time, Nancy Wexler and Allan Tobin organized a workshop sponsored by the Hereditary Disease Foundation to discuss a strategy for finding a gene for Huntington's disease. David Housman, David Botstein, and Ray White, who attended the meeting, suggested that recently developed recombinant DNA techniques might help achieve this goal. A key task in the project was to find a large family with many generations of Huntington's disease to obtain DNA samples. In 1979, a joint project of scientists from Venezuela and the United States was launched to examine a large family with Huntington's disease living on the shores of Lake Maracheibo (Venezuela). In 1983, the Huntington's disease gene was localized at the end of the short arm of chromosome 4 (Gusella et al., 1983), and a decade later it was revealed that the mutation of this gene consists of an increase in the number of repeats of the cytosine-adenine-guanine (CAG) trinucleotide (Huntington's Disease Collaborative Research Group, 1993). The methodology developed by this scientific group is currently considered standard for positional cloning of new genes.
While the wild-type gene has a stretch of 10-28 CAG repeats, the mutant form of the gene that causes Huntington's disease has an increased stretch from 39 to more than 100 CAG repeats. The discovery of the expansion of trinucleotide repeats has helped explain many of the clinical features of the disease. In particular, an inverse correlation was found between the age of onset and the length of the region with repeated trinucleotides. Anticipation of paternal inheritance can be explained by the fact that an increase in the number of repeats often occurs in men during spermatogenesis. Analysis of new mutations has shown that they usually occur when one of the parents, usually the father, had a CAG repeat count higher than 28; in this case, the number of these repeats increased in the next generation. It has now been established that if the number of repeats is no more than 28, it is stably transmitted from generation to generation. If the number of repeats is from 29 to 35, then symptoms of Huntington's disease do not appear, but when passed on to offspring, the length of this region may increase. If the number of repeats is from 36 to 39, then in some cases (but not always) the disease may manifest itself clinically (incomplete penetrance), and when passed on to offspring, an increase in the number of trinucleotide repeats is possible. If the number of repeats exceeds 40, then the disease occurs in almost all cases, and when passed on to offspring, further expansion of repeats is possible. The reasons for the increase in the number of repeats remain unknown.
Pathomorphology of Huntington's disease
Huntington's disease is characterized by neuronal loss predominantly in the caudate nucleus and putamen, and to some extent also in the cortex and other brain structures. Total brain weight in Huntington's disease is reduced not only by a decrease in the number of neurons, but also by the loss of white matter. In the cerebral cortex, cells in layers V and VI are most affected. The severity of micro- and macroscopic degenerative changes (adjusted for age at death) correlates with the number of CAG repeats. Detailed pathological analysis of changes in several hundred cases of Huntington's disease has shown that degeneration of the striatum begins in the dorsomedial part of the caudate nucleus and the dorsolateral part of the putamen, and then spreads ventrally. Different groups of neurons in the caudate nucleus and putamen are affected to different degrees. Interneurons in the striatum remain relatively intact, but some projection neurons are selectively affected. In the juvenile form of Huntington's disease, pathomorphological changes in the striatum are more pronounced and more widespread, involving the cerebral cortex, cerebellum, thalamus, and globus pallidus.
Neurochemical changes in Huntington's disease
GABA. Neurochemical studies of the brain in patients with Huntington's disease revealed a significant decrease in GABA concentration in the striatum. Subsequent studies confirmed that Huntington's disease is associated with a decrease in the number of GABAergic neurons and showed that GABA concentrations are reduced not only in the striatum but also in its projection zones - the external and internal segments of the globus pallidus and the substantia nigra. In the brain in Huntington's disease, changes in GABA receptors were also detected using receptor binding studies and in situ hybridization of mRNA. The number of GABA receptors was moderately reduced in the caudate nucleus and putamen, but increased in the reticular part of the substantia nigra and the external segment of the globus pallidus, which is likely due to denervation hypersensitivity.
Acetylcholine. Acetylcholine is used as a neurotransmitter by large nonspiny interneurons in the striatum. Early postmortem studies in patients with Huntington's disease showed decreased choline acetyltransferase (ChAT) activity in the striatum, suggesting a loss of cholinergic neurons. However, compared with the significant reduction in GABAergic neurons, cholinergic interneurons are relatively spared. Therefore, the density of acetylcholinesterase-positive neurons and ChAT activity in the striatum are actually relatively elevated compared with age-matched controls.
