Medical expert of the article
New publications
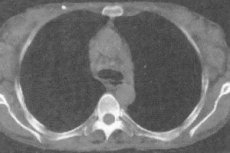
Mediastinal lymph node enlargement
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The role of the vessels and lymphatic capillaries is to absorb and remove protein fluid from the bed of the blood capillaries and return it to the venous circulation. Along the lymphatic system, near the blood vessels and large veins, lymph nodes are grouped (there are more than 600 of them in the human body) - pinkish-gray round or oval formations of approximately 0.5-50 mm, including in the mediastinum - the middle section of the chest, where the most important human organs are located: the heart, bronchi, lungs, pulmonary artery and veins, etc. They are a kind of filtration chamber for lymph and serve as a barrier to various infections. Enlargement of the mediastinal lymph nodes or lymphadenopathy is a response to a pathological process occurring in the lungs, or a consequence of malignant tumors in anatomically adjacent organs: the mammary gland, larynx, thyroid gland, gastrointestinal tract.
Epidemiology
According to statistics, mediastinal lymphadenopathy is diagnosed in 45% of patients. Since this disease is associated with such diagnoses as cancer, pneumonia, sarcoidosis, the data related to these pathologies also provide an idea of the epidemiology of enlarged mediastinal lymph nodes. More than 14 million people have been registered in the world with lung cancer, and about 17 million per year with pneumonia. Sarcoidosis is distributed unevenly in different countries, so in 40 cases per 100 thousand people it is detected in Europe and 1-2 in Japan.
Causes mediastinal lymph node enlargement
The reason for the enlargement of the mediastinal lymph nodes is the penetration of pathogenic microbes into them, which activate white blood cells that fight infection. The primary ones are bronchopneumonia, tuberculosis, sarcoidosis, malignant tumors. Malignant pathologies include lymphomas that affect not only the mediastinal lymph nodes, but also other areas, metastases of carcinomas - tumors of epithelial tissues.
Enlarged lymph nodes in lung cancer
Lung cancer is a malignant tumor that develops in the epithelial layers of the bronchi and bronchioles in 95% of cases. Less often, neoplasms affect the cells of the pleura or accessory tissues of the lungs. Of all types of cancer, this is the most common cause of death worldwide. There are 4 stages of cancer depending on the size of the tumor, its spread to adjacent tissues, and the presence of metastases in the lymph nodes and other organs. At stage 1 of cancer, the lymph nodes are not involved in the pathological process. Enlargement of the lymph nodes in lung cancer is observed from stage 2. First, the bronchial nodes are affected, at stage 3a, the mediastinal lymph nodes on the opposite side are involved, at stage 3b, the bronchopulmonary lymph nodes on the opposite side and the supraclavicular lymph nodes are involved.
Enlarged mediastinal lymph nodes after bronchopneumonia
Bronchopneumonia is an acute infectious disease affecting the walls of the bronchioles. It often occurs after an acute respiratory viral infection, but it can also be a primary disease. Enlargement of the lymph nodes after bronchopneumonia occurs due to the involvement of the lymphatic and vascular systems in the inflammatory process, including the lymph nodes of the mediastinum. As a rule, with this disease they are moderately enlarged.
Risk factors
Risk factors for enlarged mediastinal lymph nodes include smoking, long-term exposure to chemicals, harmful vapors, dusty and polluted air, and gases. Hypothermia leads to decreased immunity and various viral infections that can be complicated by pneumonia. A hereditary factor in the development of the disease, as well as long-term exposure to various medications, cannot be ruled out.
 [ 16 ]
[ 16 ]
Pathogenesis
Lymph nodes exist to filter various infectious agents from the tissues of our body, so they are located in strategically important places of the body. Having fallen into such "traps", white blood cells are activated, which fight the penetrating infection. The pathogenesis of the disease lies in the increased proliferation of lymphocytes - protective cells to activate the fight against foreign elements if the existing ones do not cope. As a result, the lymph nodes increase in size and become denser.
Symptoms mediastinal lymph node enlargement
Symptoms of enlarged mediastinal lymph nodes have a clearly expressed clinical picture.
The first signs are intense and sharp pains in the chest, sometimes they can be felt in the shoulder and neck. Hoarseness of the voice, cough, dilated pupils, sunken eyeballs, tinnitus and headaches occur. Swelling of the veins in the neck is possible, the passage of food is difficult. Chronic course of the disease is characterized by fever, tachycardia, swelling of the extremities, weakness, sweating.
Stages
Based on the time of the disease, three stages of development of the disease are distinguished:
- sharp;
- chronic;
- recurring.
