Medical expert of the article
New publications
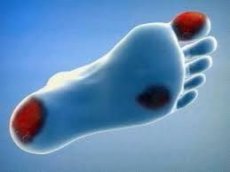
Gangrene of the foot
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
How common is foot gangrene?
Obliterating diseases of the arteries of the legs affect up to 2% of the world's population, the overwhelming majority of them are men. Gradual progression of the pathology over 5 years leads to critical ischemia of the lower extremities in 10-40% of patients. Mortality varies within 6-35%.
In 30-60% of cases, gangrene is caused by acute occlusion of the main arteries, with mortality reaching 45%. Mortality in limb necrosis caused by ileofemoral phlebothrombosis, a rather rare but extremely severe pathology, reaches 60%.
What causes gangrene of the foot?
Gangrene of the foot characterizes the terminal stage of chronic arterial insufficiency of the legs. It is caused by gradually progressing diseases of the main arteries. Sudden occlusion of the main arteries of the lower extremities during their embolism or thrombosis leads to acute ischemia. The development of contracture in the joints indicates the death of muscle tissue. Morphological examination of such patients reveals necrosis of leg tissues, despite the absence of external signs of gangrene.
Ileofemoral phlebothrombosis, occurring with the development of the so-called blue phlegmasia of the limb; impaired blood flow in small "non-main" vessels (for example, in diabetes mellitus and various arteritis), trauma (mechanical, thermal, chemical) of the distal parts of the legs - all this also leads to destruction and necrosis of tissues. The outcome of the disease can be not only the loss of a leg, but also the death of the patient due to intoxication.
What types of foot gangrene are there?
Depending on the reaction of the tissues surrounding the necrotic focus, wet and dry gangrene of the foot is distinguished.
Hyperemia, swelling of tissues around necrotic masses in combination with a characteristic foul odor are characteristic of the wet form. As a rule, its development is provoked by putrefactive microorganisms.
How is foot gangrene recognized?
When examining a patient with gangrene of the foot, it is important to determine the underlying cause of its development, as well as to assess the viability of the leg tissues at various levels. After all the examinations, it is necessary to decide on the possibility of performing revascularization of the limb in order to prevent the progression of necrosis.
Arterial insufficiency is characterized by numbness and constant pain in the legs, which decreases when the leg is lowered. A history of gradually increasing intermittent claudication is characteristic of obliterating thromboangiitis or non-specific aortoarteritis at a young age, and of obliterating atherosclerosis in the elderly. A sharp coldness of the legs, impaired sensitivity and motor activity are noted with embolism or thrombosis of the main arteries of the legs. Rapid development of edema is typical of phlebothrombosis. Moderate pain localized in the necrosis zone is characteristic of diseases based on microcirculatory disorders.
When examining a patient with gangrene of the lower limb, attention should be paid to his position. Thus, for a patient with decompensated arterial insufficiency, a sitting position on a bed with a lowered leg, which he periodically rubs, is typical. On the contrary, with venous pathology, the patient, as a rule, lies with a raised lower limb.
The etiology of necrosis can also be judged by the appearance of the limb. Hypotrophy, lack of hair, fungal infection of the nail plates are characteristic signs of chronic arterial insufficiency. Edema and cyanosis or pallor of the legs are typical for acute venous or arterial insufficiency, respectively.
Cold skin on palpation indicates limb ischemia. The key stage of clinical examination of a patient with trophic disorders is determining arterial pulsation in the affected limb. If the pulse is detected in the distal sections, then pathology of the main blood flow can be excluded. The absence of a pulse in typical points (under the inguinal fold, in the popliteal fossa, on the back or behind the medial malleolus) indicates arterial insufficiency. Contracture in the ankle or knee joints is typical for severe ischemia.
Gangrene of the foot requires standard tests for surgical patients:
- general blood test;
- biochemical blood test;
- determination of blood glucose levels.
A microbiological examination of the necrotic focus is mandatory, with determination of the sensitivity of the microflora to various antibacterial drugs.
It is advisable to begin the instrumental examination of the patient with ultrasound duplex angioscanning. This method allows answering several fundamental questions.
- Is there any significant pathology of the main vessels of the legs?
- Is surgical revascularization of the limb possible?