Substance P. Substance P is contained in many medium spiny neurons of the striatum, which predominantly project to the internal segment of the globus pallidus and the substantia nigra and usually also contain dynorphin and GABA. Substance P levels in the striatum and the pars reticularis of the substantia nigra are reduced in Huntington's disease. In the terminal stage of the disease, immunohistochemical studies have revealed a significant reduction in the number of neurons containing substance P. In earlier stages, neurons containing substance P and projecting to the internal segment of the globus pallidus are relatively spared, compared with neurons projecting to the pars reticularis of the substantia nigra.
Opioid peptides. Enkephalin is contained in the medium spiny projection GABAergic neurons of the indirect pathway, which project to the external segment of the globus pallidus and carry D2 receptors. Immunohistochemical studies have shown that enkephalin-containing neurons projecting to the external segment of the globus pallidus are lost early in Huntington's disease. These cells apparently die earlier than substance P-containing cells projecting to the internal segment of the globus pallidus.
Catecholamines. Neurons containing biogenic amines (dopamine, serotonin) and projecting to the striatum are located in the compact part of the substantia nigra, ventral tegmentum, and raphe nuclei. While noradrenergic projections to the human striatum are minimal, serotonin and dopamine levels (per gram of tissue) in the striatum are elevated, indicating the preservation of these afferent projections despite the marked loss of the striatum's own neurons. Dopaminergic neurons of the substantia nigra remain intact in both classical and juvenile forms of Huntington's disease.
Somatostatin/neuropeptide Y and nitric oxide synthetase. Measurement of somatostatin and neuropeptide Y levels in the striatum in Huntington's disease revealed a 4-5-fold increase compared to normal tissues. Immunohistochemical studies showed absolute preservation of striatal interneurons containing neuropeptide Y, somatostatin and nitric oxide synthetase. Thus, these neurons are resistant to the pathological process.
Excitatory amino acids. It has been suggested that selective cell death in Huntington's disease is due to a glutamate-induced neurotoxic effect. Levels of glutamate and quinolinic acid (an endogenous neurotoxin that is a by-product of serotonin metabolism and an agonist of glutamate receptors) in the striatum of Huntington's disease are slightly altered, but a recent study using MR spectroscopy revealed an increase in glutamate levels in vivo. The level of the glial enzyme responsible for the synthesis of quinolinic acid in the striatum of Huntington's disease is increased by about 5 times compared to normal, while the activity of the enzyme that ensures the degradation of quinolinic acid is increased in Huntington's disease by only 20-50%. Thus, the synthesis of quinolinic acid may be increased in Huntington's disease.
Studies of excitatory amino acid (EAA) receptors in Huntington's disease have revealed a significant reduction in the number of NMDA, AMPA, kainate, and metabotropic glutamate receptors in the striatum, as well as AMPA and kainate receptors in the cerebral cortex. In the late stage of Huntington's disease, NMDA receptors were virtually absent, while in the preclinical and early stages, a significant reduction in the number of these receptors was noted.
Selective sensitivity. In Huntington's disease, certain types of striatal cells are selectively lost. The medium spiny neurons, which project to the external segment of the globus pallidus and contain GABA and enkephalin, die very early in the disease, as do the neurons containing GABA and substance P and projecting to the reticular part of the substantia nigra. The loss of neurons containing GABA and enkephalin and projecting to the external segment of the globus pallidus disinhibits this structure, which in turn leads to active inhibition of the subthalamic nucleus. The decreased activity of the subthalamic nucleus can apparently explain the choreiform movements that occur in Huntington's disease. It has long been known that focal lesions of the subthalamic nucleus can cause chorea. Loss of GABA and substance P neurons projecting to the substantia nigra pars reticularis is likely to be responsible for the oculomotor disturbances seen in Huntington's disease. This pathway normally inhibits substantia nigra pars reticularis neurons projecting to the superior colliculus, which in turn regulate saccades. In juvenile Huntington's disease, the pathways mentioned above are more severely affected and, in addition, striatal projections to the internal segment of the globus pallidus are lost early.
The protein huntingtin, encoded by the gene whose mutation causes Huntington's disease, is found in various structures of the brain and other tissues. Huntingtin is normally found predominantly in the cytoplasm of neurons. The protein is found in most neurons in the brain, but recent data show that its content is higher in matrix neurons than in striosomal neurons, and higher in projection neurons than in interneurons. Thus, the selective sensitivity of neurons correlates with their huntingtin content, which is normally present in certain neuronal populations.
