Medical expert of the article
New publications
Chlamydia trachomatis (Chlamydia trachomatis)
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Currently, 14 serovars of the Chlamydia trachomatis biovar are known, which cause more than 20 nosological forms:
- serovars A, B, B1, C cause trachoma and conjunctivitis with intracellular inclusions;
- serovars D, G, H, I, J, K cause urogenital chlamydia, conjunctivitis, pneumonia of newborns, Reiter's syndrome;
- serovars L1, L2, L1a, L2a - cause lymphogranuloma venereum.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
Trachoma
Trachoma is a chronic infectious disease characterized by damage to the conjunctiva and cornea, usually leading to blindness. With trachoma (from the Greek trachys - rough, uneven), the surface of the cornea appears uneven, bumpy as a result of granulomatous inflammation,
The causative agent of trachoma, Chlamydia trachomatis, was discovered in corneal cells in 1907 by S. Prowaczek and L. Halberstelter, who proved the contagiousness of this disease by infecting orangutans with material from conjunctival scrapings of a sick person. The bacterium is found in the cytoplasm of conjunctival epithelial cells in the form of inclusions of the Prowaczek-Halberstelter body.
Epidemiology of trachoma
Trachoma is an anthroponosis transmitted by contact and household means (through hands, clothes, towels). Susceptibility is high, especially in childhood. Foci of the disease are identified. Trachoma is an endemic disease. The disease occurs in countries of Asia, Africa, Central and South America with a low standard of living and sanitary culture of the population.
 [ 10 ], [ 11 ], [ 12 ], [ 13 ]
[ 10 ], [ 11 ], [ 12 ], [ 13 ]
Pathogenesis and symptoms of trachoma
The pathogen in the form of elementary bodies penetrates through the mucous membranes of the eyes and multiplies intracellularly. Follicular keratoconjunctivitis develops, which progresses over many years and ends with the formation of cicatricial connective tissue, which leads to blindness. Often, opportunistic flora is activated, as a result of which the inflammatory process acquires a mixed character.
Immunity is not developed after the disease.
Microbiological diagnostics of trachoma
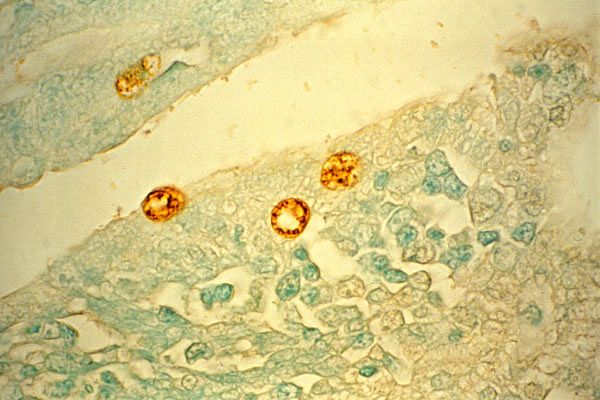
To diagnose trachoma, scrapings from the conjunctiva are examined. The preparations are stained according to Romanovsky-Giemsa, and in this case, cytoplasmic inclusions of violet color with a red center, located near the nucleus - Prowaczek-Halberstelter bodies - are found in the smears.
To detect the antigen, RIF and ELISA are performed.
It is possible to isolate the pathogen in a cell culture in vitro. For this purpose, McCoy, HeLa-229, L-929 and other cell cultures are used.
Treatment of trachoma
Antibiotics of the tetracycline group, interferon inducers and immunomodulators are used.
Prevention
Specific prevention of trachoma has not been developed. It is important to observe personal hygiene measures and improve the sanitary and hygienic culture of the population.
Urogenital chlamydia (non-gonococcal urethritis)
Urogenital chlamydia (non-gonococcal urethritis) is an acute or chronic sexually transmitted disease affecting the genitourinary system, characterized by a slow progression with subsequent development of infertility.
Chlamydia trachomatis, serovar DK, in addition to pathology of the urogenital tract, can cause eye damage (conjunctivitis with inclusions), as well as Reiter's syndrome.
Epidemiology of urogenital chlamydia
Urogenital chlamydia is an anthroponotic infection, the source of infection is a sick person. The route of infection is contact, mainly sexual. Contact-household route is possible (in such cases, familial chlamydia develops), as well as infection by contact with the mucous membrane of the eyes when swimming (pool conjunctivitis).
