Medical expert of the article
New publications
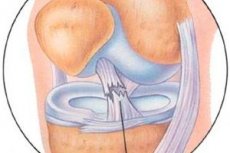
Anterior cruciate ligament injuries
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
For several decades, work has been carried out to study the results of arthroscopic treatment of injuries to the capsular-ligamentous apparatus of the knee joint.
Despite the variety of arthroscopic methods for treating anterior post-traumatic instability of the knee joint, there is still a significant percentage of unsatisfactory results, the most important reasons for which are complications resulting from errors at the stages of diagnosis, surgical treatment and rehabilitation of patients with anterior post-traumatic instability.
The literature covers quite extensively possible complications after arthroscopic treatment of anterior posttraumatic instability. However, little attention has been paid to the analysis of their causes and methods of their correction.
Epidemiology
The problem of treating patients with knee joint pathology remains important and one of the most difficult in traumatology to this day. The knee joint is the most frequently injured joint, accounting for up to 50% of all joint injuries and up to 24% of lower limb injuries.
According to various authors, ruptures of the cruciate ligaments of the knee joint occur with a frequency of 7.3 to 62% among all injuries of the capsular-ligamentous apparatus of the knee joint.
Diagnostics anterior cruciate ligament injuries
All patients undergo a clinical and radiological examination before the primary operation. Anamnesis, examination, palpation, clinical testing of knee joint structure damage, radiography, general blood and urine analysis, biochemical blood and urine tests are performed. According to indications, the following instrumental studies are performed: testing on the CT-1000 device, CT, MRI, ultrasound. Diagnostic arthroscopy immediately precedes surgical treatment.
The patient examination begins with finding out the complaints and collecting the anamnesis. It is important to determine the mechanism of damage to the ligamentous apparatus of the knee joint and collect information about previous operations on the knee joint. Next, they conduct an examination, palpation, measure the circumference of the joint, determine the amplitude of passive and active movements, and also widely use the Lysholm questionnaire testing tables for athletes and the 100-point scale developed at the Central Institute of Traumatology and Orthopedics for patients with less physical demands.
The functions of the lower extremities are assessed based on the following parameters: complaints of instability in the joint, the ability to actively eliminate the passively imposed pathological displacement of the tibia, support ability, lameness, performance of special motor tasks, maximum strength of the periarticular muscles during prolonged work, hypotrophy of the thigh muscles, muscle tone, complaints of pain in the joint, the presence of synovitis, compliance of motor capabilities with the level of functional aspirations.
Each sign is assessed on a 5-point scale: 5 points - no pathological changes, compensation of functions; 4-3 points - moderate changes, subcompensation; 2-0 points - pronounced changes, decompensation.
The assessment of treatment results includes three degrees: good (more than 77 points), satisfactory (67-76 points) and unsatisfactory (less than 66 points).
One of the criteria for subjective evaluation of treatment results is the patient's own assessment of his/her functional state. The condition for a good result is the restoration of functional performance. Without this, the treatment results are considered satisfactory or unsatisfactory.
During the clinical examination, range of motion is assessed and stability tests are performed. It is always important to rule out the anterior drawer sign.
Patients complain of pain and/or a feeling of instability in the joint. The pain may be caused by the instability itself or by associated cartilage or meniscus damage. Some patients cannot recall the previous injury, suddenly becoming aware of the knee joint months or years later. Patients rarely describe the knee joint as unstable. They usually describe uncertainty, looseness, and inability to control movement in the injured joint.
Crepitus under the patella is characteristic due to a violation of biomechanics in the patellofemoral joint.
Often secondary symptoms become dominant: chronic joint effusion, degenerative changes in the joint or Baker's cyst.
The condition of the active-dynamic stabilizing structures both before and after the operation is also considered important. This is due to the achievement of a sufficiently reliable stabilizing effect due to the periarticular muscles.
Great importance is attached to the indicator of muscle strength.
