Medical expert of the article
New publications
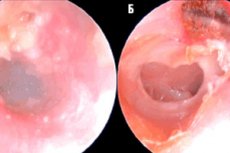
Epitympanitis
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Epitympanitis is a medical term that can be associated with a variety of conditions and diseases related to the ear and hearing. The exact meaning of the term can depend on the context and medical specialty. Here are a few possible interpretations of the term:
- Epitympanitisas osteomyelitis: In otolaryngology (otorhinolaryngology), the term "epitympanitis" can be used to describe an inflammatory process in the bone tissue of the skull box that can affect the auditory ossicleas well. This condition is sometimes referred to as "osteomyelitis of the epitympanum".
- Epitympanitis as a symptom: Epitympanitis can also be used as a symptom in the diagnosis of ear diseases. It may indicate an inflammatory process or other abnormalities in the ear and auditory ossicles.
- Link to meningitis: In rare cases, the term "epitympanitis" may be used to describe inflammation of the auditory bone associated with meningitis (inflammation of the membranes of the brain and spinal cord).
To determine the exact meaning of the term "epitympanitis" and its relationship to a specific disease or symptom, you should consult a physician, particularly an otorhinolaryngologist (ENT doctor). He or she will be able to perform the necessary examination and diagnosis and provide recommendations for treatment and management of the condition.
Causes of the epitympanitis
The causes of epitympanitis can be varied and may include:
- Viral infections: Some viruses can infect the neuroepithelium, leading to the development of epitympanitis. An example is herpesvirus.
- Autoimmune diseases: Some autoimmune diseases can cause inflammation and damage to the neuroepithelium.
- Toxins and chemicals: Exposure of epithelial neurons to toxins or chemicals can lead to the development of epitympanitis.
- Genetic factors: Certain disorders of a genetic nature may predispose to the development of this condition.
- Tumors: The presence of tumors in the epithelium or in nearby tissues may affect the neuroepithelium.
- Trauma: Mechanical trauma or injury can result in neuroepithelial damage.
- Other diseases: Some other diseases, such as diabetes, may affect the neuroepithelium and contribute to the development of epitympanitis.
Symptoms of the epitympanitis
Symptoms of epitympanitis may include:
- Pain: Patients may experience pain in the ear area, which may be moderate to severe. The pain may be worse when pressure is applied to the ear area or when chewing.
- Ear discharge: There may be a discharge from the ear. It may be liquid or pus. The pus may have a distinctive odor.
- Hearing loss: Due to inflammation and dysfunction of the middle ear, patients may experience temporary or permanent hearing loss.
- Itchingand discomfort: You may experience itching, discomfort, or a feeling of fullness inside the ear.
- General symptoms: In some cases, symptoms of epitympanitis may be accompanied by general symptoms such as fever or weakness.
Stages
Epitympanitis is an inflammatory disease of the middle ear that can have different stages depending on the nature and severity of the inflammation. Common stages of epitympanitis include:
- Initial stage (catarrhal epitympanitis): In this stage, the inflammation begins with catarrhal changes in the middle ear mucosa. The patient may experience mild pain or discomfort in the ear. There is usually no pus or serous discharge from the ear in this stage, and hearing is usually not severely impaired.
- Otitis mediastage (serous epitympanitis): In this stage, otitis media may develop with the secretion of a serous (liquid) discharge from the middle ear. This may cause temporary hearing loss.
- Cavitary stage (purulent epitympanitis): In this stage, the inflammation becomes more severe and purulent contents begin to collect in the ear. The patient may experience ear pain and hearing loss. Pus may come out of the ear.
- Chronic stage (chronic epitympanitis): If the inflammation does not respond to treatment or keeps coming back, it may become chronic. In this stage, the inflammation and pus discharge may periodically increase and then improve. Chronic epitympanitis can cause more serious consequences such as damage to the eardrum and permanent hearing loss.
Forms
Epitympanitis can be acute or chronic and has different characteristics. I will describe them in more detail:
-
Acute epitympanitis:
- Characteristics: Acute epitympanitis is an inflammation of the mucous membrane of the middle ear that develops rapidly and presents with abrupt symptoms.
- Symptoms: Symptoms of acute epitympanitis may include ear pain, ear discharge, fever, hearing loss, and general malaise.
- Causes: Acute epitympanitis is most often associated with infections, such as bacterial or viral infections, that can enter the middle ear through the pharynx (eustachian tube).
- Treatment: Treatment for acute epitympanitis may include antibiotics for bacterial infection, anti-inflammatory medications, pain medications, and ear care recommendations.
-
Chronic purulent epitympanitis:
- Characteristics: Chronic suppurative epitympanitis is a prolonged and often recurrent inflammation of the middle ear mucosa with pus discharge.
- Symptoms: Symptoms of chronic purulent epitympanitis may include ear pain, purulent discharge from the ear, hearing loss, sometimes fever, and general malaise.
- Causes: Causes of chronic epitympanitis may include long-term infections, anatomical features of the ears, and other factors.