The latter is associated with a resurgence of the disease.
 [ 22 ]
[ 22 ]
Enlarged lymph nodes in the root of the lung
Enlargement of the lymph nodes in the root of the lung is one of the most common pathologies of this part of the organ. Unilateral lesions are most often caused by tuberculous bronchoadenitis, cancer metastases and malignant lymphomas, bilateral lesions are caused by stage 1 sarcoidosis, which is characterized by the formation of granulomas in the lymph nodes.
 [ 23 ]
[ 23 ]
Enlarged intrathoracic lymph nodes of the lungs
One of the reasons for the enlargement of the intrathoracic lymph nodes of the lungs, as well as in their roots, is pulmonary tuberculosis. Lymphoid tissue grows, and the lymph node increases accordingly. Then signs of specific inflammation appear.
A slight increase in nodes (up to 1.5 cm) is called bronchoadenitis. When inflammation occurs around the lesion, infiltrative bronchoadenitis occurs, which is localized mainly on one side. Even with a bilateral location, it is asymmetrical. Tissue death in the form of a cheesy mass is characteristic of tumor-like or tumorous bronchoadenitis.
Another cause of pulmonary lymphadenopathy is a benign disease - sarcoidosis, which is characterized by the formation of epithelioid granulomas in the lymph nodes. This pathology is more common in women aged 20-40 years. The nature of this disease is not yet clear, some scientists associate its occurrence with infectious agents, others - with a genetic factor.
Enlargement of the intrathoracic lymph nodes of the lung can also be caused by trauma to the organ.
Complications and consequences
Since enlargement of the mediastinal lymph nodes is most often secondary and develops against the background of a number of the above-mentioned diseases, the consequences and complications depend on the underlying pathology. Enlargement of the mediastinal lymph nodes can lead to pulmonary artery thromboembolic disease, sepsis. In any case, early detection of the problem, even with malignant tumors, makes them not as life-threatening to a person as in the later stages of the disease.
Diagnostics mediastinal lymph node enlargement
Diagnosis of enlarged mediastinal lymph nodes is carried out on the basis of the disease history, tests, instrumental and differential diagnostics, since the lymph nodes inside the chest are not visually accessible.
Tests
For laboratory confirmation of the suspected diagnosis, a general and biochemical blood test, a blood microreaction (test for syphilis) are performed. A lymph node biopsy is also performed. In case of malignant neoplasms, leukocytosis, a decrease in the total number of lymphocytes, an increase in ESR, and anemia are detected in the blood.
If lymphogranulomatosis or leukemia is suspected, a bone marrow puncture is performed. If tuberculosis is suspected, a sputum analysis is performed. Sarcoidosis also changes the general blood and urine analysis, biochemical, including a decrease in the level of erythrocytes, an increase in monocytes, lymphocytes, eosinophils, ESR. There are also specific tests for this disease: a significant increase in the ACE enzyme in venous blood or calcium in the urine confirms the presence of pathology.
 [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ]
[ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ]
Instrumental diagnostics
In addition to X-ray examination of the mediastinum, which is characterized by a two-dimensional flat image and is unable to provide a complete picture of all its organs, including due to insufficient display contrast, there are other methods of instrumental diagnostics.
X-ray is a modern and effective examination that displays a more accurate three-dimensional image on the screen. It helps to clarify the structure and contours of the darkening, if it is a neoplasm - the degree of its growth into the mediastinum, the relationship to other organs. Informative methods include computed tomography, magnetic resonance imaging, and ultrasound examination.
Bronchoscopy is a method using an endoscope to obtain material for biological research in case of suspected tuberculosis, to examine the trachea and bronchi. Endoscopy is used to examine enlarged lymph nodes.
Enlarged lymph nodes on mediastinal x-ray
In the absence of a pathological process in the lungs, the lymph nodes are not visible on the image. Enlarged lymph nodes on an X-ray of the mediastinum look like a "pathological shadow" and give an idea of the localization of the tumor, shape, outlines, mobility, and relationship with neighboring organs. Enlarged lymph nodes may be indicated by compaction, expansion of the roots of the lungs on the image. This picture is typical for bronchitis, pneumonia, and smokers' lungs. Tuberculosis of the intrathoracic lymph nodes is determined using a survey X-ray, and the clinical picture depends on the extent of their damage, as evidenced by the shadow of the root of the lung, the outline of its outer contour, and other characteristics. For a more accurate study of the anatomy of the mediastinum, various contrast methods of fluoroscopy are used - pneumomediastinography (using gas through puncture), angiocardiography (using iodine), bronchography (various contrast agents), and examination of the esophagus using barium.