To diagnose anterior instability and evaluate the long-term results of its treatment, the most informative tests are used: the anterior “drawer” symptom in the neutral position of the tibia, the abduction test, the adduction test, and the Lachman test.
An important indicator of the functional state is the ability to actively eliminate the passively imposed pathological displacement of the tibia relative to the thigh.
From special motor tasks we use walking, running, jumping, climbing stairs, squats, etc.
It is imperative to take into account the endurance of the periarticular muscles during long-term work.
The passive testing complex includes the anterior “drawer” symptom in three positions of the tibia, abduction and adduction tests at 0 and 20° of flexion in the joint, a recurvation test and a lateral change of support point test, the Lachman-Trillat test, and measurement of pathological rotation of the tibia.
The active testing complex includes an active anterior “drawer” test in three positions of the lower leg, active abduction and adduction tests at 0 and 20° flexion in the joint, and an active Lachman test.
To determine damage or insufficiency of the anterior cruciate ligament, the anterior "drawer" symptom is used - passive displacement of the tibia (anterior translation), also with different flexion positions of the tibia. It is recommended to focus on one of the most accepted, according to literature, gradations of this symptom: I degree (+) - 6-10 mm, II degree (++) -11-15 mm, III degree (+++) - more than 15 mm.
In addition, the anterior drawer symptom should be assessed with different rotational positions of the tibia - 30°, external or internal rotation.
The Lachman sign is recognized as the most pathognomonic test for detecting damage to the anterior cruciate ligament or its graft. It is believed that it provides the most information about the state of the anterior cruciate ligament in acute KC injury, since when it is performed, there is almost no muscular resistance to the anteroposterior translation (displacement) of the tibia, as well as in chronic KC instability.
The Lachman test is performed in the supine position. The Lachman test is assessed based on the magnitude of the anterior displacement of the tibia relative to the femur. Some authors use the following gradations: Grade I (+) - 5 mm (3-6 mm), Grade II (++) - 8 mm (5-9 mm), Grade III (+++) - 13 mm (9-16 mm), Grade IV (++++) - 18 mm (up to 20 mm). In an effort to unify the assessment system, we use a three-stage gradation similar to that previously described for the anterior "drawer" symptom.
The symptom of a change in the rotation point, or the symptom of anterior dynamic subluxation of the tibia (pivot shift-test), is also considered a symptom pathognomonic for damage to the anterior cruciate ligament; to a lesser extent, it is characteristic of a combination with a rupture of the internal lateral ligamentous structures.
The test is performed in the supine position, the leg muscles should be relaxed. One hand grasps the foot and turns the shin inward, the other is located in the area of the lateral femoral condyle. With slow flexion of the knee joint to 140-150°, the hand feels the occurrence of anterior subluxation of the tibia, which is eliminated with further flexion.
The pivot shift test on Macintosh is performed in a similar position of the patient. Internal rotation of the tibia is performed with one hand, and valgus deviation with the other. With a positive test, the lateral part of the articular surface of the tibia (the outer plateau) is displaced forward, with slow flexion of the knee to 30-40°, it is displaced backward. Although the pivot shift test is considered pathognomonic for anterior cruciate ligament deficiency, it may be negative in case of damage to the iliotibial tract (ITT), complete longitudinal rupture of the medial or lateral meniscus with dislocation of its body (a "watering can handle" rupture), a pronounced degenerative process in the lateral part of the joint, hypertrophy of the tubercles of the intercondylar eminence of the tibia, etc.
The active Lachmann test can be used both during clinical examination and during radiographic examination. In case of damage to the anterior cruciate ligament, the anterior displacement of the tibia reaches 3-6 mm. Testing is performed in the supine position with the legs fully extended. One hand is placed under the thigh of the examined limb, bending it at the knee joint at an angle of 20°, and the KJ of the other leg is grasped with the hand so that the thigh of the examined limb lies on the examiner's forearm. The other hand is placed on the anterior surface of the patient's ankle joint, his heel is pressed to the table. Then the patient is asked to tense the quadriceps muscle of the thigh and carefully monitor the movement of the tibial tuberosity forward. If it is displaced by more than 3 mm, the symptom is considered positive, which indicates damage to the anterior cruciate ligament. To determine the condition of the medial and lateral stabilizers of the joint, a similar test can be performed with internal and external rotation of the tibia.