- Is occlusive-stenotic lesion of the main arteries accompanied by pronounced hemodynamic disturbances?
The answer to the last question can be obtained by measuring the systolic pressure in the main arteries in the lower third of the leg using ultrasound Doppler. Systolic pressure in the tibial arteries below 50 mm Hg or an ankle-brachial index of less than 0.3 indicate critical ischemia of the distal parts of the legs. Angiography in patients with gangrene is only justified in preparation for vascular surgery.
One of the most informative methods for assessing the state of tissue blood flow in gangrene of the legs is scintigraphy with 11Tc-pyrfotech. This radiopharmaceutical has affinity for bone tissue and necrosis foci (especially with perifocal inflammation). The distribution of the isotope in the legs is assessed 2.5 hours after intravenous administration. The level of accumulation of 11Tc-pyrfotech in the affected limb less than 60% of that in the contralateral "healthy" limb is considered low, indicating severe ischemia.
Laser Doppler flowmetry allows to determine the degree of tissue blood flow disturbance quite accurately. In addition to basal blood flow indicators, it is necessary to determine its reaction to functional tests: postural and occlusion. In critical ischemia, basal blood flow has a characteristic monophasic low-amplitude appearance; the reaction to the postural test is inverted, to the occlusion test - sharply slowed.
Patients with foot gangrene that developed against the background of a systemic disease (e.g., obliterating atherosclerosis, diabetes mellitus, arteritis) should be consulted by a therapist, cardiologist, neurologist, and endocrinologist. Sometimes a gastroenterologist consultation is required, since 30% of patients with foot gangrene against the background of critical leg ischemia have erosive and ulcerative lesions of the upper gastrointestinal tract.
Gangrene of the foot is differentiated from the following diseases:
- with severe dermatitis;
- with necrotic form of erysipelas;
- with positional compression syndrome.
The diagnostic algorithm includes an assessment of the condition of the legs and other organs and systems. The result of the clinical and instrumental examination of a patient with gangrene of the lower limb should be a clearly formulated diagnosis, reflecting, in addition to the condition and prevalence of the necrotic focus, the nature of the underlying disease.
How is foot gangrene treated?
The goal of treatment is to eliminate the purulent-necrotic focus and subsequent complete healing of the wound. The desire for maximum preservation of the limb is the postulate of modern surgery.
Outpatient treatment is possible in case of local necrosis caused by microcirculatory disorders. Pathology of the main vessels of the limb complicated by necrosis is an indication for hospitalization.
Drug treatment is aimed at improving tissue blood flow, and in case of intoxication symptoms - complex, including antibacterial, anti-inflammatory and detoxifying therapy. When prescribing antibiotics, it should be taken into account that in all patients with long-term necrosis, the regional lymphatic system is infected. Moreover, a microbiological study of the popliteal and inguinal lymph nodes, performed after 20-30 days of inpatient treatment, usually reveals the same microflora that was in the area of trophic disorders at the time of hospitalization. Thus, antibacterial therapy for a condition such as gangrene of the foot is long-term and is prescribed taking into account the sensitivity to drugs of both the microflora existing in the wound discharge (if any) and the microorganisms identified in the necrotic focus during hospitalization.
The scope of surgical intervention depends on the size of the necrotic focus, the characteristics of regional hemodynamics and the general condition of the patient.
The development of necrosis against the background of microcirculatory disorders with preserved main blood flow in the distal parts of the legs allows us to limit ourselves to radical necrectomy with the application of a drainage-washing system (or without it) and primary wound suturing.
Satisfactory perfusion of tissues surrounding the necrotic focus even against the background of disturbances in the main blood flow is the basis for minimizing the volume of sanitizing intervention (only necrotic masses are removed). If there is doubt about the viability of the remaining tissues, primary sutures are not applied, leaving the wound open.
In patients with gangrene of the foot against the background of limb ischemia, the severity of the general condition should be taken into account, since vascular interventions in decompensated concomitant pathology are characterized by a higher mortality rate than primary amputation at the thigh level. When choosing the volume of intervention in patients with critical ischemia, it is necessary to assess whether the supporting function will be preserved in the case of hemodynamically effective revascularization. Indications for amputation at the level of the leg or thigh:
- total gangrene of the foot;
- necrosis of the heel area with involvement of bone structures;
- occlusion of the distal arterial bed of the legs.
