Medical expert of the article
New publications
Ganglioneuroma
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A ganglioneuroma is a benign tumor that develops from ganglion cells that are part of the nervous system. Ganglioneuromas can occur in various parts of the body, but most often they develop in the perispinal ganglia, neuroganglia, or other parts of the peripheral nervous system. [1] They are usually located in the retroperitoneum (32-52%) or in the posterior mediastinum (39-43%).Less frequently, gangloneuromas can also be found in the cervical region (8-9%). [2], [3] These tumors are usually slow-growing and benign, although in rare cases they may be malignant. The main localization is the mediastinum in children older than 10 years of age. Association with malignant neuroblastoma is rare and is still a topic of debate.
Symptoms of a ganglioneuroma can vary depending on its location and size. In most cases, ganglioneuromas do not cause symptoms and are discovered incidentally when being screened for other diseases or when x-rays are taken. However, if the tumor grows and begins to put pressure on surrounding tissues or nerves, the following symptoms may occur:
- Pain or discomfort in the area of the tumor.
- Numbness or weakness in areas innervated by the tumor.
- An increase in the size of the tumor that can be felt by palpation.
Diagnosing ganglioneuroma may require a variety of medical tests, including x-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI), or a tumor biopsy.
Treatment of ganglioneuroma may include surgical removal of the tumor, especially if it is causing symptoms or is suspected to be malignant. The prognosis for patients with ganglioneuroma is usually favorable, especially if the tumor is benign and successfully removed. However, it is important to discuss treatment and prognosis with your doctor based on your specific situation.
Causes of the ganglioneuromas
Here are some of the potential causes of ganglioneuroma:
- Genetic factors: Some types of ganglioneuromas may be associated with genetic mutations or inherited syndromes that increase the risk of developing tumors.
The tyrosine kinase receptor ERBB3 is one of the most frequently regulated genes in HN. [4] Furthermore, recent case series have found high expression of GATA3 in all HN tumors (100%), implying that it may be a very reliable marker of HN. [5], [6] Finally, the coexistence of HN with neuroblastoma has been associated with hemizygous deletion of 11q14.1-23.3. Indeed, the predisposition to develop neurogenic tumors may be associated with deletion of the NCAM1 and CADM1 genes, which lie in 11q. [7] However, unlike neuroblastoma, HN do not seem to show MYCN gene amplification.
- Trauma: Damage to nerves or tissues due to trauma can contribute to the development of ganglioneuroma in the nervous system.
- Inflammation: Certain infectious or inflammatory processes may increase the likelihood of ganglioneuroma formation.
- Neurodegenerative diseases: Some neurodegenerative diseases may be associated with ganglioneuroma formation.
- Neurofibromatosis: This genetic condition, such as neurofibromatosis type 1 (Recklinghausen's disease), may increase the risk of developing ganglioneuroma.
- Idiopathic Causes: In some cases, the cause of ganglioneuroma may remain unknown and it is categorized as "idiopathic".
Pathogenesis
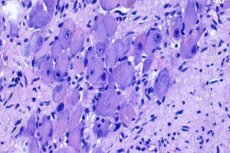
The vast majority of ganglioneuromas are histologically benign masses that can be divided into two main categories. First, "mature-type" ganglioneuromas consist of mature Schwann cells, ganglion cells, and perineural cells within a fibrous stroma, with a complete absence of neuroblasts and mitotic figures.Second, "maturation-type" ganglioneuromas consist of similar cell populations with varying degrees of maturation, ranging from fully mature cells to neuroblasts. However, the finding of neuroblasts usually indicates neuroblastoma or ganglioneuroblastoma. These types of neurogenic tumors may evolve into ganglioneuromas. [8]
Symptoms of the ganglioneuromas
Ganglioneuromas can occur in different parts of the body and have a variety of symptoms, depending on their location and size. Here are some of the common symptoms that may accompany a ganglioneuroma:
- Pain: A tumor may cause pain or discomfort in the area where it is located. The pain may be moderate to intense and may be worse when the tumor is pressed or moved.
- Tumor: In some cases, ganglioneuromas may be palpable. The tumor may be mobile and have a characteristic, soft or firm consistency.
- Swelling: Swelling may develop around the tumor, especially if it is close to adjacent structures.
- Neurologic symptoms: In some cases, ganglioneuromas can put pressure on surrounding nerve structures and cause symptoms related to the function of those nerves. For example, a tumor in the neck or back can cause symptoms related to compression of the spinal cord or peripheral nerves.
- Symptoms of neighboring organs: If a ganglioneuroma is located close to organs or blood vessels, it can put pressure on them and cause symptoms related to those organs. For example, if the tumor is in the chest area, it can cause breathing problems or heart symptoms.
Ganglioneuromas are often asymptomatic and are discovered incidentally during medical tests or examinations. Visualization studies show a partially cystic and calcified mass, so several differential diagnoses, such as neurofibroma or chordoma, must be considered. In rare cases, the tumor is hormonally active and secretion of vasoactive intestinal polypeptide may cause diarrhea. [9] In contrast to neuroblastoma, catecholamine secretion is rare in ganglioneuromas. 80% of neuroblastomas produce elevated levels of VMA and HMA, and urine tests are used as a screening method. But so far, these tests have not been found to reduce neuroblastoma mortality because additionally detected tumors are at an early stage and may undergo spontaneous regression. [10]
Forms
Adrenal ganglioneuromas are usually detected incidentally because of the widespread use of computed tomography and MRI imaging techniques. [11], [12] Specifically,ganglioneuromas account for approximately 0.3-2% of all adrenal incidentalomas [13] In most cases, ultrasound reveals a well-circumscribed, homogeneous, hypoechogenic lesion.