X-ray
Radiography is performed using the generally accepted method in two standard projections; functional radiographs are also performed.
When evaluating the images, the position of the patella, the tibiofemoral angle, the convexity of the lateral tibial plateau, the concavity of the medial plateau, and the dorsal position of the fibula in relation to the tibia are taken into account.
X-rays allow us to assess the overall condition of the knee joint, identify degenerative changes, determine the condition of the bones, the type and position of metal structures, the location of the tunnels and their expansion after surgical treatment.
The doctor's experience is of great importance, since the evaluation of the obtained images is quite subjective.
Lateral radiographs should be taken at 45° flexion in the joint to properly assess the relationship of the tibia to the patella. To objectively assess the rotation of the tibia, it is necessary to superimpose the lateral and medial condyles of the tibia on each other. The height of the patella is also assessed.
Insufficient extension is easier to diagnose in the lateral projection, with the patient lying with the leg pronated.
To determine the limb axis, additional X-rays in direct projection on long cassettes with the patient standing are required, since there are deviations from the norm in deforming arthrosis. The anatomical axis of the limb, determined by the longitudinal orientation of the thigh to that of the shin, is on average 50-80°. This is the most important point in the course of further surgical treatment (corrective osteotomy, arthroplasty, endoprosthetics).
The degree of displacement of the tibia relative to the femur in the anteroposterior and medial-lateral directions is determined using functional radiographs with load.
In chronic anterior instability of the knee joint, characteristic radiographic signs are noted: narrowing of the intercondylar fossa, narrowing of the joint space, the presence of peripheral osteophytes on the tibia, upper and lower poles of the patella, deepening of the anterior meniscal groove on the lateral condyle of the femur, hypertrophy and pointedness of the tubercle of the intercondylar eminence.
The lateral radiograph very often indicates the cause of the limitation of motion. The lateral radiograph at maximum extension may indicate insufficient extension, while evaluating the position of the tibial tunnel relative to the intercondylar arch, which appears as a linear thickening (Blumensaat's line).
 [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
Computer tomography
CT is not considered a routine examination. CT is performed on patients when other types of examination are insufficiently informative, especially in the case of compression fractures of the tibial condyles.
CT is good for visualizing bone and osteochondral damage. CT allows for various dynamic tests with knee flexion at various angles.
 [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ]
[ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ]
KT-1000
To measure the anteroposterior displacement of the tibia, the KT-1000 device is used.
The KT-1000 device is an arthrometer, it consists of the actual device for measuring the anteroposterior displacement of the tibia relative to the femur and supports for the lower thirds of the thighs and feet. The device is attached to the shin using Velcro straps, and the existing sensor platform presses the patella to the anterior surface of the femur. In this case, the joint space should coincide with the line on the device. The lower limb located on the supports is bent at the knee joint within 15-30° to measure the anterior displacement of the shin and 70° to measure the posterior displacement of the shin relative to the femur.
First, the injured knee joint is tested. To measure the anterior displacement of the tibia, the doctor pulls the handle located in the anterior-upper part of the device towards himself and tries to make an anterior displacement of the tibia by holding the sensory pad on the patella. In this case, a force of 6, 8 and 12 kg is applied, which is controlled by sound signals. With each sound signal, the doctor notes the deviation of the arrow on the scale and records the device readings. The displacement of the tibia relative to the femur is expressed in millimeters. Next, the doctor tests the posterior displacement of the tibia by bending it at the knee joint to an angle of 70° and tries to displace the tibia backwards using the device handle. The sound signal that occurs when the arrow is deflected indicates the magnitude of the posterior displacement of the tibia relative to the femur.
Similar testing is performed on the healthy knee joint. The corresponding data obtained from the healthy and damaged knee joints are then compared and subtracted. This difference shows the amount of anterior displacement of the tibia relative to the femur under a load of 6, 8 and 12 kg.