When choosing the level of intervention, one should be guided by the clinical picture of the disease and the data of the instrumental examination. Thus, in acute vascular pathology (embolism and thrombosis of the main arteries, thrombosis of the main veins), amputation is performed 15-20 cm above the proximal border of the clinical manifestations of ischemia. Determining the indicators of tissue blood flow in various segments of the limb allows amputation to be performed in the area of satisfactory microcirculation.
Surgical tactics in chronic arterial insufficiency of the legs complicated by necrosis are differentiated. Direct revascularization of the lower limb is indicated when the volume of destruction and subsequent necrectomy allows us to expect preservation of the supporting function and there is a distal arterial bed suitable for reconstruction. It is advisable to perform sanitation of the lesion and vascular reconstruction simultaneously. Guillotine necrectomy is the optimal volume (minimal, since additional trauma to ischemic tissues leads to progression of necrosis) of simultaneous sanitizing intervention with vascular reconstruction. Subsequently, the wound is treated openly.
According to instrumental research methods, maximum restoration of tissue blood flow occurs one month after hemodynamically effective vascular reconstruction. That is why repeated intervention on the foot, which usually combines staged necrectomy and plastic wound closure, is advisable to perform no earlier than one month after revascularization.
Surgical treatment methods
Disarticulation of the finger
Gangrene of the foot and distal phalanx of the toe against the background of satisfactory tissue blood flow in the foot is the main indication for surgery. Dorsal and plantar cutaneous-subcutaneous-fascial flaps are cut out. The capsule and lateral ligaments of the interphalangeal joint are dissected, turning the main phalanx to the dorsal side. It is necessary to try not to damage the articular surface of the head of the metatarsal bone. After removal of bone structures, primary sutures are applied and, if necessary, the wound is drained.
Amputation of fingers with resection of the metatarsal head
Indication for surgery: gangrene of the foot and distal and main phalanges of the toe against the background of satisfactory tissue blood flow in the foot. Dorsal and plantar cutaneous-subcutaneous-fascial flaps are cut out. The metatarsal bone is cut proximal to the head with a Gigli saw, the sawing is processed with a rasp. The tendons of the muscles - flexors and extensors of the toe are isolated and cut as high as possible. The operation is completed by applying primary sutures and drainage (or without it, depending on the clinical situation).
Sharp amputation
Indication for surgery - gangrene of the foot and several toes against the background of satisfactory tissue blood flow in the foot. Dorsal and plantar skin-subcutaneous-fascial flaps are cut out.
The tendons of the muscles - flexors and extensors of the fingers - are isolated and crossed as high as possible. The metatarsal bones are separately isolated and sawed in the middle, the sawing is processed with a rasp. The operation is completed by applying primary sutures and drainage or without it, depending on the clinical situation.
Chopard amputation
Indication for surgery: gangrene of the foot and toes, spreading to the distal part against the background of satisfactory tissue blood flow in it. Two bordering incisions are made in the area of the heads of the metatarsal bones.
The metatarsal bones are isolated. The tendons are crossed as high as possible. The amputation is performed along the line of the transverse joint of the tarsus (Chopar's) with preservation of the calcaneus, talus and part of the metatarsus. The stump is covered with a plantar flap immediately or after the inflammatory process has subsided.
Amputation of the lower leg
Indication for surgery - gangrene of the foot against the background of satisfactory blood flow in the shin and low - in the foot. Two skin-subcutaneous-fascial flaps are cut out: a long posterior and a short anterior, 13-15 and 1-2 cm, respectively.
The muscles around the fibula are cut transversely, the peroneal nerve and vessels are isolated and cut. The fibula is cut 1-2 cm above the level of the tibia. The periosteum along the line of dissection is shifted only in the distal direction. First, the fibula is cut and only then the tibia. The anterior and posterior tibial vessels are isolated and ligated. The muscles are cut. Due to the peculiarities of the blood supply, it is advisable to remove the soleus muscle.
The sawed-off tibias are processed, the soft tissues are sutured without tension, leaving a tubular drainage at the bottom of the wound for active aspiration.
