Medical expert of the article
New publications
Diagnosis of stages of prostate cancer course
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Clinically, a distinction is made between localized (T 1-2, N 0, M 0 ), locally advanced (T 3-4, N 0-1, M 0 ) and generalized cancer (T 1-4, N 0-1, M 1 ).
Patients with clinically localized and locally advanced stages are classified according to the degree of risk (D'Amico A V. et al., 2003):
- low: stage T 1a-c; PSA level less than 10 ig/ml: Gleason grading - 2-5; in biopsy - unilateral lesion less than 50%:
- moderate: stage T 2a; PSA level less than 10 ng/ml; Gleason score - 3 + 4 = 7; in biopsy - bilateral lesion less than 50%;
- high stage T 2b, T 3a-b; PSA level - 10-20 ng/ml; Gleason grading - more than 4 + 3 - 7; in biopsy - damage more than 50%, perineural invasion;
- very high: stage T 4; PSA level over 20 ng/ml; Gleason score over 8; biopsy shows lymphovascular invasion.
After the diagnosis has been clarified and the extent of the process has been established (localized, locally advanced or generalized), the doctor and the patient are faced with a choice of treatment method. In modern society, great importance is attached to the quality of life of patients after the start of treatment. The quality of life without treatment corresponds to the course of the underlying disease and depends on the progression of the oncological process. Changes in the quality of life occur mainly after the start of treatment and the use of one of the therapeutic or surgical methods. Clearly establishing the stage of the process allows not only to choose the optimal treatment method, but also to predict the further course of the disease.
Determination of the PSA level in combination with the clinical picture of prostate cancer and the gradation of the tumor according to the Gleason scale significantly increases the information content of each of the listed indicators in establishing the pathological stage of cancer. A.V. Partin et al. (1997) proposed prognostic tables that allow predicting the further spread of the tumor, the choice of treatment method, the degree of radicality and the prognosis of the effectiveness of treatment
To assess the spread of the tumor, the most commonly used methods are DRE, TRUS, determination of the PSA level and bone scintigraphy. If necessary, computed tomography (CT) or magnetic resonance imaging (MRI) and chest X-ray are prescribed.
Any of the imaging methods is designed to determine the stage and assess the effectiveness of treatment. After verifying the diagnosis, the urologist must clarify the volume of the primary tumor, its boundaries, invasive or metastatic potential of the tumor. All these indicators are of great importance for the prognosis of the disease and the choice of treatment method.
Primary tumor (T)
First of all, it is necessary to determine whether the tumor is limited to the prostate gland (T 1-2 ) or extends beyond the capsule (T 3-4 ). Digital examination often does not allow to assess the spread of the tumor. According to some data, the results of DRE correspond to those of histological examination in less than 50% of patients. However, a more detailed examination is indicated only when deciding on radical treatment.
The PSA level may reflect the extent of the tumor, but does not allow for an accurate determination of the morphological stage. The combination of the PSA level, Gleason index, and palpation data allows for a better prediction of the morphological stage than each of these parameters separately. The value of free PSA is controversial: in one study, determining the free PSA content helped to clarify the stage in localized tumors, but other studies did not confirm this. Only in-depth studies will help resolve this issue.
Transrectal ultrasound is most often used to examine the condition of the prostate gland. This method can detect only 60% of tumors and does not always show capsule invasion. Almost 60% of patients with stage T3 . Ultrasound indicates a less common process. Ultrasound signs of capsule invasion are bulge, unevenness and rupture of the gland contour. Invasion of tumor cells into the seminal vesicles is a poor prognostic sign, but information about it is extremely important for choosing a treatment method. When performing TRUS, attention should be paid to the echostructure of the vesicles (hyperechogenicity), their asymmetry, deformation and expansion. Also, damage to the seminal vesicles is indicated by loss of roundness and compaction at the base of the gland. These signs are quite subjective, so it is inappropriate to rely entirely on ultrasound data. Invasion of the seminal vesicles indicates a high risk of local relapse and metastases, and their biopsy is indicated for clarification (before surgery). The examination should not be started with this procedure, but if the risk of invasion is high and the choice of treatment depends on the biopsy result, then its implementation is justified. A negative result does not exclude microscopic invasion. As a rule, a biopsy of the seminal vesicles is carried out at the clinical stage T 2b and higher and the PSA content is more than 10 ng/ml. The result is considered positive if at least one biopsy from the base of the prostate gland contains tumor cells. Not only additional studies, but also a thorough analysis of the results of the primary biopsy allow to increase the accuracy of clinical determination of the stage (the number and extent of tumor foci, capsule invasion play a role). The degree of differentiation is also important: with a Gleason index of less than 6, the tumor is localized in 70% of cases.