What do need to examine?
How to examine?
Differential diagnosis
The task of differential diagnostics is to correctly recognize pathology among all possible diagnoses: tuberculosis, tumors, sarcoidosis, lymphocytic leukemia, lymphogranulomatosis, viral infections, pneumonia and other diseases leading to an increase in lymph nodes in the mediastinum.
Who to contact?
Treatment mediastinal lymph node enlargement
Treatment of enlarged mediastinal lymph nodes directly depends on the diagnosis. Let's consider the therapy of the most possible pathologies. Thus, treatment of sarcoidosis is effective with steroid inhalations. Treatment of tuberculosis involves a long period (up to six months) and is carried out in a hospital, after which it continues on an outpatient basis for up to one and a half years. Anti-tuberculosis therapy includes a combination of 3-4 anti-tuberculosis drugs in combination with immunomodulators, metabolic therapy, and physiotherapy. Various neoplasms most often require surgical intervention in combination with chemotherapy and radiation. In case of mediastinal lymphoma and late stages of tumors, only conservative treatment is used.
Medicines
Prednisolone is initially used to treat sarcoidosis.
Prednisolone is a synthetic analogue of the hormones cortisone and hydrocortisone. It is an anti-inflammatory, antitoxic, anti-allergic drug. It is available in tablets and ampoules. The dose is determined individually, but usually starts at 20-30 mg per day during an exacerbation. In chronic cases - 5-10 mg. They can initially prescribe intravenously (30-45 mg), and with positive dynamics, switch to a reduced dose in tablets. Side effects are sometimes expressed as excessive hair growth, obesity, formation and perforation of ulcers. Prednisolone is contraindicated in pregnancy, in old age, with hypertension, ulcerative lesions of the gastrointestinal tract.
For inhalations, large doses of fluticasone and budesonide are used. If the pathology does not respond to treatment, azathioprine, chrysanol, and cyclosporine are prescribed.
Azathioprine - refers to drugs that correct immune processes. Release form - tablets. It is recommended to take 1-1.5 mg per kilogram of weight per day. Nausea, vomiting, toxic hepatitis may occur. It is contraindicated in leukopenia.
Combination therapy for tuberculosis may include the following drug combinations: isoniazid, pyrazinamide, rifampicin or isoniazid, rifampicin, ethambutol. During outpatient treatment, a combination of two drugs is prescribed: isoniazid with ethambutol, or with ethionamide, or with pyrazinamide.
Isoniazid is prescribed for the treatment of all forms and localizations of tuberculosis, both in adults and children. It is available in tablets, powders, solutions. The methods of administration are different: orally, intramuscularly, intravenously, intracavernously, with inhalation. The dose for each case is individual, on average up to 15 mg once after meals 1-3 times a day. Side effects may occur in the form of nausea, vomiting, dizziness, drug-induced hepatitis, breast enlargement in men and bleeding in women. Contraindicated in patients with epilepsy, high blood pressure, liver disease, coronary heart disease, etc.
Rifampicin is a broad-spectrum antibiotic, available in pharmacies in capsules and ampoules with a porous mass. The capsules are taken on an empty stomach half an hour to an hour before meals, and are administered intravenously by drip only to adults, using sterile water and glucose to prepare the solution. For adults, the daily dose is 0.45 g, for children 10 mg / kg. The course of treatment is a month and is carried out under the close supervision of doctors, since there may be allergic reactions, decreased blood pressure, indigestion, liver and kidney problems. It is not prescribed to pregnant women, children under 3 years of age, with hypersensitivity to the drug.
Vitamins
Enlarged mediastinal lymph nodes, no matter what the cause, require a balanced diet rich in vitamins and microelements. The list of healthy foods is very large, including lean meats, vegetables (zucchini, carrots, asparagus, celery, cabbage, cucumbers, eggplants, onions, garlic, sweet peppers), various fresh and dried fruits, nuts, cereals, cottage cheese, yogurts, fresh juices and other products. Rosehip infusions, beef liver, butter, citrus fruits will help boost immunity. For sarcoidosis, there is a limitation in calcium intake, but vitamins E, D, C, omega-3 are necessary for a sick organism.
Physiotherapy treatment
Physiotherapeutic treatment is not used for tumor-related enlargement of the mediastinal lymph nodes. UHF therapy on the thymus gland is effective for patients with sarcoidosis. Pulmonary tuberculosis is treated with laser, ultrasound, and inductothermy. These methods increase blood circulation in the lungs, thereby enhancing the effect of anti-tuberculosis drugs. They are contraindicated in acute cases of the disease, hemoptysis, and tumor processes.