- Treatment: Treatment of chronic purulent epitympanitis depends on its cause and severity. The doctor may prescribe antibiotics, ear washing, surgery (e.g., myringotomy to remove pus clots), or other methods depending on the situation.
Epitympanitis can take several forms, depending on the characteristics of the disease and the middle ear structures involved. Here are some of the forms of this disease:
- Exudative (secretory) epitympanitis: This is the most common form. In this form of epitympanitis, there is a buildup of mucus and fluid in the middle ear due to impaired drainage and ventilation of the ear tube. This can be caused by infection, allergic reactions, anatomical features, or other factors.
- Purulent (pulsatile) epitympanitis: This form is characterized by the presence of a purulent secretion in the middle ear. It may be caused by a bacterial infection that leads to inflammation and collection of pus in the ear cavity.
- Atelectatic (plastic) epitympanitis: This form is associated with the formation of atelectasis in the middle ear, which means that the tympanic membrane (tympanic membrane) becomes dense and stiff. This can be caused by chronic inflammatory processes and impaired ventilation of the ear tube.
- Combined epitympanitis: This is a form that includes several of the above characteristics.
- Adhesive epitympanitis: This form is associated withadhesions and scarring in the middle ear, which can occur after surgery or with chronic inflammation.
Complications and consequences
Epitympanitis can have a variety of complications and consequences that depend on the severity of the condition, the cause of the condition, and the effectiveness of treatment. Some of the possible complications and consequences of epitympanitis include:
- Vision impairment: Epitympanitis, which affects the neuroepithelium of the eye, can lead to visual impairment. This can include blurred vision, impaired color perception, and other visual impairment.
- Pain and discomfort: Patients with epitympanitis may experience pain and discomfort in the area of the affected neurons.
- Dry Eye Syndrome: As the neuroepithelium is destroyed, patients may develop dry eye syndrome, which is characterized by a sensation of dryness, burning and discomfort in the eye.
- Refractive problems: Epitympanitis can cause changes in the refraction of the eye, which may require correction with glasses or contact lenses.
- Eye infections: Irritation and damage to the neuroepithelium can make the eye more vulnerable to infections.
- Deterioration of quality of life: Epitympanitis can have a negative impact on the patient's quality of life due to restricted visual function and discomfort.
- Spread of infection: If epitympanitis is due to infection, it can spread to neighboring tissues and cause more serious complications.
- Surgical treatment: In some cases, epitympanitis may require surgical intervention, for example, to remove affected tissue.
Diagnostics of the epitympanitis
Diagnosing epitympanitis (osteomyelitis of the epitympanum) usually involves several steps:
- Clinical Exam: The doctor will examine and talk to the patient to learn about symptoms that may indicate the presence of epitympanitis. These may include ear pain, ear discharge, hearing loss, and other symptoms.
- Visual examination of the ears: The doctor will examine the ears with an oropharyngoscope or other instrument to look for inflammatory signs or changes in the ear area.
- Audiometry: Audiometric tests may be performed to assess hearing to determine the degree of hearing loss.
- Computed tomography (CT) or magnetic resonance imaging (MRI): These educational techniques can be used to look in more detail at the bones and tissues in the ear and skull region.
- Laboratory tests: Sometimes laboratory tests of blood and other bodily fluids may be needed to detect inflammation and infection.
- Biopsy: In some cases, it may be necessary to take a tissue sample for biopsy and then analyze it in a laboratory.
- Consultation with other specialists: Depending on the diagnostic results, other specialists such as a neurosurgeon, infectious disease specialist or oncologist may need to be consulted.
Computed tomography (CT) scans can be useful in the diagnosis and evaluation of epitympanitis (chronic otitis media) and its complications. CT scans of the middle ear may reveal the following characteristics of epitympanitis:
- Infection and inflammation: CT scans can help visualize signs of infection and inflammation in the middle ear, such as the presence of fluid, pus or mucus, and swelling of the mucous membrane.
- Changes in the ear cavity: CT scans can help identify structural changes in the middle ear, such as thickening of the tympanic membrane, the presence of atelectasis (plastic epitympanitis), or impaired ventilation of the ear tube.
- Complications: CT can also be used to detect complications associated with epitympanitis, such as middle ear osteomyelitis (inflammation of the middle ear bones) or cholesteatoma (abnormal growth in the middle ear).
Diagnostic CT scans are usually performed in specialized centers or clinics. After receiving the CT scan results, the doctor will be able to determine the extent and nature of the disease and develop a treatment plan depending on the changes detected.
Differential diagnosis
The differential diagnosis of epitympanitis (chronic otitis media) involves identifying the differences between this condition and other conditions that may exhibit similar symptoms. Below are some conditions to consider in the differential diagnosis:
- Acute otitis media: Acute otitis media may have symptoms similar to epitympanitis, but it is characterized by an abrupt onset of symptoms and an active middle ear infection.
- Allergicrhinitis: Allergic runny nose can cause stuffy ears and increased mucus in the ears. However, the main symptom here is related to nasal mucus and allergic manifestations.
- Gastroesophageal reflux (GERD): Reflux of acid from the stomach into the larynx and ear tube can irritate the ears and lead to symptoms similar to epitympanitis. Complaints of heartburn and dysphagia may also indicate GERD.