Blood flow in the prostate gland with cancer is higher than in a normal gland or with its hyperplasia. After castration, the intensity of blood flow in the gland is reduced. The development of echo-Dopplerographic maps for the diagnosis and monitoring of prostate cancer is promising, but at present there is no reliable data on the use of echo-Dopplerography in determining the stage of the local process. It is possible to use this method to obtain additional material during targeted biopsy from foci of pathological vascularization.
The results of prostate cancer visualization directly depend on the technical equipment of the clinic and the experience of the specialist. That is why all modern visualization methods play not a determining but a clarifying role, and the choice of treatment method is based on a combination of clinical examination data and instrumental studies.
MRI has the best capabilities for visualizing the structure of the prostate gland. The modern standard for examining the pelvic organs using the MRI method is the use of an endorectal sensor, which allows obtaining an image with the highest possible spatial resolution of 0.5-1 mm. Forcing air into the endorectal sensor provides clear visualization of the prostate capsule, rectoprostatic angles and Denonvilliers' rectoprostatic fascia. The use of an endorectal sensor in MRI does not limit the visualization of regional lymph nodes (up to the level of the bifurcation of the abdominal aorta). Prostate cancer is characterized by low signal intensity on T-weighted images against the background of a high-intensity signal from an unchanged peripheral zone of the gland. Irregular shape, diffuse spread with mass effect, fuzzy and uneven contours are morphological characteristics of foci of low signal intensity in the peripheral zone of the prostate gland, suggesting a neoplastic nature of the lesion. When performing dynamic contrasting, cancer foci quickly accumulate the contrast agent in the arterial phase and quickly remove the agent, which reflects the degree of angiogenesis and, accordingly, the degree of tumor malignancy. Low signal intensity is also characteristic of foci of post-biopsy hemorrhages, prostatitis, stromal benign hyperplasia of the neutral zone of the gland, fibrous-cicatricial changes, fibromuscular hyperplasia, consequences of hormonal or radiation therapy. MRI without dynamic contrasting does not allow reliable differentiation of most of the listed changes and diseases.
As noted above, one of the main tasks of any imaging method for prostate cancer is to determine the volume of the gland lesion and the spread of the tumor beyond the capsule. Determining the tumor volume is important for prognosis. A tumor volume of less than 4 cm 3 indicates distant metastases, and 12 cm 3 indicates an extremely high probability of metastases. According to research, the accuracy of MRI in detecting foci of neoplastic lesions of the prostate gland ranges from 50 to 90%. The sensitivity of MRI in determining the localization of prostate cancer is about 70-80%, while microscopic foci of cancer (foci) cannot be detected using MRI.
The most important advantage of endorectal MRI is the ability to localize neoplastic lesions in areas inaccessible to other diagnostic methods and to clarify the nature and direction of tumor growth. For example, MRI allows detecting neoplastic lesions in the anterior parts of the peripheral zone of the prostate gland, inaccessible with transrectal biopsy. In general, MRI significantly complements the data of DRE and TRUS on tumor localization.
Endorectal MRI allows visualization of the gland capsule, vascular-nerve bundles, seminal vesicles, gland apex, periprostatic venous plexus and determination of local prevalence of gland tumor. It should be emphasized that capsule penetration is considered a microscopic sign, and even modern MRI devices (endorectal coil) are not able to provide such information. It is only possible to obtain data on growth beyond the gland capsule.
Diagnostic criteria for extracapsular extension using MRI:
- the presence of an extracapsular tumor;
- uneven contour of the gland (deformation, angularity);
- asymmetry of neurovascular bundles;
- obliteration of the rectoprostatic angles;
- wide contact of the tumor with the capsule.
The highest specificity (up to 95-98%) and accuracy of MRI results are achieved when examining patients with medium or high risk of extracapsular invasion. It is believed that extracapsular invasion (according to MRI data) indicates the inappropriateness of surgical treatment and an unfavorable prognosis for the disease. Hormonal or radiation therapy does not affect the accuracy of detecting extracapsular spread of prostate tumor. The main difficulty in detecting foci of cancer and extracapsular spread of tumor is the high variability of tomogram interpretation by different specialists. The primary task of a specialist in radiation diagnostics is to achieve high diagnostic specificity (even at the expense of sensitivity) in order not to deprive operable patients of the chance for radical treatment.
The similarity of the density of cancerous, hyperplastic and normal prostate tissue in CT makes this method of little use for assessing the local spread of the tumor. Invasion into the seminal vesicles is more important than invasion into the capsules, but even in this case CT provides information only in advanced cases. However, this method is actively used to mark the area of impact before radiation therapy.
The slow development of radiation diagnostics in our country has led to late diagnosis of prostate cancer and, consequently, to insufficient prevalence of radical methods of prostate cancer treatment (for example, prostatectomy), low availability of modern tomographs and the absence of appropriate training programs for specialists in radiation diagnostics and urologists. Despite the fact that CT and MRI are now widespread, the level of equipment of offices and education of specialists in radiation diagnostics is insufficient for the information obtained to become decisive in choosing a method of treatment for patients with prostate cancer.