As in the brains of patients with Huntington's disease, in mice transgenic for the N-terminal fragment of the Huntington's disease gene with an expanded number of repeats, huntingtin forms dense aggregates in the nuclei of neurons. These intranuclear inclusions form in striatal projection neurons (but not in interneurons). In transgenic mice, the inclusions form several weeks before the onset of symptoms. These data suggest that huntingtin protein containing an increased number of glutamine residues whose inclusions encode trinucleotide repeats, or a fragment of it, accumulates in the nucleus and may consequently impair its control of cellular functions.
Symptoms of Huntington's disease
The age at which the first symptoms appeared in patients with Huntington's disease is difficult to determine with precision, since the disease manifests itself gradually. Changes in personality and behavior, mild coordination disorders may occur many years before the appearance of more obvious symptoms. By the time the diagnosis is established, most patients have choreic movements, impaired coordination of fine movements, and slow generation of voluntary saccades. As the disease progresses, the ability to organize one's activities is impaired, memory decreases, speech becomes difficult, oculomotor disorders and impaired performance of coordinated movements increase. Although at the early stage of the disease there are no changes in muscle and posture, as it progresses, dystonic postures may develop, which over time may turn into a dominant symptom. At a late stage, speech becomes slurred, swallowing becomes significantly difficult, walking becomes impossible. Huntington's disease usually progresses over 15-20 years. In the terminal stage, the patient is helpless and requires constant care. The fatal outcome is not directly related to the primary disease, but to its complications, for example, pneumonia.
Dementia in Huntington's disease
ICD-10 code
P02.2. Dementia in Huntington's disease (G10).
Dementia develops as one of the manifestations of a systemic degenerative-atrophic process with predominant damage to the striatal system of the brain and other subcoecal nuclei. It is inherited in an autosomal dominant manner.
As a rule, the disease manifests itself in the third or fourth decade of life with choreoform hyperkinesis (especially in the face, arms, shoulders, gait), personality changes (excitable, hysterical and schizoid types of personality anomalies), psychotic disorders (special depression with gloom, sullenness, dysphoria; paranoid mood).
Of particular importance for diagnostics is the combination of choreoform hyperkinesis, dementia and hereditary burden. The following is specific for this dementia:
- slow progression (on average 10-15 years): dissociation between the remaining ability to care for oneself and obvious intellectual incompetence in situations requiring productive mental work (conceptual thinking, learning new things);
- pronounced unevenness of mental performance, which is based on gross disturbances of attention and inconstancy of the patient’s attitudes (“jerky” thinking, similar to hyperkinesis);
- atypicality of obvious violations of higher cortical functions;
- inverse relationship between the increase in dementia and the severity of psychotic disorders.
Taking into account the high proportion of psychotic (paranoid delusions of jealousy, persecution) and dysphoric disorders in the clinical picture of the disease, treatment is carried out using various neuroleptics that block dopaminergic receptors (phenothiazine and butyrophenone derivatives) or reduce the level of dopamine in tissues (reserpine).
Haloperidol (2-20 mg/day), tiapride (100-600 mg/day) for no more than three months, thioridazine (up to 100 mg/day), reserpine (0.25-2 mg/day), and the anticonvulsant clonazepam (1.5-6 mg/day) are used. These drugs help reduce hyperkinesis, smooth out affective tension, and compensate for personality disorders.
Inpatient treatment of mental disorders is carried out taking into account the leading syndrome, age and general condition of the patient. In outpatient treatment, the principles of therapy are the same (continuous maintenance therapy of movement disorders, periodic change of drug). Lower doses of neuroleptics are used in outpatient treatment.
Rehabilitation measures for mild and moderate dementia include occupational therapy, psychotherapy, and cognitive training. It is necessary to work with family members and provide psychological support to people caring for the patient. The main method of disease prevention is medical and genetic counseling of the patient's closest relatives with a referral for DNA analysis when deciding on childbearing.
The prognosis is generally unfavorable. The course of the disease is slowly progressive, and the disease usually leads to death after 10-15 years.
 [ 18 ]
[ 18 ]
What's bothering you?
Diagnosis of Huntington's disease
Diagnosis is based on typical symptoms, family history, and genetic testing. Due to atrophy of the head of the caudate nucleus, MRI and CG reveal enlargement of the cerebral ventricles in the late stage of the disease.