- Upper respiratory tract infections: Upper respiratory tract infections such as viral rhinitis or sinusitis can cause ear stuffiness and even ear discomfort, but inflammation is usually limited to the upper respiratory tract.
- Osteosclerosis of the inner ear: This is a rare condition of the inner ear that can cause gradual hearing loss and long-term ear pain that resembles the symptoms of epitympanitis.
Differential diagnosis requires seeing a specialist, such as an otolaryngologist, to perform the necessary tests, including audiometry (hearing measurement) as well as visual examination of the ear using special instruments. Based on the diagnostic results, the correct treatment will be determined and an accurate diagnosis will be established.
Mesotympanitis and epitympanitis are two different ear-related conditions, and they have different characteristics and causes.
- Mesotympanitis is an inflammation of the middle ear. It can be acute (acute mesotympanitis) or chronic (chronic mesotympanitis). Acute mesotympanitis is most often caused by infections, both bacterial and viral. Chronic mesotympanitis can be caused by long-term infections or other factors such as allergies or anatomical features of the ears. Treatment for mesotympanitis may include antibiotics, anti-inflammatory medications, and sometimes surgery may be required.
- Epitympanitis (or epithelial intraepithelial neurotyopia) is a condition involving damage to neurons located in the epithelium, which can lead to impaired neuroepithelial function. The causes of epitympanitis can be varied and can include viral infections, autoimmune diseases, trauma, and other factors. Treatment for epitympanitis depends on its cause and may include antiviral medications, anti-inflammatory drugs, and other methods aimed at improving the condition of the neuroepithelium.
Who to contact?
Treatment of the epitympanitis
Treatment for epitympanitis depends on its cause, severity and specific symptoms. Epitympanitis can be caused by a variety of factors such as viruses, autoimmune processes, or injury, so treatment will focus on addressing the underlying cause. Here are some treatments that can be used:
- Treatment of the underlying condition: If epitympanitis is associated with a viral infection or autoimmune disease, your doctor may prescribe medication to combat that underlying cause.
- Anti-inflammatorytherapy: Anti-inflammatory drugs such as nexatin and glucocorticoids can be used to reduce inflammation and pain.
- Vision maintenance: In cases of severe visual impairment, corrective devices such as glasses or contact lenses may be required.
- Symptomatic treatment: If the patient is experiencing pain or discomfort, the doctor may recommend medication to relieve symptoms.
- Physical therapy: In some cases, physical therapy can help restore neuronal function and improve your overall condition.
- Surgery: In rare cases, surgical intervention may be necessary, for example, to remove diseased tissue.
- Follow your doctor's recommendations: It is important to follow your doctor's recommendations and have regular medical check-ups to monitor the condition of your eye and the effectiveness of treatment.
Surgical treatment
Surgery for epitympanitis may be considered only in certain cases where conservative treatment is ineffective or if there is a need for surgery to improve visual function or remove diseased tissue. However, surgery depends on the specific situation and the cause of the epitympanitis.
Possible surgical interventions for epitympanitis may include:
- Excision of affected tissue: The doctor may decide to remove affected neuroepithelial tissue or tumors if they are the underlying cause of epitympanitis.
- Reconstruction of damaged tissue: In rare cases, if neuroepithelial structures have been damaged by trauma or other factors, surgical reconstruction may be required.
- Electrodeimplantation: In some cases, electrode implants may be used to stimulate neurons and restore function.
- Keratoplasty: If epitympanitis is accompanied by severe corneal abnormalities, a corneal transplant (keratoplasty) may be necessary.
Clinical Guidelines
Clinical guidelines for the treatment of epitympanitis may vary depending on the cause and severity of the condition. Because epitympanitis is a relatively rare condition and requires an individualized approach to treatment, it is important to follow the recommendations of the physician who is diagnosing and monitoring your condition. However, below are some general clinical guidelines:
- Specialist Consultation: If you suspect epitympanitis or if you have symptoms such as vision changes or eye pain, see an ophthalmologist or neurologist for diagnosis and consultation.
- Investigations and Diagnosis: Your doctor may perform a variety of investigations and tests, including neuroimaging (e.g., MRI of the head) and ophthalmologic tests to diagnose and determine the cause of epitympanitis.
- Treatment of the Underlying Disease: If epitympanitis is caused by other medical conditions, such as viral infections or autoimmune diseases, your doctor will prescribe treatment to manage these underlying problems.
- Anti-inflammatory and Immunomodulatory Drugs: In some cases, anti-inflammatory drugs and immunomodulatory drugs may be prescribed to reduce inflammation and decrease symptoms.
- Physical Therapy and Rehabilitation: Physical therapy exercises and rehabilitation can help restore neuroepithelial function and improve overall condition.
- Vision correction: If epitympanitis is accompanied by visual impairment, your doctor may recommend corrective devices such as eyeglasses or contact lenses.
- Regular Monitoring: It is important to monitor the condition of the eye on a regular basis and visit your doctor to monitor and adjust treatment if necessary.

