Medical expert of the article
New publications
Epiglottitis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Acute epiglottitis is a disease of the larynx caused by Haemophilus influenzae type b, leading to acute respiratory failure (acute respiratory failure of the obstructive type); rapidly progressing inflammation of the epiglottis and surrounding tissues of the laryngopharynx, characterized by increasing symptoms of difficulty breathing as a result of swelling of the epiglottis and aryepiglottic folds.
Epidemiology
The source and reservoir of infection is a person. The disease is transmitted by airborne droplets. The pathogen is excreted from the nasopharynx of 80% of healthy people. Healthy carriage can last from several days to several months. Most often, children aged from six months to 4 years fall ill, less often newborns, older children and adults. The frequency of carriage of Haemophilus influenza type B among children in Russia in normal times is no more than 5%, during an epidemic it increases sharply.
Causes epiglottitis
The main causative agent of epiglottitis in children (up to 90%) is Haemophilus influenzae (type B). In addition to Haemophilus influenzae, the following pathogens have been identified (with them, the disease occurs in a milder form): Staphylococcus aureus, Streptococcus pyogenes, Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus parainfluensae (Pfeiffer's bacillus). The latter belongs to the genus Haemophilus, which unites 16 species of bacteria, 8 of which are pathogenic for humans. The most dangerous are Haemophilus influenza, which causes damage to the respiratory tract, skin, eyes, epiglottis, endocarditis, meningitis, arthritis, and Haemophilus ducteyi.
Risk factors
Risk factors for the development of acute epiglottitis in children:
- age from 6 months to 4 years,
- male gender (boys get sick 1.5-2 times more often than girls),
- previous allergization,
- perinatal encephalopathy,
- preventive vaccinations that coincide in time with the onset of the disease,
- concomitant lymphogranulomatosis (and associated chemotherapy), sickle cell anemia, agammaglobulinemia,
- post-splenectomy condition.
Children aged 2-12 years are more likely to get sick, and adults are less likely to get sick.
Symptoms epiglottitis
Acute epiglottitis often begins with a respiratory infection, minor sore throat, phonation disorders, difficulty swallowing, and fever. Symptoms of acute epiglottitis can quickly progress to complete obstruction of the larynx, which develops within 4-6 hours from the moment of onset. In this case, the child is in a sitting position with the chin thrust forward; the cervical spine is maximally extended; the tongue protrudes from the oral cavity; profuse salivation. Coughing occurs rarely.
Characteristic features include sudden rise in temperature, severe sore throat, rapidly progressing airway obstruction, and increased salivation. Acrocyanosis, sweating, and pale skin with a gray tint are expressed. The child is in a forced semi-sitting position. The head is in a characteristic "sniffing" position, "grabbing" air with the mouth. Stenotic breathing, all accessory muscles are involved, the voice is hoarse, the cough is rare, quite sonorous, but dry and unproductive. The child cannot swallow. When trying to lay the child on his back, respiratory failure increases. Vomiting is possible, including "coffee grounds". Heart sounds are muffled, tachycardia, pulse is weak. On examination, the pharynx is hyperemic, filled with a large amount of thick and viscous mucus and saliva, occasionally an enlarged cherry-red epiglottis can be seen.
Anxiety is replaced by a sharp increase in cyanosis, and hypoxic coma develops with a fatal outcome.
Manifestation of the disease and severe airway obstruction are the hallmarks of epiglottitis.
 [ 15 ]
[ 15 ]
Where does it hurt?
Forms
There are edematous, infiltrative and abscessing forms of acute epiglottitis. Infiltrative and abscessing forms can lead to the development of sepsis. Against the background of a septic condition, hemophilic meningitis often develops. As the symptoms of acute epiglottitis subside, stenosis of the larynx and subglottic space, purulent laryngotracheobronchitis come to the fore.
Diagnostics epiglottitis
Diagnosis of acute epiglottitis in children is based on anamnesis data, clinical picture of the disease, visualization of the epiglottis, etiologic diagnosis of blood cultures and a smear from the oropharynx.
When inhaling and exhaling, sounds with a predominance of low tones are heard. Severe stridor, retraction in the area above and below the sternum with signs of cyanosis indicate a threat of complete obstruction of the airways.
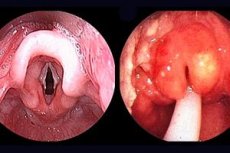
On examination of the pharynx: dark cherry infiltration of the root of the tongue, swollen and inflamed epiglottis.
Laryngoscopy: edematous arytenoid cartilages, inflamed supraglottic structures of surrounding tissues. In some cases, the study may cause laryngospasm in the child, requiring immediate intervention. The diagnosis is established by direct examination of the pharynx and larynx.