Anterior displacement is determined at a 30° flexion angle of the tibia.
If a difference in the magnitude of the anterior displacement at 67H and 89H of the affected and healthy joints of more than 2 mm is detected, a rupture of the anterior cruciate ligament is suspected.
There are certain principles of instrumental testing for instability of the knee joint. The following parameters must be taken into account: the degree of rigidity of fixation of the limb with belts, the location of the sensory sensors on the joint, complete relaxation of the leg muscles, the location of the arthrometer in relation to the joint space, the degree of rotation of the lower leg, the weight of the leg, the angle of flexion in the knee joint.
In the acute period after injury, the use of an arthrometer is inappropriate, since it is impossible to completely relax the periarticular muscles. It is necessary to choose the neutral position of the shin correctly, taking into account that with anterior displacement of the shin, internal rotation occurs, with posterior - external. Otherwise, the value of the anteroposterior translation will be less than the true value. In order to obtain the maximum value of pathological displacement of the shin, it is also necessary to allow its free rotation.
The degree of translation depends on the magnitude of the applied force, its point of attraction and direction.
The use of footrests should not limit the rotation of the lower leg. It is necessary to position the sensors strictly oriented towards the joint space, since if they are displaced distally, the readings will be less than the true value, if proximally - more.
A mandatory condition for an objective assessment is fixation of the patella in the intercondylar groove. To do this, it is necessary to give the tibia an angle of flexion in the joint of about 25-30°. In case of congenital and post-traumatic subluxations of the patella, the angle of flexion is increased to 40°. In case of anterior instability, the angle of flexion in the joint is 30°, in case of posterior instability - 90°.
Two audio signals accompany the test: the first at a load of 67N, the second at 89N. Sometimes, more force is required to determine a rupture of the anterior cruciate ligament.
Normally, the difference between the two limbs when testing the anteroposterior displacement does not exceed 2 mm; sometimes a value of less than 3 mm is indicated as the normal limit.
The index of anterior compliance is taken into account, i.e. the difference between the displacement at 67N and 89N. This value should also not normally exceed 2 mm.
If the displacement is more than 2 mm, we can talk about a rupture of the anterior cruciate ligament (anterior cruciate ligament graft).
It should also be noted that in case of instability of both knee joints or hypermobility, the use of the KT-1000 arthrometer is not advisable.
In conclusion, it should be said that when using this arthrometer, there is certainly an element of subjectivity, depending on a number of parameters, including the researcher. Therefore, the examination of patients should be carried out (if possible) by one doctor.
With the help of CT-1000 it is possible to only ascertain the anteroposterior displacement of the tibia relative to the femur, while lateral instability is not recorded.
Magnetic resonance imaging
MRI is the most informative of the non-invasive research methods, allowing visualization of both bone and soft tissue structures of the knee joint.
A healthy anterior cruciate ligament should appear low intensity on all images. Compared to the denser posterior cruciate ligament, the anterior cruciate ligament may be slightly inhomogeneous. Because of its oblique orientation, many prefer to use oblique coronal images. If the anterior cruciate ligament is torn, MRI can visualize the site of injury.
The anterior cruciate ligament is well visualized on lateral sections during extension and external rotation of the tibia. The anterior cruciate ligament is brighter than the posterior cruciate ligament, the fibers of the anterior cruciate ligament are twisted. The absence of continuity of the fibers or their chaotic orientation indicates a rupture of the ligament.
A complete rupture of the anterior cruciate ligament is diagnosed more by indirect signs: anterior displacement of the tibia, excessive posterior tilt of the posterior cruciate ligament, wavy contour of the anterior cruciate ligament.
Ultrasound examination
The advantages of ultrasound are low cost, safety, speed, and highly informative images of soft tissues.