Usually, adrenal ganglioneuromas are hormonally silent and as a result may be asymptomatic; even if the lesion is of significant size. [14], [15] On the other hand, it has been reported that up to 30% of patients with ganglioneuromas may have elevated plasma and urine catecholamine levels, but without any symptoms of catecholamine excess. [16] In addition, it has been noted that ganglion cells can secrete vasoactive intestinal peptide (VIP), while pluripotent progenitor cells sometimes produce steroid hormones such as cortisol and testosterone. [17], [18]
Diagnostics of the ganglioneuromas
Diagnosis of ganglioneuroma involves several steps and methods:
- Physical Exam: Your doctor will perform an initial exam during which you can discuss your symptoms and medical history.
- Symptom Survey: Your doctor may conduct a detailed interview to find out the nature and duration of your symptoms, such as pain, numbness, weakness, and other neurological manifestations.
- Imaging: The following methods may be used to visualize the tumor and its exact location:
- X-ray tomography (CT) or magnetic resonance imaging (MRI): These imaging techniques help determine the size and location of the tumor, as well as its relationship to surrounding tissues and nerves.
- Ultrasound: Ultrasound can be used to visualize the tumor, especially if it is located on the surface of the body.
- Radiography: In some cases, X-rays may be used to detect a tumor, although they may be less informative than CT or MRI scans.
- Biopsy: It may be necessary to take a tissue sample from the tumor (biopsy) to definitively confirm the diagnosis. The tissue is then sent for laboratory testing to determine whether the tumor is malignant or benign.
- Neurologic examination: If ganglioneuroma is associated with neurologic symptoms, a more detailed neurologic examination may be required, including evaluation of muscle strength, sensitivity, and motor coordination.
Differential diagnosis
Differential diagnosis of ganglioneuroma can be important in determining the nature of the tumor and choosing the most appropriate treatment. Here are some diseases and conditions that may have symptoms or signs similar to ganglioneuroma and may need to be ruled out at diagnosis:
- Ganglioneuroblastoma: This is a malignant tumor that can also arise from ganglions. It can be difficult to distinguish from benign ganglioneuroma.
- Other Neuroblastic Tumors: This includes tumors such as neuroblastomas, neurogenic sarcomas, and other tumors originating from neurons and nerve cells.
- Cysts: Some cysts, such as epidermal or arthrographic cysts, may have a similar appearance to ganglioneuroma.
- Lymphadenopathy: Enlarged lymph nodes can mimic a tumor and cause similar symptoms.
- Metastasis: Tumors that metastasize to nerve tissue may also be similar to ganglioneuroma.
- Osteochondroma: Osteochondroma is a benign tumor that can develop in bones and soft tissues, and it can be similar to ganglioneuroma.
- Osteosarcoma: This is a malignant bone tumor that may have similar symptoms to tumors developing in surrounding tissues.
Studies such as educational imaging (X-ray, CT, MRI), biopsy and histologic examination of tissue samples may be necessary for differential diagnosis.
Treatment of the ganglioneuromas
Treatment for a ganglioneuroma may depend on its size, location, symptoms, and potential danger to surrounding tissues. Here are common methods and steps for treating ganglioneuroma:
-
Observation and expectation:
- In some cases, especially if the ganglioneuroma is small and does not cause symptoms or pain, the doctor may recommend simply monitoring it and not actively treating it. This decision may be made to avoid the risk of surgery, especially if the tumor does not pose a health risk.
-
Surgical removal:
- If the ganglioneuroma causes symptoms, pain, restricts movement, or threatens surrounding tissues, surgical removal of the tumor may be necessary. The therapeutic treatment for ganglioneuroma is complete removal of the tumor, whereas treatment of neuroblastoma depends on the stage of the disease and includes surgery, chemotherapy, and radiation therapy. [19], [20]
- Surgery can be performed using the classic method or laparoscopy, depending on the size and location of the tumor.
-
X-ray radiation therapy:
- In some cases, when surgical removal of a ganglioneuroma is difficult or dangerous, radiation therapy may be used to reduce the size of the tumor or control its growth.
-
Sclerosing injection:
- This method can be used to treat small ganglioneuromas, especially those in close contact with joints. A special substance is injected into the tumor, which causes it to shrink or resorb.
-
Recurrence control:
- After successful treatment, it is important to be under medical supervision to monitor for possible tumor recurrences and respond to them in a timely manner.
Treatment of ganglioneuroma should be individualized and the method of treatment should be decided according to the specific circumstances of each case.
List of authoritative books and studies related to the study of ganglioneuroma
- "Neurilemmoma" (Ganglioneuroma) is a book by J. Jay Frantz Jr., published in 2002.
- "Neurogenic Tumors: Clinical Pathology with Biochemical, Cytogenetic, and Histologic Correlations" is a book by Guido Kloppel and George F. Murphy, published in 1986.
- "Surgical Pathology of the Nervous System and Its Coverings" is a book by Kevin J. Donnelly and John R. Beyer, published in 1987.
- "Soft Tissue Tumors: A Multidisciplinary, Decisional Diagnostic Approach" is a book by John F. Fetsch and Sharon W. Weiss, published in 2007.
- "Neurofibromatosis: Phenotype, Natural History, and Pathogenesis" is an article authored by Vincent M. Riccardi, published in Annals of Internal Medicine in 1986.
Literature
- Gusev, E. I. Neurology: national guide: in 2 vol. / ed. By E. I. Gusev, A. N. Konovalov, V. I. Skvortsova. - 2nd ed. Moscow: GEOTAR-Media, 2021. - Т. 2.
- Chissov, V. I. Oncology / Ed. By V. I. Chissov, M. I. Davydov - Moscow: GEOTAR-Media, 2008. I. Chissov, M. I. Davydov - Moscow: GEOTAR-Media, 2008.