Treatment of Huntington's disease
Treatment of Huntington's disease is symptomatic. Chorea and agitation can be partially suppressed with neuroleptics (eg, chlorpromazine 25-300 mg orally 3 times a day, haloperidol 5-45 mg orally 2 times a day) or reserpine 0.1 mg orally once a day. Doses are increased to the maximum tolerated (before side effects occur, such as drowsiness, parkinsonism; for reserpine, hypotension). The goal of empirical therapy is to reduce glutamatergic transmission via Nmethyl-O-aspartate receptors and maintain energy production in the mitochondria. Treatment aimed at increasing GABA in the brain is ineffective.
Genetic testing and counseling are important because symptoms of the disease appear after the childbearing years. People with a positive family history and those interested in testing are referred to specialized centers, taking into account all the ethical and psychological implications.
Symptomatic treatment of Huntington's disease
There is no effective treatment that can stop the progression of Huntington's disease. Several trials of various drugs have been conducted, but no significant effect has been achieved. Neuroleptics and other dopamine receptor antagonists are widely used to correct mental disorders and involuntary movements in patients with Huntington's disease. Involuntary movements reflect an imbalance between the dopaminergic and GABAergic systems. Accordingly, neuroleptics are used to reduce excess dopaminergic activity. However, these drugs themselves can cause significant cognitive and extrapyramidal side effects. In addition, except in cases where the patient develops psychosis or agitation, their effectiveness has not been proven. Neuroleptics often cause or aggravate dysphagia or other movement disorders. Newer generation neuroleptics such as risperidone, clozapine and olanzapine may be particularly useful in the treatment of Huntington's disease because they cause fewer extrapyramidal side effects but may reduce paranoid symptoms or increased irritability.
Tetrabenazine and reserpine also reduce the activity of the dopaminergic system and can reduce the severity of involuntary movements in the early stages of the disease. However, these drugs can cause depression. Since the disease itself often causes depression, this side effect significantly limits the use of reserpine and tetrabenazine. In the late stages of the disease, cells bearing dopamine receptors die, so the effectiveness of dopamine receptor antagonists is weakened or lost.
Neuroleptics, antidepressants, and anxiolytics are used to treat psychosis, depression, and irritability in patients with Huntington's disease, but they should only be prescribed for as long as the patient actually has these symptoms. Drugs that may be helpful at one stage of the disease may become ineffective or even harmful as the disease progresses.
GABA receptor agonists have been tested in patients with Huntington's disease, since Huntington's disease has been shown to have a significant decrease in GABA levels in the striatum, as well as hypersensitivity of GABA receptors in its projection areas. Benzodiazepines have proven effective in cases where involuntary movements and cognitive impairment are aggravated by stress and anxiety. Low doses of these drugs should be prescribed to avoid unwanted sedative effects. In most patients with Huntington's disease, none of the drugs leads to a significant improvement in quality of life.
In early-onset Huntington's disease with parkinsonian symptoms, dopaminergic agents may be tried, but their effectiveness is limited. Moreover, levodopa may cause or increase myoclonus in these patients. At the same time, baclofen may reduce rigidity in some patients with Huntington's disease.
 [ 26 ], [ 27 ], [ 28 ], [ 29 ]
[ 26 ], [ 27 ], [ 28 ], [ 29 ]
Preventive (neuroprotective) treatment of Huntington's disease
Although the genetic defect in Huntington's disease is known, how it leads to selective neuronal degeneration remains unclear. It is hypothesized that preventive therapies aimed at reducing oxidative stress and excitotoxicity may potentially slow or halt disease progression. The situation may be somewhat similar to hepatolenticular degeneration, in which the genetic defect remained unknown for many years, but preventive therapies aimed at the secondary effect, copper accumulation, were "cured." In this regard, the hypothesis that Huntington's disease is associated with a disorder of energy metabolism and cell death due to excitotoxicity has attracted particular attention. The disease itself may cause cell death due to intranuclear aggregation of N-terminal fragments of huntingtin, which disrupts cellular and metabolic functions. This process may affect some groups of neurons to a greater extent than others due to their higher sensitivity to excitotoxic damage. In this case, preventive therapy with excitatory amino acid receptor antagonists or agents that prevent free radical damage will be able to prevent or delay the onset and progression of the disease. In laboratory models of amyotrophic lateral sclerosis, it has been shown that antioxidant agents and receptor antagonists (RAAs) are able to slow down the progression of the disease. Similar approaches may be effective in Huntington's disease. Clinical trials of glutamate receptor antagonists and agents that enhance the function of complex II of the mitochondrial electron transport chain are currently underway.
 [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ]
[ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ]

