Medical expert of the article
New publications
Cryptogenic epilepsy with seizures in adults
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
According to the international classification in force until last year, symptomatic or secondary epilepsy, caused by damage to brain structures, idiopathic, primary (an independent, presumably hereditary disease) and cryptogenic epilepsy were distinguished. The latter option means that modern diagnostics have not established any causes for periodic epileptic seizures, and hereditary predisposition is also not traced. The very concept of "cryptogenic" is translated from Greek as "unknown origin" (kryptos - secret, secret, genos - generated).
Science does not stand still and, perhaps, soon the origin of periodic epileptic seizures of unknown etiology will be established. Experts suggest that cryptogenic epilepsy is a secondary symptomatic disease, the genesis of which cannot be established with the current level of diagnostics.
Epidemiology
Epilepsy and epileptic syndromes are very common neurological pathologies, which often lead to serious consequences. Manifestation of epileptic seizures can occur in people of any gender and at any age. It is believed that approximately 5% of the world's population has experienced at least one seizure in their lifetime.
Every year, epilepsy or epileptic syndrome is diagnosed in an average of every 30-50 people out of 100 thousand people living on Earth. Most often, epileptic seizures occur in infants (from 100 to 233 cases per 100 thousand people). The peak of manifestation falls on the perinatal period, then the incidence rate decreases almost by half. The lowest rates are in people from 25 to 55 years old - about 20-30 cases per 100 thousand people. Then the likelihood of epileptic seizures increases and from the age of 70 the incidence rate is 150 cases or more per 100 thousand people.
The causes of epilepsy are established in approximately 40% of cases, so a disease of unknown etiology is not uncommon. Infantile spasms (West syndrome), which is a cryptogenic epilepsy, is diagnosed in four- to six-month-old children, with one child with such a diagnosis occurring on average among 3,200 infants.
Causes cryptogenic epilepsy
The basis for diagnosing epilepsy are periodic seizures, the cause of which is an abnormally strong electrical discharge, which is the result of synchronization of the activity of brain cells in all frequency ranges, which is externally expressed in the appearance of sensory-motor, neurological and mental symptoms.
For an epileptic seizure to occur, the so-called epileptic neurons must be present, which are characterized by instability of the resting potential (the difference in potentials of an unexcited cell on the inner and outer sides of its membrane). As a result, the action potential of an excited epileptic neuron has an amplitude, duration, and frequency that are significantly higher than normal, which leads to the development of an epileptic seizure. It is believed that seizures occur in people with a hereditary predisposition to such shifts, that is, groups of epileptic neurons capable of synchronizing their activity. Epileptic foci also form in areas of the brain with altered structure due to injuries, infections, intoxications, and the development of tumors.
So, in patients diagnosed with cryptogenic epilepsy, modern neuroimaging methods do not detect any abnormalities in the structure of the brain matter, and there is no epileptic in the family history. Nevertheless, patients experience fairly frequent epileptic seizures of various types that are difficult to treat (possibly precisely because their cause is unclear).
Accordingly, the known risk factors for the occurrence of epileptic seizures – genetics, disruption of brain structure, metabolic processes in its tissues, consequences of head injuries or infectious processes – are not detected during examinations and surveys.
According to the new classification of epilepsies of 2017, six etiological categories of the disease are distinguished. Instead of symptomatic, it is now recommended to determine the type of epilepsy by the established cause: structural, infectious, metabolic, immune, or a combination of them. Idiopathic epilepsy assumed the presence of a hereditary predisposition and is now called genetic. The term "cryptogenic" has been replaced by "unknown etiological factor", which made the meaning of the wording clearer, but did not change.
The pathogenesis of epilepsy is presumably as follows: formation of an epileptic focus, i.e. a community of neurons with impaired electrogenesis → creation of epileptic systems in the brain (with excessive release of excitatory mediators, a “glutamate cascade” is launched, affecting all new neurons and contributing to the formation of new foci of epileptogenesis) → formation of pathological interneuronal connections → generalization of epilepsy occurs.
The main hypothesis of the mechanism of epilepsy development is the assumption that the pathological process is triggered by a violation of the equilibrium state between excitatory neurotransmitters (glutamate, aspartate) and those responsible for inhibition processes (γ-aminobutyric acid, taurine, glycine, norepinephrine, dopamine, serotonin). What exactly violates this equilibrium in our case remains unknown. However, as a result, the cell membranes of neurons suffer, the kinetics of ion flows is disrupted - ion pumps are inactivated and, conversely, ion channels are activated, the intracellular concentration of positively charged ions of potassium, sodium and chlorine is disrupted. Pathological ion exchange through destructured membranes determines changes in the level of cerebral blood flow. Dysfunction of glutamate receptors and the production of autoantibodies to them cause epileptic seizures. Periodically recurring, excessively intense neural discharges, realized in the form of epileptic seizures, lead to profound disturbances in metabolic processes in the cells of the brain substance and provoke the development of the next seizure.