Radiography is performed only in cases of doubtful diagnosis and provided that the child is accompanied by a doctor who knows the intubation method. Diagnostic signs - epiglottis shadow with an increased volume of swollen soft tissue, rounded and thickened edge of the aryepiglottic folds.
What do need to examine?
How to examine?
Differential diagnosis
Differential diagnostics are carried out with the following diseases:
- acute stenosing laryngotracheitis (false croup syndrome),
- retropharyngeal abscess,
- abscess of the root of the tongue,
- BA,
- thermal and chemical lesions of the oropharyngeal mucosa,
- foreign body of the larynx,
- subglottic hemangioma,
- laryngeal papillomatosis,
- multiple soft tissue tumors of the oropharynx,
- bronchiolitis,
- whooping cough.
Who to contact?
Treatment epiglottitis
Children with epiglottitis require emergency hospitalization. Transportation is performed only in a sitting position. If necessary, tracheal intubation. Amoxicillin/clavulanate [40 mg/(kg x day) | or ceftriaxone |100-200 mg/(kg x day)| is administered parenterally. The extreme measure is tracheostomy.
The main directions of treatment of acute epiglottitis:
- maintaining the patency of the upper respiratory tract,
- rational antibiotic therapy,
- infusion therapy,
- immunocorrective therapy.
It is necessary to emphasize the danger of inhalation with warm humidified mixtures. Indications for hospitalization of the patient in the intensive care unit are increasing anxiety, progression of dyspnea, intractable hyperthermia, hypercapnia. An attempt at tracheal intubation by emergency doctors may end fatally, so it is necessary to deliver the patient to the nearest pediatric intensive care unit. However, problems with tracheal intubation are possible in the intensive care unit as well. It is necessary to be prepared to impose a microtracheostomy for high-frequency ventilation of the lungs.
It is dangerous to place the patient in a horizontal position, as this may lead to obstruction of the airways by a sunken epiglottis. Tracheal intubation should be performed in a semi-sitting position. The use of inhalation anesthetics, especially halothane, for anesthesia poses a certain danger. Inhalation of sevoflurane and rapid access to a peripheral vein are more rational. Midazolam at a dose of 0.3-0.5 mg/kg and sodium oxybutyrate at a dose of 100 mg/kg are used for sedation.
Puncture of the central vein is performed after restoration of airway patency.
Antibacterial therapy
Use second-generation cephalosporins cefuroxime 150 mg / (kg x day), third-generation cephalosporins - cefotaxime 150 mg / (kg x day), ceftriaxone 100 mg / (kg x day), ceftazidime 100 mg / (kg x day) in combination with aminoglycosides nithromycin 7.5 mg / (kg x day). Use carbapenems - meropenem (meronem) 60 mg / (kg x day) in three doses. The duration of the course of antibacterial therapy is at least 7-10 days of fluid in the vascular bed and providing patients with a sufficient amount of calories and plastic substances.
As pulmonary gas exchange improves and the patient's general condition stabilizes, the focus of therapy should be shifted to meeting energy and plastic needs using parenteral nutrition or mixed (parenteral-enteral nutrition).
 [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
Immunocorrective therapy
- normal human immunoglobulin for intravenous administration up to 1 g/kg for 3 days,
- pentaglobin 5 ml/kg once.
When treating community-acquired pneumonia, a differentiated approach to the choice of antibiotics should be taken into account, taking into account the age, severity of the condition, and the presence of concomitant diseases. When choosing an antibiotic for a patient with nosocomial pneumonia, the nature of the microflora of the department (general profile department or intensive care unit), the use of artificial ventilation, and the time of development of ventilator pneumonia are taken into account.
Community-acquired pneumonia
Drugs of choice
- amoxicillin + clavulanic acid or ampicillin + sulbactam in combination with macrolides (for mild cases),
- cephalosporins III-IV generation + macrolides intravenously + rifampicin (in severe cases)
Alternative drugs
- intravenous fluoroquinolones, carbapenems
Nosocomial pneumonia
Drugs of choice
- Amoxicillin + clavulanic acid, ampicillin + sulbactam,
- II-III generation cephalosporins
Alternative drugs
- fluoroquinolones, cefepime + aminoglycosides, vancomycin.
Antioxidant therapy (ascorbic acid, vitamin E)
Treatment of complications
In non-cardiogenic pulmonary embolism, artificial ventilation, defoamers (ethyl alcohol), intravenous administration of saluretics, and aminophylline are used.
In case of pyopneumothorax, pleural drainage is installed. In case of myocardial dystrophy, drugs with cardiotropic action are prescribed - dobutamine 10-20 mcg/(kg x min), dopamine 5-20 mcg/(kg x min).
Использованная литература

