Medical expert of the article
New publications
Ehrlichia (ehrlichia)
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The Anaplasmataceae family includes 4 genera - Anaplasma, Ehrlichia, Neorickethsia, Wolbachia. The generic name Ehrlichia (Ehrlichia) was proposed in honor of the German microbiologist Ehrlich.
The closest connections are noted with the genera Rickettsia and Orietiria. Representatives of the Anaplasmataceae family are obligate intracellular proteobacteria that reproduce in specialized vacuoles of eukaryotic cells and have common genetic, biological and ecological characteristics. In human pathology, the most important are Anaplasma, the causative agent of human granulocytic anaplasmosis (HGA), and Ehrlichia chajjfeensis, the causative agent of human monocytic ehrlichiosis (HME), and of lesser importance are Neorickertsia sennetsu and B. ewingii.
Morphology of Ehrlichia and Anaplasma
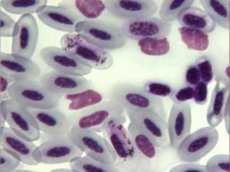
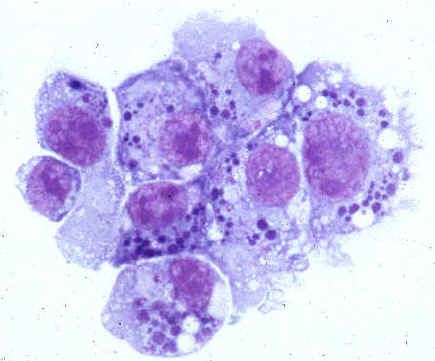
Ehrlichia and anaplasma are gram-negative, small-sized coccobacillary bacteria (length from 0.5 to 1.5 mm-km). Morphologically, they are pleomorphic coccoid or ovoid microorganisms that acquire a dark blue or purple color when stained according to Romanovsky. They are detected in specialized vacuoles - phagosomes in the cytoplasm of infected eukaryotic cells in the form of compact clusters - morulae, so named because of their external resemblance to mulberry berries.
There are two different morphological forms of Ehrlichia (similar to Chlamydia): larger reticular cells, characterizing the stage of vegetative development, and smaller Ehrlichia cells, characterizing the stationary stage of rest.
Microecology of the pathogen, host range and natural habitat
Ehrlichia and apaplasma are obligate intracellular parasites that affect mesodermal cells of mammals, primarily blood cells and vascular endothelial cells. Their reservoirs are various species of warm-blooded animals. The carriers of the pathogens are ixodid ticks, which transmit microorganisms to their hosts when feeding on blood. According to the spectrum of human cells affected, there are pathogens of human monocytic ehrlichiosis (they mainly affect peripheral blood monocytes) and human granulocytic anaplasmosis (they mainly affect granulocytes, mainly neutrophils).
Antigenic structure of Ehrlichia and Anaplasma
Representatives of the Anapfosmataceae family have common antigenic determinants, which determine the greatest cross-reactivity within genogroups.
Physiology of Ehrlichia and Anaplasma
Anaplasma and Ehrlichia are slow-growing microorganisms that reproduce by transverse binary fission, with the presence of vegetative (reticular) and resting (elementary) cells, similar to chlamydia. Representatives of the genera Anaplasma, Ehrlichia, Neorickettsia, and Wolbachia are obligate intracellular proteobacteria that reproduce in specialized vacuoles (phagosomes or endosomes) of eukaryotic cells called morulae. The causative agent of human monocytic ehrlichiosis reproduces in monocytes and macrophages, and the causative agent of human granulocytic anaplasmosis reproduces in granulocytes (neutrophils).
Pathogenicity factors of Ehrlichia and Anaplasma
Representatives of the family have surface proteins that function as adhesins. They interact with lectin-containing associated (for the causative agent of human granulocytic anaplasmosis) receptors of host cells. The presence of factors that prevent phagosomal-lysosomal fusion and provide the possibility of an intraphagosomal development cycle has been proven. Anapfosmataceae has a mechanism for delaying spontaneous apoptosis of neutrophils, which promotes their reproduction in them.
 [ 11 ], [ 12 ], [ 13 ], [ 14 ]
[ 11 ], [ 12 ], [ 13 ], [ 14 ]
Pathogenesis and symptoms of ehrlichiosis and anaplasmosis
The pathogenesis of human granulocytic anaplasmosis and human monocytic ehrlichiosis in the initial stage is caused by the process of pathogen penetration through the skin and is realized with the participation of a tick-carrier. There is no primary effect at the site of penetration. The pathogen spreads lymphogenously and then hematogenously. Infection of sensitive target cells occurs in three stages: penetration into the cell (initiation of phagocytosis), reproduction in membrane-bound cytoplasmic vacuoles (phagosomes), exit from the cell. The infectious process in human monocytic ehrlichiosis is accompanied by damage to the macrophages of the spleen, liver, lymph nodes, bone marrow and other organs. In severe lesions, hemorrhagic syndrome develops with hemorrhages of internal organs, gastrointestinal bleeding, hemorrhagic rashes on the skin.
The pathogenesis and pathological anatomy of human granulocytic anaplasmosis have not been sufficiently studied.
Symptoms of ehrlichiosis and anaplasmosis resemble acute respiratory viral infections. Rash is detected in no more than 10% of patients with human granulocytic anaplasmosis. In patients with human granulocytic anaplasmosis, fever and other clinical manifestations quickly pass with treatment with tetracyclines; without antibiotic therapy, the duration of the disease can be up to 2 months.
Microbiological diagnostics of ehrlichiosis and anaplasmosis
Serological diagnostics of ehrlichiosis and anaplasmosis is currently the most common approach to confirm the diagnosis of human granulocytic anaplasmosis and human monocytic ehrlichiosis. Methods include RNIF, ELISA, immunoblotting based on recombinant proteins (ELISA/immunoblotting). These methods are highly sensitive and quite specific. Seroconversion is the best method of confirmation in the 1st (25% of patients) - 2nd (75%) weeks of the disease.
Microscopically examine thin smears of the peripheral role for the presence of clusters of small bacteria (morula) inside neutrophils. PCR allows identifying the acute phase before using antibiotics. It is also possible to use isolation on HL-60 cell culture.
Prevention and treatment of ehrlichiosis and anaplasmosis
Doxycycline 100 mg 2 times a day for 10-21 days is effective for the treatment of ehrlichiosis and anaplasmosis. As with other tick-borne infections, non-specific preventive measures and anti-tick measures are used for human granulocytic anaplasmosis and human monocytic ehrlichiosis.