The specificity of this process is the aggressiveness of the neurons of the epileptic focus in relation to the still unchanged areas of the brain, allowing them to subjugate new areas. The creation of epileptic systems occurs in the process of forming pathological relationships between the epileptic focus and the structural components of the brain that are capable of activating the mechanism of epilepsy development. Such structures include: the thalamus, the limbic system, the reticular formation of the middle part of the brainstem. The relationships that arise with the cerebellum, the caudate nucleus of the subcortex, the anterior orbital cortex, on the contrary, slow down the development of epilepsy.
In the process of disease development, a closed pathological system is formed – the epileptic brain. Its formation ends with a disorder of cellular metabolism and interaction of neurotransmitters, cerebral circulation, increasing atrophy of cerebral tissues and vessels, activation of specific cerebral autoimmune processes.
Symptoms cryptogenic epilepsy
The main clinical manifestation of this disease is an epileptic seizure. Epilepsy is suspected when the patient has had at least two reflex (unprovoked) epileptic seizures, the manifestations of which are very diverse. For example, epilepsy-like seizures caused by high temperature and not occurring in a normal state are not epilepsy.
Patients with cryptogenic epilepsy may experience seizures of different types, and quite frequently.
The first signs of the disease development (before the appearance of full-fledged epileptic seizures) may remain unnoticed. The risk group includes people who suffered from febrile seizures in early childhood, with a conclusion about increased seizure readiness. In the prodromal period, sleep disorders, increased irritability, and emotional lability may be observed.
In addition, attacks do not always occur in the classic generalized form with falls, convulsions, and loss of consciousness.
Sometimes the only early signs are speech disorders, the patient is conscious but does not speak or answer questions, or periodic short fainting spells. This does not last long - a couple of minutes, so it goes unnoticed.
Simple focal or partial (local, limited) seizures occur more easily, the manifestations of which depend on the location of the epileptic focus. The patient does not lose consciousness during the paroxysm.
During a simple motor seizure, tics, twitching of the limbs, muscle cramps, rotational movements of the torso and head may be observed. The patient may make inarticulate sounds or remain silent, not answering questions, smacking their lips, licking their lips, and making chewing movements.
Simple sensory seizures are characterized by paresthesia – numbness of various parts of the body, unusual taste or smell sensations, usually unpleasant; visual disturbances – flashes of light, a grid, spots before the eyes, tunnel vision.
Vegetative paroxysms are manifested by sudden pallor or hyperemia of the skin, increased heart rate, jumps in blood pressure, constriction or dilation of the pupils, discomfort in the stomach area up to pain and vomiting.
Mental seizures are manifested by derealization/depersonalization, panic attacks. As a rule, they are precursors to complex focal seizures, which are already accompanied by impaired consciousness. The patient understands that he is having a seizure, but cannot seek help. The events that happened to him during the seizure are erased from the patient's memory. The person's cognitive functions are impaired - a feeling of unreality of what is happening, new changes within oneself appears.
Focal seizures with subsequent generalization begin as simple (complex), turning into generalized tonic-clonic paroxysms. They last about three minutes and turn into deep sleep.
Generalized seizures occur in a more severe form and are divided into:
- tonic-clonic, occurring in the following sequence: the patient loses consciousness, falls, his body bends and stretches out in an arc, convulsive twitching of muscles throughout the body begins; the patient's eyes roll back, his pupils are dilated at this moment; the patient screams, turns blue as a result of stopping breathing for several seconds, foamy hypersalivation is observed (the foam may acquire a pinkish tint due to the presence of blood in it, which indicates biting of the tongue or cheek); sometimes involuntary emptying of the bladder occurs;
- myoclonic seizures look like intermittent (rhythmic and arrhythmic) twitching of muscles for several seconds throughout the body or in certain areas of the body, which look like flapping of limbs, squatting, clenching of hands into fists and other monotonous movements; consciousness, especially in focal seizures, is preserved (this type is more often observed in childhood);
- absences - non-convulsive seizures with a short-term (5-20 seconds) loss of consciousness, expressed in the fact that a person freezes with open, expressionless eyes and does not react to stimuli, usually does not fall, upon coming to, continues the interrupted activity and does not remember the seizure;
- atypical absences are accompanied by falls, involuntary emptying of the bladder, are longer lasting and occur in severe forms of the disease, combined with mental retardation and other symptoms of mental disorders;
- atonic seizures (akinetic) - the patient falls sharply as a result of loss of muscle tone (in focal epilepsies - there may be atony of individual muscle groups: facial - drooping of the lower jaw, cervical - the patient sits or stands with his head hanging), the duration of the seizure is no more than one minute; atony in absences occurs gradually - the patient slowly sinks, in isolated atonic seizures - falls sharply.