 [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
Amputation of the thigh
Indication for surgery - gangrene of the foot against the background of low tissue blood flow in the foot and lower leg. Anterior and posterior skin-subcutaneous flaps are cut out.
The great saphenous vein is isolated and ligated. The proper fascia of the thigh is dissected, the sartorius muscle is mobilized and transected. Then the superficial femoral artery and vein are exposed. The vessels are mobilized, ligated twice, and dissected. In the posterior group of thigh muscles, the sciatic nerve is isolated, infiltrated with an anesthetic solution, ligated with an absorbable thread, and cut off as high as possible. After this, the anterior and posterior groups of the thigh muscles are transected with an amputation knife. The exposed femur is cleared of periosteum in the distal direction with a raspatory and, after proximal abduction of the muscles, is sawed with a retractor.
The sharp edges of the saw are processed with a rasp and rounded. Careful hemostasis is performed in the intersected muscles (they are then either sutured or not if they are swollen, bleed poorly, or have a dull color). Sutures are necessarily applied to the fascia and skin, leaving tubular drains under the fascia and muscles for active aspiration.
 [ 21 ], [ 22 ], [ 23 ], [ 24 ]
[ 21 ], [ 22 ], [ 23 ], [ 24 ]
Postoperative complications
The main postoperative complication in patients with gangrene of the foot is the progression of limb necrosis, which is usually associated with an error in the choice of the level of intervention. Thus, amputations (against the background of arterial insufficiency) require reamputation in more than 50% of cases; at the level of the shin - in 10-18%; thigh - only in 3% of patients. With the development of wound complications (suppuration, necrosis of the wound edges), repeated interventions are often required. Long-term non-healing wounds, as well as bone fragments protruding from soft tissues are indications for reamputation. However, it is important to remember that mortality rates for reamputations are always higher than those after primary interventions at the same level.
Patients with gangrene of the foot against the background of atherosclerosis often develop acute myocardial infarction or acute cerebrovascular accident. Anticoagulant therapy with low-molecular heparins helps reduce the risk of developing these complications. A sharp decrease in motor activity with loss of support function, especially in patients with severe concomitant pathology, often leads to the development of hypostatic pneumonia.
Long-term pain syndrome, chronic intoxication, uncontrolled use of oral analgesics and non-steroidal anti-inflammatory drugs in the preoperative period, traumatic nature of the intervention - all this predetermines the frequent development of both chronic and acute ulcers of the stomach or duodenum with subsequent bleeding or perforation. That is why all patients with critical ischemia of the lower extremities must be prescribed drugs that inhibit the production of hydrochloric acid (HCl) throughout the entire treatment period.
Early activation of patients is advisable. After various amputations, it is possible to get up and walk already on the first day of the postoperative period. If the supporting function is preserved, it is necessary to reduce the load on the limb, for which crutches are used. If the wound process proceeds favorably, the sutures are removed 10-14 days after the operation. Longer hospital treatment (1.5-2 months) is required for patients who have undergone limb revascularization and necrectomy, since tissue blood flow in the foot is restored gradually.
How is foot gangrene prevented?
Gangrene of the foot can be prevented if vascular pathology is identified in a timely manner and adequate treatment is prescribed.
What is the prognosis for foot gangrene?
Gangrene of the foot has a different prognosis. It depends primarily on the cause, as well as the level of limb amputation. Damage to various vascular basins predetermines high mortality in acute decompensated arterial insufficiency and gangrene against the background of vascular atherosclerosis. The highest mortality is characterized by amputations at the hip level (up to 40%), as well as complex interventions, including direct revascularization and necrectomy (up to 20%).
Loss of the supporting function of the leg leads to persistent disability. According to statistics, after amputation at the level of the shin, only 30% of patients use a prosthesis for the limb, at the level of the thigh - no more than 10%. Only 15% of patients use orthopedic shoes after amputations at the level of the ankle joints. The progression of the underlying disease and unresolved problems of medical and social rehabilitation after amputations lead to the fact that 2 years after the amputation of the thigh, half of the patients die, and one third of the survivors lose the second limb. After amputation, after 2 years, the mortality rate reaches 15%, 10% of patients lose the operated limb, 5% lose the contralateral limb, and 1% of patients lose both limbs.