Ultrasound allows to study the condition of the soft tissues of the knee joint, the surface of the bone and cartilage by the echogenicity of the structure, and also to determine tissue edema, fluid accumulation in the joint cavity or periarticular formations by a decrease in echogenicity. Ultrasound is used to detect damage to the meniscus of the knee joint, collateral ligaments, soft tissue structures surrounding the knee joint.
Arthroscopy
In diagnostic arthroscopy, the authors use standard approaches: anterolateral, anteromedial, and superior patellar lateral.
Arthroscopic examination of the anterior cruciate ligament includes assessment of the appearance of the anterior cruciate ligament, integrity of the ligament's own synovial membrane, orientation of collagen fibers not only at the tibial attachment site of the ligament, but also along its length, especially at the site of the femoral insertion. If in cases of damage to the anterior cruciate ligament along its length and at the tibial attachment site with a ruptured bone fragment, arthroscopic diagnostics does not present any particular difficulty, then diagnostics of intrasynovial (intrastruncal) fresh and old injuries of the anterior cruciate ligament presents great difficulties. This is due to the fact that externally, at first glance, the anterior cruciate ligament seems to be intact: the synovial membrane is intact, palpation of the anterior cruciate ligament with an arthroscopic hook shows the presence of a full-fledged structure and thickness of the ligament, the arthroscopic symptom of the anterior "drawer" shows sufficient tension of the ligament fibers. However, a more careful examination of the capillary network in the middle and femoral parts of the ligament, as well as opening the synovial membrane of the ligament, makes it possible to determine damage to the ligament fibers and the presence of hemorrhages or scar tissue. A secondary sign of an old intrasynovial injury to the anterior cruciate ligament is hypertrophy of the synovial and fatty tissue on the femoral part of the posterior cruciate ligament and the vault of the intercondylar notch of the femur (the "tissue growth" symptom).
Sometimes only arthroscopically it is possible to record the following types of damage to the anterior cruciate ligament:
- injury to the anterior cruciate ligament at the femoral attachment site with or without formation of a stump;
- intrasynovial injury of the anterior cruciate ligament;
- anterior cruciate ligament injury;
- in rare cases - damage to the anterior cruciate ligament in the area of the intercondylar eminence with a break in a bone fragment.
Treatment anterior cruciate ligament injuries
In the compensated form of anterior instability of the knee joint, treatment consists of immobilization followed by restoration of joint mobility and the functions of active stabilizers (muscles).
In subcompensated and decompensated forms of anterior instability, there is a need for surgical intervention aimed at restoring the integrity of primarily static stabilizers. The treatment complex necessarily includes functional treatment to strengthen active stabilizers.
It should also be noted that as a result of treatment measures, mainly in the case of anteromedial instability, transitions from subcompensated to compensated form are possible, since this anatomical region has the largest number of secondary stabilizers, which has a beneficial effect on the treatment outcome.
Management of patients with anterior instability of the knee joint depends on many factors: age, type of professional activity, level of sports training, concomitant intra-articular injuries, degree of instability, risk of re-injury, time since injury. First of all, plastic reconstruction of the anterior cruciate ligament in case of rupture is indicated for professional athletes, especially with concomitant injuries to other structures of the knee joint. Reconstruction of the anterior cruciate ligament is also recommended for chronic instability of the knee joint.
Indications for anterior arthroscopic static stabilization are primary and recurrent subcompensated and decompensated forms and types of anteromedial (A2M1, A2M2, AZM1, AZM2, AZM3) and anterolateral (A2L1, A2L2, A2L3, AZL1, AZL2, AZL3) instability, and the inability to compensate for the pathology with conservative treatment methods.
The decision on plastic reconstruction of the anterior cruciate ligament in patients over 50 years old is made depending on the age and level of physical activity of the patient, the degree of deforming arthrosis. Plastic surgery of the anterior cruciate ligament is recommended in case of severe limitation of physical activity due to instability of the knee joint.
In each individual case, the decision on surgical treatment is made taking into account the individual characteristics of the patient.
