Medical expert of the article
New publications
Perineum
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The perineum is a complex of soft tissues (skin, muscles, fascia) that closes the exit from the pelvic cavity.
The perineum occupies the area bounded in front by the lower edge of the pubic symphysis, behind by the tip of the coccyx, and on the sides by the lower branches of the pubic and ischial bones and the ischial tuberosities. If we take the ischial tuberosities as the extreme lateral points of the perineum, the lower point of the pubic symphysis in front, and the tip of the coccyx behind, then the outline of the perineum can be compared to a rhombus.
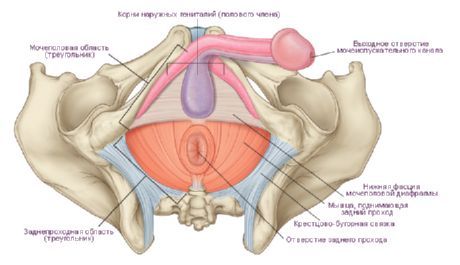
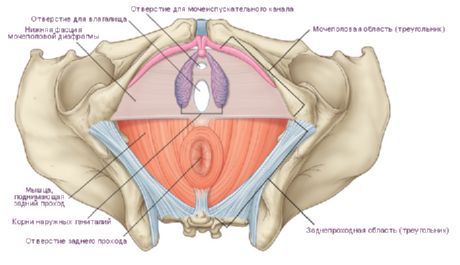
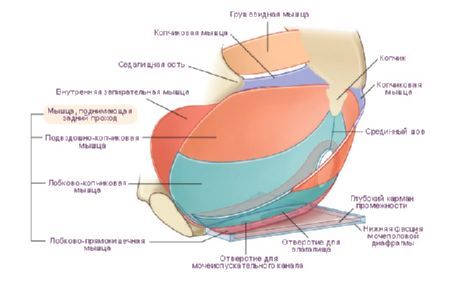
The transverse line connecting the ischial tuberosities divides this region into two parts shaped like triangles. The anterior-upper part is called the urogenital region (regio urogenitalis), and the lower-posterior part is called the anal region (regio analis). Within the urogenital region is the urogenital diaphragm, and in the anal region is the pelvic diaphragm. Both diaphragms are adjacent to each other with their bases, and their apices are directed respectively to the pubic symphysis and coccyx.
In a narrow sense, the perineum is understood to be the area located between the external genitalia in front and the anus in the back. This area corresponds to the tendinous center of the perineum (centrum tendineum perinei). In women, this area extends from the posterior edge of the genital slit to the anterior edge of the anus, and in men, from the posterior edge of the scrotum to the anterior edge of the anus. In the anteroposterior direction, a dark stripe runs across the skin of the perineum - the median perineal suture (raphe perineum), which in men continues in front into the suture of the scrotum.
The urogenital diaphragm (urogenital area) and the pelvic diaphragm (anal area) are muscular-fascial plates formed by two layers of muscles (superficial and deep) and fascia. In the anal area, the muscles of the pelvic diaphragm lie between its upper and lower fascia. The muscles of the urogenital diaphragm are located in such a way that the deep layer is enclosed between the upper and lower fascia of the urogenital diaphragm. This entire muscular-fascial plate is covered by the pelvic fascia on the side of the pelvic cavity and by the superficial fascia on the outside (from below).
The urogenital diaphragm occupies the anterior part of the perineum and has the shape of a triangle, the apex of which is directed toward the pubic symphysis. The sides are limited by the lower branches of the pubic and ischial bones, the base corresponds to the line connecting the ischial tuberosities. The urethra passes through the urogenital diaphragm in men, and the urethra and vagina in women.
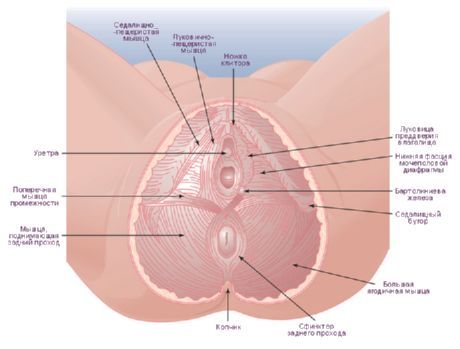
The muscles of the urogenital diaphragm are divided into superficial and deep. The superficial muscles include 3 muscles: the superficial transverse perineal muscle, the ischiocavernosus and the bulbospongiosus
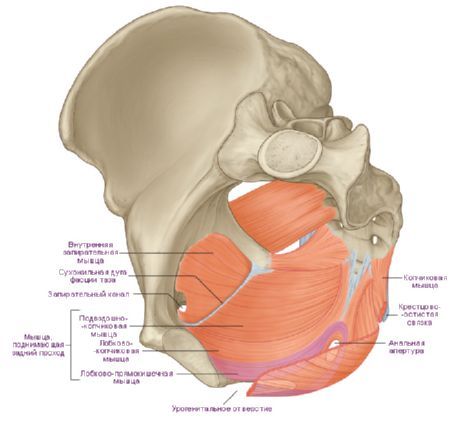
The superficial transverse perineal muscle (m.transversus perinei superficialis) is paired and lies in the deep layer of subcutaneous fat. It begins on the lower branch of the ischium near the ischial tuberosity, goes transversely towards the same muscle on the other side and ends in the tendinous center of the perineum, formed by thin flat tendons of these muscles. Some of the fibers of this muscle are woven into the external sphincter of the anus and into the bulbospongiosus muscle of the opposite side. The superficial transverse muscles participate in strengthening the tendinous center of the perineum.