Folk remedies
Traditional medicine recipes for treating various lung diseases use herbs, bee products, animal and vegetable fats, nuts, etc. Here are some of them:
- mix pork fat (200g), butter (50g), honey (tablespoon), cocoa (50g), egg yolks (4 pcs.), cream (300g). Beat the resulting mass in a blender and boil until thick sour cream. Drink cooled 1 tablespoon 3 times a day;
- 2 tablespoons of lycopodium and a pack of softened butter are added to half a liter of honey, mixed thoroughly. Take several times a day, one tablespoon at a time;
- beet juice, aloe, honey, Cahors wine (100g each), a spoonful of pork fat are mixed and infused for 2 weeks, daily portion 40-50g per day;
- at fever compresses of grated horseradish and rubbing with vinegar are effective;
- inhalations using pine needles or eucalyptus oil.
 [ 41 ], [ 42 ], [ 43 ], [ 44 ]
[ 41 ], [ 42 ], [ 43 ], [ 44 ]
Herbal treatment
There are many herbs in nature that can help in combination with drug treatment. If the enlargement of the mediastinal lymph nodes is associated with infectious diseases, pneumonia, tuberculosis, sarcoidosis, then you can safely use teas and decoctions with linden, berries or elder flowers, coltsfoot, licorice, plantain, sage, celandine, nettle, calendula. The pharmacy network sells special herbal collections that balance all the necessary components to combat pathological foci.
Homeopathy
Homeopathy is often used when various other methods have been tried and no results have been achieved. Homeopathic treatment for cancer uses biologically active substances discovered at different times by different scientists, aimed at stimulating the body's resistance and activating antitumor mechanisms. If all known treatment methods have been exhausted, but no effect has been achieved, an autonosode is used - a homeopathic autovaccine made using ultra-low doses of toxins and poisons. Such preparations are individual and are made from the patient's blood, urine or saliva based on an alcohol solution.
Homeopathic remedies are also used to treat tuberculosis. Depending on the symptoms, one or another drug is prescribed. Thus, for prolonged sputum, phosphorus is prescribed in different dilutions (in 6, 12, 30); for dyspnea - adonis vernalis, apocynum, digitalis; hemoptysis - millefolium, ferrum aceticum, witch hazel; fever - aconite, belladonna, gelsemium, ferrum phosphoricum; cough - sodium phosphorus, sodium sulphuricum.
Apocynum – made from the root of the red kutra, used in 3, 6, 12, 30 dilutions. Side effects and contraindications are not described.
Millefolium is an anti-inflammatory and venotonic drug in drops. It is recommended to take 10-15 drops three times a day before meals. No side effects have been identified.
Aconite has a combined effect, reduces the secretion of phlegm in the bronchi, reduces temperature, has antiseptic, anti-inflammatory, anesthetic properties. Use half an hour before meals or an hour after. During an exacerbation, put 8 granules under the tongue 5 times a day, gradually reducing to three doses. After 2 weeks, reduce the frequency of administration to 2 times, continue for another two weeks. Allergic reactions are possible, but you should not stop treatment. Contraindicated for pregnant women, hypotensive patients, hypersensitive people.
Hamamelis - for the treatment of lungs is used in granules, the dose is determined by the homeopath individually. For use by pregnant women, a consultation with a gynecologist is necessary.
Surgical treatment
Surgical treatment is used for tumors and cysts of the mediastinum, and it is necessary to do this as early as possible. In the case of malignant tumors, the approach is individual, since at the last stage a radical method does not make sense. Indications for surgical intervention in tuberculosis are the absence of positive dynamics for 1.5-2 years. Sarcoidosis extremely rarely requires surgical intervention, such a need may arise to save a person's life with various complications.
Prevention
The best prevention is a healthy lifestyle, physical exercise, and proper nutrition - all this strengthens the immune system and makes the body less susceptible to various infections. It is also necessary to avoid factors that cause diseases of the mediastinal organs: work or residence in areas of air pollution, contact with patients, hypothermia, stress.
Forecast
The prognosis for the development of pathologies varies for different diseases. Sarcoidosis does not directly pose a threat to life, but its complications can be very dangerous. Timely and complete treatment of tuberculosis has favorable dynamics, and neglect leads to death. Malignant tumors detected at early stages are successfully eliminated by surgery, at later stages - have an unfavorable prognosis.