The following conditions and diseases are considered contraindications to static stabilization:
- presence of grade III-IV gonarthrosis;
- severe hypotrophy of the thigh muscles;
- joint contracture;
- the period after injury is more than 3 days and less than 3 weeks;
- infectious diseases;
- osteoporosis;
- thrombosis of the vessels of the lower limb.
At the stage of determining the indications and contraindications for surgical treatment of anterior post-traumatic instability, a dilemma sometimes arises. On the one hand, the consequences of chronic instability (hypotrophy of the thigh muscles, deforming arthrosis) become contraindications to performing static stabilization, and arthroscopic stabilization using transplants with bone blocks leads to an increase in the load on the articular cartilage (as a consequence - to the progression of deforming arthrosis). On the other hand, conservative methods do not provide a sufficient stabilizing effect, which also contributes to the development of deforming arthrosis.
Sometimes it is recommended to postpone the operation until the range of motion in the knee joint increases, which can take 2-3 weeks. Postponing the operation in the acute phase leads to a reduction in complications during rehabilitation measures associated with the restoration of range of motion in the knee joint after surgical treatment.
Selection of autograft and fixation method
The most commonly used autografts for reconstruction of the anterior cruciate ligament are patellar tendon, semimembranosus and grace tendon, and in rare cases Achilles and quadriceps tendon. The central third of the patellar tendon with two bone blocks remains the most common autograft for reconstruction of the anterior cruciate ligament in athletes. The quadriceps tendon with one bone block or without a bone block is increasingly used as an autograft for replacing the anterior cruciate ligament. The most commonly used automaterial for anterior cruciate ligament transplantation at CITO is the central third of the patellar tendon. This graft has two bone blocks (from the patella and tibial tuberosity) to ensure primary reliable rigid fixation, which facilitates early loading.
The advantages of patellar tendon autograft are as follows.
- Normally, the width of the patellar ligament allows for the collection of an autograft of any required width and thickness. Typically, the graft is 8-10 mm wide, but sometimes, in cases of repeated reconstruction, the required width can reach 12 mm.
- The patellar ligament is always available as automaterial and has minor anatomical variations. This allows for technically simple automaterial collection at any time.
- Bone blocks allow the graft to be firmly fixed, for example by means of interference screws, screwed between the bone block and the wall of the bone tunnel. This method provides very high primary fixation.
The use of an autograft from the tendons of the semitendinosus and grace muscles, according to some authors, increases the pathological external rotation of the tibia to 12%. The success of the reconstruction of the anterior cruciate ligament significantly depends on the biological remodeling of the transplant.
Due to the removal of a strip of ligament with bone blocks from the patella and tibial tuberosity, this area becomes painful. Although the bone defect can be closed with spongy bone, it is not always possible to adequately close the defect with soft tissues, especially if the primary injury has caused scar formation around the tendon.
Since the bone block is taken from the tibial tuberosity, which is important for knee support, some patients (wrestlers, artists, clergy, etc.) may complain of pain during direct load on the knee joint or inability to support the knee. There are observations when the patient does not complain of instability of the knee joint and insufficient limb function after surgery, but due to this complication is forced to quit or limit their usual professional activity. Therefore, a good result is based not only on stability.
In the sports and ballet trauma clinic of the Central Institute of Traumatology and Orthopedics, preference is given to the use of autografts from the patellar ligament with two bone blocks and their fixation with interference screws.
Anterior static stabilization of the knee joint with a free autograft from the patellar ligament is performed following diagnostic arthroscopy to determine the scope and types of intervention.
The autograft is usually taken from the ipsilateral limb to preserve the contralateral limb as a support. First, a bone block is taken from the tibial tuberosity, then from the patella. One of the bone blocks must be large enough to be fixed in the femoral tunnel.
To reduce the likelihood of bone block splitting and the amount of damage to the donor site, trapezoid-shaped autograft bone fragments are harvested; such a bone block is easier to process with crimping pliers, which gives the graft a rounded shape, while reducing the risk of patellar fracture.
Such an autograft is easier to install in intraosseous tunnels. The autograft is first cut off from the tibial tuberosity, then from the patella.