In the post-seizure period, the patient is lethargic and inhibited; if he is not disturbed, he falls asleep (especially after generalized seizures).
Types of epilepsy correspond to types of seizures. Focal (partial) seizures develop in a local epileptic focus, when an abnormally intense discharge encounters resistance in neighboring areas and is extinguished without spreading to other parts of the brain. In such cases, cryptogenic focal epilepsy is diagnosed.
The clinical course of the disease with a limited epileptic focus (focal form) is determined by its location.
Most often, damage to the temporal region is observed. The course of this form is progressive, seizures are often of a mixed type, lasting for several minutes. Cryptogenic temporal epilepsy outside of seizures is manifested by headaches, constant dizziness, nausea. Patients with this form of localization complain of frequent urination. Before the seizure, patients feel an aura-harbinger.
The lesion may be located in the frontal lobe of the brain. The seizures are characterized by suddenness without a prodromal aura. The patient has head twitching, eyes roll under the forehead and to the side, automatic, fairly complex gesticulation is characteristic. The patient may lose consciousness, fall, and have tonic-clonic muscle spasms throughout the body. With this localization, a series of short-term seizures are observed, sometimes with a transition to generalized and / or status epilepticus. They can begin not only during the daytime wakefulness, but also during night sleep. Cryptogenic frontal epilepsy, developing, causes mental disorders (violent thinking, derealization) and the autonomic nervous system.
Sensory seizures (sensation of warm air moving across the skin, light touches) combined with convulsive twitching of body parts, speech and motor disorders, atony, accompanied by urinary incontinence.
Localization of the epileptic focus in the orbital-frontal region is manifested by olfactory hallucinations, hypersalivation, epigastric discomfort, as well as speech disorders, cough and laryngeal edema.
If electrical hyperactivity cascades across all parts of the brain, a generalized seizure develops. In this case, the patient is diagnosed with cryptogenic generalized epilepsy. In this case, seizures are characterized by intensity, loss of consciousness, and end with the patient falling into prolonged sleep. Upon awakening, patients complain of headaches, visual phenomena, fatigue, and emptiness.
There is also a combined (when both focal and generalized seizures occur) and unknown type of epilepsy.
Cryptogenic epilepsy in adults is considered, and not without reason, secondary with an unspecified etiological factor. It is characterized by sudden seizures. Outside of clinical symptoms, epileptics have an unstable psyche, explosive temperament, and a tendency to aggression. The disease usually begins with manifestations of some focal form. As the disease progresses, the lesions spread to other parts of the brain; the advanced stage is characterized by personal degradation and pronounced mental deviations, and the patient becomes socially maladjusted.
The disease has a progressive course and the clinical symptoms of epilepsy change depending on the stage of development of epilepsy (the degree of prevalence of the epileptic focus).
Complications and consequences
Even in mild cases of focal epilepsy with isolated, rare seizures, nerve fibers are damaged. The disease has a progressive course, with one seizure increasing the likelihood of the next, and the area of brain damage expanding.
Generalized frequent paroxysms have a destructive effect on brain tissue and can develop into status epilepticus with a high probability of a fatal outcome. There is also a risk of cerebral edema.
Complications and consequences depend on the degree of damage to brain structures, the severity and frequency of seizures, concomitant diseases, the presence of bad habits, age, the adequacy of the chosen treatment tactics and rehabilitation measures, and the responsible attitude to treatment of the patient himself.
At any age, injuries of varying severity can occur during falls. Hypersalivation and a tendency to gag during a seizure increase the risk of liquid substances entering the respiratory system and developing aspiration pneumonia.
In childhood, there is instability of mental and physical development. Cognitive abilities often suffer.
The psycho-emotional state is unstable – children are irritable, capricious, often aggressive or apathetic, they lack self-control, and they adapt poorly to the group.
In adults, these risks are compounded by injuries when performing work that requires increased attention. During seizures, the tongue or cheek is bitten.
Epileptics have an increased risk of developing depression, mental disorders, and social maladjustment. People suffering from epilepsy are limited in physical activity and choice of profession.
Diagnostics cryptogenic epilepsy
In the diagnosis of epilepsy, many different methods are used to help differentiate this disease from other neurological pathologies.
First of all, the doctor must listen to the complaints of the patient or his parents, if it is a child. An anamnesis of the disease is compiled - details of the manifestation, the specifics of the course (frequency of seizures, fainting, the nature of convulsions and other nuances), the duration of the disease, the presence of similar diseases in the patient's relatives. This survey allows us to assume the type of epilepsy and the localization of the epileptic focus.
