Medical expert of the article
New publications
Epstein-Barr virus
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
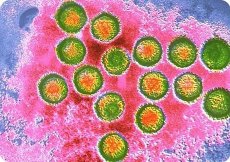
Epstein-Barr virus (EBV) causes infectious mononucleosis, which affects people of all ages, as well as a tumor of the upper jaw, Burkitt's lymphoma, found in children and adolescents in Central Africa, and nasopharyngeal carcinoma in adult men in China. Epstein-Barr virus was first identified by electron microscopy of transplanted cells derived from Burkitt's lymphoma.
The Epstein-Barr virus differs significantly from other herpes viruses in its antigenic properties. Various antigens are detected using CSC, immunodiffusion, and RIF. The earliest to be detected are the membrane antigen (MA, or LYDMA: membrane antigen, or lymphocyte detected membrane antigen), complement-fixing nuclear antigen (EBNA - Epstein-Barris nucleic antigen); the late antigen is the viral capsid antigen (VCA - virus capsid antigen).
The Epstein-Barr virus is quite original in its interaction with the host cell it infects: it causes not death, but proliferation of lymphocytes. The transformation of lymphocytes caused by the Epstein-Barr virus allows the latter to be cultivated for a long time; in this case, a positive RIF with antiserum to the Epstein-Barr virus is detected. This transformation makes lymphocytes capable of endless division. Epstein-Barr virus genomes appear in large quantities in all cells, and the nuclear antigen (EBNA) is released into the environment.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
Pathogenesis and symptoms of infectious mononucleosis
The pathogenesis of infection caused by the Epstein-Barr virus is still poorly understood. In infectious mononucleosis, the Epstein-Barr virus enters the mucous membrane of the mouth and nasopharynx, then penetrates into the regional lymph nodes, multiplies and disseminates hematogenously. In the lymph nodes, tonsils and spleen, reticular and lymphoid cells proliferate to form large mononuclear forms; focal necrosis often occurs. Lymphoid cellular infiltrates may form in the liver.
The incubation period for infectious mononucleosis is from 4 to 60 days, most often 7-10 days. The disease is characterized by gradual development: the temperature rises, a sore throat appears, nasal breathing is impaired, regional lymph nodes enlarge, and plaque appears on the tonsils. Leukocytosis is noted in the blood, one of the most characteristic signs of the disease is the appearance in the blood of atypical mature mononuclear cells of medium and large size with wide basophilic protoplasm - atypical mononuclear cells and wide-plasma lymphocytes; their number is 10-15% or more. Complications (sinusitis, pneumonia, meningitis, nephritis) are rare, the prognosis is favorable. Immunity is very specific. B-lymphocytes produce viral particles, but malignancy usually does not occur. This is associated with the appearance of specific T-killers, the target of which is the viral antigen MA on the surface of the B-lymphocyte. Natural killers and the K-cell mechanism are activated. The activity of suppressors increases, inhibiting the proliferation and differentiation of B-lymphocytes and thereby preventing the reproduction of affected cells. During recovery, memory T-cells appear, which destroy B-lymphocytes infected with the virus after their restimulation. These cells circulate in the blood of those who have recovered for life. Virus-neutralizing antibodies are also synthesized. In Burkitt's lymphoma and nasopharyngeal carcinoma, the affected cells contain multiple copies of the integrated genome of the Epstein-Barr virus, and the EBNA antigen appears in the cell nuclei. Antibodies to the capsid antigen, first of the IgM class, then of the IgG class, appear in the blood of those who have recovered. Later, antibodies to the early antigens MA and EBNA appear. The antibodies persist for life. To detect viral DNA in affected transformed cells, the DNA probe method is used.