Regional lymph nodes (N)
Regional lymph nodes should be assessed only when this directly affects the treatment strategy (usually when planning radical treatment). High PSA levels, T2c -T3a tumors, poor differentiation, and perineural invasion are associated with a high risk of lymph node metastasis. Assessment of lymph node status based on PSA levels is considered insufficient.
Only lymphadenectomy (open or laparoscopic) provides the necessary information. Recent studies of extended lymphadenectomy have shown that prostate cancer does not always affect the obturator lymph nodes. In asymptomatic tumors and PSA levels less than 20 kg/ml. CT confirms enlarged lymph nodes only in 1% of cases. The use of MRI or CT is justified in cases of high risk of metastasis, since the specificity of these methods reaches 93-96%. However, even a positive result when using them can be false, and only a puncture of a suspicious lymph node allows one to refuse lymphadenectomy. According to retrospective analysis, the size of the lymph node does not always indicate the presence of metastases in it; asymmetry of the affected lymph nodes is considered a more informative sign. Currently, only 2-3% of patients who have undergone radical prostatectomy for localized prostate cancer are diagnosed with metastasis to the lymph nodes based on postoperative histological examination.
Positron emission tomography (PET) and scintigraphy with labeled antibodies are recommended as methods for detecting metastasis to lymph nodes, but their use is still limited due to insufficient sensitivity.
Partin's nomograms (2001) can be used to assess the risk of regional lymph node involvement. Nomograms are mathematical algorithms that are used for a specific patient or a group of patients. These tables allow one to determine the probability of local tumor spread (to the capsule, seminal vesicles) and lymph node involvement based on the clinical stage, PSA level, and Gleason index. In particular, they make it possible to identify a group of patients with a low (less than 10%) probability of lymph node metastasis (with a PSA level over 20 ng/md, stage T 1-2a, and Gleason index 2-6); in this group, the condition of the lymph nodes may not be specified before radical treatment. The risk of lymph node metastasis can also be assessed by detecting tumor areas with pronounced anaplasia (4-5 points): if such areas are found in four or more biopsies or they predominate in at least one biopsy, the risk reaches 20-45%. In other patients it does not exceed 2.5%. Additional examination is not required in such cases.
Distant metastases (M)
In 85% of patients dying from prostate cancer, lesions of the axial skeleton are detected. Bone metastases occur due to the penetration of cancer cells into the bone marrow with the bloodstream, which leads to tumor growth and lysis of bone structures. The prevalence of bone metastases affects the prognosis, and their early detection warns the doctor about possible complications. In 70% of cases, metastasis is combined with an increase in the activity of the bone isoenzyme of alkaline phosphatase (ALP). Determination of the activity of ALP and the PSA level in the vast majority of cases allows us to detect bone metastasis. According to multivariate analysis, these indicators are affected only by the number of bone metastases. It is important that the activity of the bone isoenzyme ALP reflects the degree of bone damage more accurately than the PSA level.
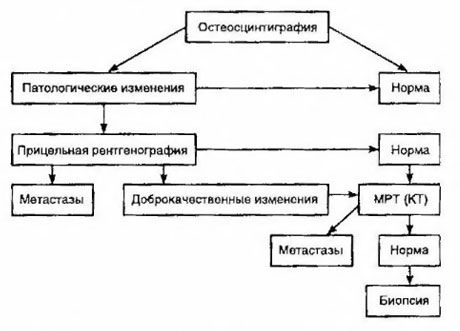
Scintigraphy is considered the most sensitive method for detecting bone metastases (it is superior to radiography and determination of alkaline and acid phosphatase activity). Technetium diphosphonates are better used as a radiopharmaceutical drug, since their accumulation in bones is much more active than in soft tissues. A correlation has been shown between a semi-quantitative assessment of bone damage and survival. Detection of distant metastases is possible in any organ. They most often occur in non-regional lymph nodes, lungs, liver, brain and skin. In case of corresponding complaints and symptoms, chest radiography, ultrasound, CT and MRI are used to detect them. The tactics for suspected bone metastasis are presented in the diagram.
The most reliable laboratory indicator that helps to determine the degree of metastasis is the PSA level. It has been shown that its increase over 100 ng/ml is the only parameter that reliably indicates distant metastases. Determining the PSA level reduces the number of patients who need bone scintigraphy. The probability of detecting bone metastases with a decrease in the PSA level is very low. In the absence of complaints and the initial PSA content of less than 20 ng/ml, detection of highly and moderately differentiated tumors, scintigraphy can be avoided. At the same time, in the case of poorly differentiated tumors and capsule invasion, scintigraphy is indicated (regardless of the PSA level).


 [
[