Medical expert of the article
New publications
Hereditary nonpolyposis colorectal carcinoma: causes, symptoms, diagnosis, treatment
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
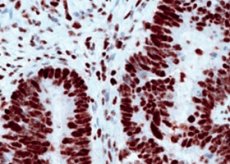
Hereditary nonpolyposis colorectal carcinoma (HNPCC) is an autosomal dominant disorder that accounts for 3-5% of colorectal cancer cases. Symptoms, initial diagnosis, and treatment are similar to other forms of colorectal cancer. HNPCC is suspected based on history and requires confirmation by genetic testing. Patients also require observation for other malignancies, particularly endometrial and ovarian cancer.
Patients with one of several known mutations have a 70-80% lifetime risk of developing colorectal cancer. Compared with sporadic forms of colon cancer, HNSCC occurs at a younger age (average 40 years) and the lesion is more likely to be proximal to the splenic flexure. Previous colonic disease usually consists of a solitary colonic adenoma, in contrast to the multiple adenomas seen in patients with familial adenomatous polyposis (FAP), another inherited form of colorectal cancer.
However, similar to FAP, numerous extraintestinal manifestations may be seen. Benign lesions include café-au-lait spots, sebaceous cysts, and keratoacanthomas. The main associated malignancies are endometrial and ovarian tumors (risk 39% and 9%, respectively, at age 70 years). Patients also have an increased risk of cancer of the ureter, renal pelvis, stomach, biliary tract, and small intestine.
Symptoms of hereditary nonpolyposis colorectal carcinoma
Symptoms and signs are similar to other forms of colorectal cancer. The same applies to the diagnosis and main directions of treatment of the tumor itself. The specificity of the diagnosis of HNCRC is confirmed by genetic testing. However, it is quite difficult to accept the test result, since (unlike FAP) there are no typical clinical manifestations. Thus, suspicion of HNCRC requires a detailed study of the family history, coinciding with FAP, which should be collected from all young patients.
According to the Amsterdam II criteria for HNCCC, all three of the following history elements must be present: (1) three or more relatives with FAP or HNCCC-associated malignancy, (2) colorectal cancer occurring in at least two generations, and (3) at least one case of FAP before age 50.
Diagnosis of hereditary nonpolyposis colorectal carcinoma
Patients who meet these criteria should have their tumor tissue examined for DNA changes called microsatellite variation (MSI). If significant MSI is detected, genetic testing for specific HNCGC mutations is indicated. Other authors use additional criteria (e.g., Bethesda criteria) to initiate MSI testing. If MSI testing is not performed at a given institution, the patient should be referred to a specialized center.
Patients with confirmed HNSCC require further screening for other malignancies. Annual endometrial aspiration and transvaginal ultrasound are recommended to detect endometrial cancer. For ovarian cancer, investigations include annual transvaginal ultrasound and serum CA 125 levels. Prophylactic hysterectomy and oophorectomy are also the treatment of choice. Urinalysis is used to screen for renal tumors.
First-degree relatives of patients with HNSCC should have colonoscopy every 1 to 2 years beginning at age 20 and annually after age 40. Female first-degree relatives should be screened annually for endometrial cancer and ovarian cancer. More distant relatives should have genetic testing; if the test results are negative, they should have colonoscopy similar to average-risk patients.
What do need to examine?
How to examine?


 [
[