The disease is very common (up to 40-50% of all inflammatory diseases of the genitourinary system are caused by chlamydia ), but may remain unrecognized (in 70-80% of cases the infection is asymptomatic).
 [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
[ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
Pathogenesis and symptoms of urogenital chlamydia
Chlamydia trachomatis (chlamydia trachomatis) affects the epithelium of the mucous membrane of the urogenital tract. In men, the urethra is primarily infected, in women - the cervix. In this case, slight itching, mucopurulent discharge may be observed. Ascending infection is observed later. As a result of inflammatory processes, male and female infertility develops.
Chlamydia occurs as an infection, in association with gonococci and other pathogenic and opportunistic pathogens. Infection of a pregnant woman is dangerous for both the mother and the fetus: premature birth, postpartum complications, conjunctivitis, meningoencephalitis, sepsis, pneumonia may be observed in newborns. Infection is possible when the child passes through the birth canal of an infected mother.
Along with the damage to individual organs, chlamydia is also characterized by systemic manifestations (Reiter's syndrome). It is characterized by damage to the genitourinary organs (prostatitis), eye disease (conjunctivitis) and joints (arthritis). The disease proceeds with remissions and repeated attacks. The development of the disease is associated with chlamydial antigens, which provoke immunopathological processes in genetically predisposed individuals (70% of those affected have the histocompatibility antigen HLA B27).
Immunity is not formed after an infection. Specific antibodies are found in the blood of infected people, which do not have a protective function.
Microbiological diagnostics of urogenital chlamydia
The material for the study is scrapings from the epithelium of the urethra, cervical canal, conjunctiva. Microscopic examination is possible - preparations are stained according to Romanovsky-Giemsa and Gram. With the help of RIF and ELISA, chlamydia antigens are determined in the studied material. Comprehensive determination of immunoglobulins of classes M, G, A in RNGA,. RIF and ELISA are the most reliable methods and allow determining the stage of development. PCR and DNA hybridization are used. In case of damage to the urogenital tract, cultivation of the pathogen on cell cultures is used.
Treatment of urogenital chlamydia
Antibiotics of the tetracycline series, macrolides, fluoroquinolones are used for a long time (14-21 pep), as well as interferon preparations, interferon inducers and immunomodulators.
Prevention of urogenital chlamydia
Specific prevention of urogenital chlamydia has not been developed. Non-specific measures of prevention of sexually transmitted diseases, timely detection and treatment of patients with urogenital chlamydia are important.
Lymphogranuloma venereum
Lymphogranuloma venereum is a disease characterized by lesions of the genitals and regional lymph nodes and symptoms of generalized infection. The disease is caused by Chlamydia trachomatis (chlamydia trachomatis), serovars L1, L2, L1a, L2a
Epidemiology of lymphogranuloma venereum
The source of infection is a sick person. The path of infection is contact-sexual, much less often contact-household. The infection is endemic in countries with a hot climate - in East Asia, Central and South America, isolated cases are found everywhere. The susceptibility of the population is increased.
 [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
Pathogenesis and symptoms of lymphogranuloma venereum
The entry point for infection is the mucous membranes of the genitals, where chlamydia multiplies. Ulcers appear on the genitals. Then the microbes penetrate into the regional (usually inguinal) lymph nodes. The inflamed lymph nodes open up, forming fistulas with purulent discharge. After several months, destructive changes appear in the surrounding tissues - rectal abscesses.
Immunity
After the disease, persistent immunity develops.
Microbiological diagnostics of lymphogranuloma venereum
The material for the study is pus from buboes, biopsy of the affected lymph nodes. Microscopy of smears-imprints is carried out, the pathogen is isolated in cell cultures and in chicken embryos. The serological method determines antibodies in the microimmunofluorescence reaction. An allergic test establishes the presence of DTH to the pathogen antigens (Frey's intradermal test).
Treatment of lymphogranuloma venereum
Antibiotic therapy with tetracycline and macrolide drugs.
Prevention of lymphogranuloma venereum
Specific prevention of venereal lymphogranuloma has not been developed. Non-specific measures for the prevention of sexually transmitted infections are important.