Using arthroscopic compression, bone blocks are given a rounded shape.
Simultaneously with the preparation of the autograft, the optimal (isometric) position of the tibial tunnel is determined. For this purpose, a special stereoscopic system is used (the angle of the stereoscopic system is 5.5°). The tunnel is centered, focusing on the remaining tibial part of the anterior cruciate ligament, and if it is absent, on the area between the tubercles of the intercondylar eminence or 1-2 mm behind them.
Its diameter varies depending on the size of the autotransplant (it should be 1 mm larger than the diameter of the transplant). A drill of a given diameter is used to form an intraosseous tunnel (strictly along the spoke, otherwise the canal will widen). The joint is washed thoroughly to remove bone chips. An arthroscopic rasp is used to smooth the edge of the tibial canal exit.
At the next stage, a drill is used to determine the femoral insertion point on the lateral femoral condyle (5-7 mm from the posterior edge) for the right knee joint at 11 o'clock. In revision reconstructions, the "old" canal is usually used with minor variations in its position. Using a cannulated drill, the femoral canal is drilled; its depth should not exceed 3 cm. Having finished drilling the canal, the edges of the femoral canal are processed using an arthroscopic rasp.
In some cases, plastic surgery of the intercondylar notch is performed (Gothic arch, ramp of the intercondylar notch).
Before inserting the autograft into the bone tunnels, all bone-cartilaginous fragments are removed from the joint cavity using an arthroscopic clamp and thorough rinsing of the joint.
The sutured graft is inserted into the intraosseous tunnels and fixed in the femoral tunnel with an interference screw.
After fixation of the femoral end of the transplant, the joint is washed with antiseptics to prevent purulent complications.
Then the operated lower limb is fully extended and fixed in the tibial canal, necessarily with full extension of the knee joint. The threads are pulled along the axis of the canal, the arthroscope is inserted into the lower tibial portal, the point and direction of fixation with a screw are determined using a knitting needle (if the bone tissue in this area is hard, a sword is inserted). When screwing in the screw, the displacement of the bone block is monitored according to the position and tension of the threads so that it is not pushed out of the canal into the joint cavity. At the next stage, using an arthroscope, it is visualized whether the bone block protrudes into the joint due to its displacement along the axis of the canal when tightening the screw (therefore, it is better to use a self-tightening screw), then using an arthroscope, the degree of adhesion of the bone block to the wall of the bone tunnel is assessed, after which the screw is completely tightened.
If the initial length of the autograft with bone blocks exceeds 10 cm, there is a high probability of the bone block protruding out of the tibial canal.
To avoid pain in the patellofemoral joint in the postoperative period, the protruding part of the bone block is bitten off after fixation.
Before closing with soft tissues, sharp protruding bone edges and corners are smoothed with a rasp, and then the soft tissues are sutured.
Next, carefully examine the area of the tibial screw for bleeding; if necessary, perform thorough hemostasis using coagulation.
Control X-ray images in two projections are taken directly in the operating room.
The wounds are sutured tightly in layers; it is not recommended to install drainage, as it becomes an entry point for infection; if necessary (the appearance of effusion in the joint), a joint puncture is performed the next day.
A postoperative brace with a 0-180° lock is applied to the operated limb.
After the operation, a cold system is applied to the joint, which significantly reduces the number of complications such as paraarticular edema and joint effusion.
For the first time in Russia, the Central Institute of Traumatology and Orthopedics has begun using a more universal method of fixing autografts with Rigidfix polylactic acid pins and the latest generation Mi-La-Gro interference screw for grafts with bone blocks. The universality of the method lies in its application to both soft tissue grafts and grafts with bone blocks. The advantages of the method are the absence of the risk of damaging the soft tissue part of the autograft with bone blocks at the time of fixation, rigid fixation, and the absence of problems with removing the fixing pins due to their resorption. The rigidity of the primary fixation and the tight fit of the bone blocks of the graft are ensured by the swelling of the pins and the resulting compression.