Blood and urine tests are prescribed to assess the general condition of the body, the presence of factors such as infections, intoxications, biochemical disorders, and to determine the presence of genetic mutations in the patient.
Neuropsychological testing is performed to assess cognitive abilities and emotional status. Periodic monitoring allows assessing the impact of the disease on the nervous system and psyche, and also helps to determine the type of epilepsy.
However, first of all, this is an instrumental diagnostics, thanks to which it is possible to assess the intensity of electrical activity of the brain regions (electroencephalography), the presence of vascular malformations, neoplasms, metabolic disorders, etc. in its regions.
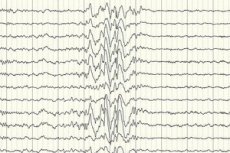
Electroencephalography (EEG) is the main diagnostic method, as it shows deviations from the norm in brain wave intensity even outside of an attack – increased seizure readiness of certain areas or the entire brain. The EEG pattern of cryptogenic partial epilepsy is spike-wave or sustained slow-wave activity in certain parts of the brain. Using this study, the type of epilepsy can be determined based on the specificity of the electroencephalogram. For example, West syndrome is characterized by irregular, virtually unsynchronized arrhythmic slow waves with abnormally high amplitude and spike discharges. In most cases of Lennox-Gastaut syndrome, the electroencephalogram during wakefulness reveals irregular generalized slow spike-wave activity with a frequency of 1.5-2.5 Hz, often with amplitude asymmetry. During night rest, this syndrome is characterized by the registration of fast rhythmic discharges with a frequency of approximately 10 Hz.
In the case of cryptogenic epilepsy, this is the only way to confirm its presence. Although there are cases when even immediately after a seizure, the EEG does not register changes in the shape of brain waves. This may be a sign that changes in electrical activity occur in the deep structures of the brain. Changes in the EEG may also be present in patients without epilepsy.
Modern methods of neurovisualization are necessarily used - computer, resonance, positron emission tomography. This instrumental diagnostics allows to evaluate changes in the structure of the brain substance due to injuries, congenital anomalies, diseases, intoxications, to detect neoplasms, etc. Positron emission tomography, which is also called functional MRI, helps to identify not only structural, but also functional disorders.
Deeper foci of abnormal electrical activity can be detected by single-photon emission computed tomography, and resonance spectroscopy can detect disturbances in biochemical processes in the brain tissue.
An experimental and not widespread diagnostic method is magnetoencephalography, which records magnetic waves emitted by neurons in the brain. It allows us to study the deepest structures of the brain, inaccessible to electroencephalography.
Differential diagnosis
Differential diagnostics are performed after conducting the most comprehensive studies. The diagnosis of cryptogenic epilepsy is made by excluding other types and causes of epileptic seizures identified during the diagnostic process, as well as hereditary predisposition.
Not all medical institutions have the same diagnostic potential, so such a diagnosis requires further diagnostic research at a higher level.
Treatment cryptogenic epilepsy
There is no single method for treating epilepsy, however, clear standards have been developed that are followed in order to improve the quality of treatment and the lives of patients.
Prevention
Since the causes of this particular type of epilepsy have not been established, preventive measures have a general focus. A healthy lifestyle - no bad habits, good nutrition, physical activity provides good immunity and prevents the development of infections.
Paying close attention to your health, timely examination and treatment of diseases and injuries also increases the likelihood of avoiding this disease.
Forecast
Cryptogenic epilepsy manifests at any age and does not have a specific symptom complex, but manifests itself in a very diverse way - different types of seizures and types of syndromes are possible. To date, there is no single method for a complete cure for epilepsy, but antiepileptic treatment helps in 60-80% of cases of all types of diseases.
On average, the disease lasts for 10 years, after which the seizures may stop. However, 20 to 40% of patients suffer from epilepsy their entire lives. About a third of all patients with any type of epilepsy die from causes associated with it.
For example, cryptogenic forms of West syndrome have an unfavorable prognosis. In most cases, they develop into Lennox-Gastaut syndrome, mild forms of which are amenable to drug control, while generalized forms with frequent and severe seizures can remain for life and be accompanied by severe intellectual degradation.
In general, the prognosis depends very much on the time of the start of treatment; when it is started in the early stages, the prognosis is more favorable.
Epilepsy can result in lifelong disability. If a person develops a persistent health disorder as a result of the disease, leading to a limitation of life activities, then this is determined by a medical and social examination. It also makes a decision on assigning a specific disability group. You should first contact your attending physician on this issue, who will introduce the patient to the commission.


 [
[