The ischiocavernosus muscle (m.ischiocavernosus) is also paired, originates on the lower branch of the ischium. Its medial side is adjacent to the crus of the penis (in men) or the clitoris (in women). The muscle is attached to the cavernous body, part of this muscle with a tendon ending continues to the back of the penis, where it connects with the fibers of the same muscle on the opposite side. In women, this muscle is smaller than in men. When contracted, the ischiocavernosus muscles promote erection of the penis or clitoris by squeezing the venous vessels.
The bulbospongiosus muscle (m.bulbospongiosus) in men originates on the suture and the lower surface of the bulb of the penis. The fibers go forward, laterally and upward, embrace the bulb and spongy body of the penis on the right and left and are attached to its protein tunica and superficial fascia on the back of the penis. When contracting, the muscle compresses the bulb, cavernous bodies and dorsal vein of the penis, as well as the bulbourethral glands, participates in erection, and also facilitates the ejection of sperm and urine from the urethra. In women, the bulbospongiosus muscle is paired, embraces the vagina in the area of its opening (m.sphincter urethrovaginalis). The muscle originates on the tendinous center of the perineum and the external sphincter of the anus, is attached to the dorsal surface of the clitoris, intertwining with its protein tunica. On its way, the muscle is adjacent to the vestibular glands from below. When contracting, it narrows the entrance to the vagina, compresses the large vestibular gland, the vestibular bulb, and the veins coming out of it.
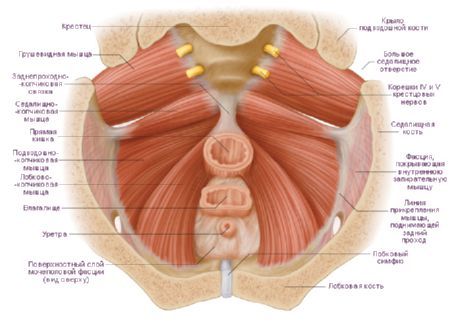
The deep muscles of the urogenital diaphragm include the transverse perineal muscle and the sphincter muscle of the urethra.
The deep transverse perineal muscle (m.transversus perinei profundus) is paired, has the appearance of a thin plate, and begins on the branches of the ischium and pubis. Along the midline of the perineum, its flat tendon connects with the tendon of the same muscle on the other side and participates in the formation of the tendinous center of the perineum. Both muscles strengthen the urogenital diaphragm.
The muscle - the sphincter of the urethra (m.sphincter urethrae) begins partly on the lower branches of the pubic bones. The muscle bundles have a predominantly circular direction, covering the membranous part of the urethra in men, and the urethra in women. In men, the fiber bundles of this muscle are attached to the prostate gland, and in women they are woven into the wall of the vagina. The muscle is an arbitrary constrictor of the urethra. In women, the muscle also constricts the vagina.
Pelvic diaphragm
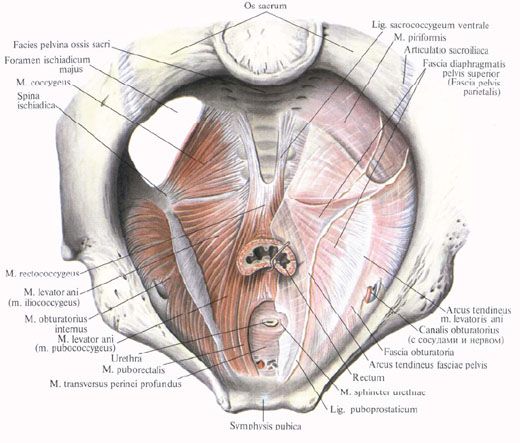
The pelvic diaphragm (diaphragma pelvis) occupies the back of the perineum and has the shape of a triangle, the apex of which is directed toward the coccyx, and the corners are directed toward the ischial tuberosities. The final section of the rectum passes through the pelvic diaphragm in both men and women.
The superficial layer of the pelvic diaphragm muscles is represented by an unpaired muscle - the external anal sphincter (m.sphincter ani externus). This muscle lies under the skin surrounding the terminal section of the rectum. It consists of several bundles, the most superficial of which end in the subcutaneous tissue. The bundles, starting at the top of the coccyx, cover the anus and end in the tendinous center of the perineum. The deepest bundles, surrounding the lower section of the rectum, are adjacent to the muscle that lifts the anus. All bundles of the external anal sphincter, when contracting, compress (close) the opening of the anus.
The deep muscles of the pelvic diaphragm include two muscles that form the posterior section of the floor of the pelvic cavity. The muscle that lifts the anus (m.levator ani) is paired, has the shape of a thin triangular plate, forms a funnel with a similar muscle on the other side, the wide part facing upward. The lower parts of both muscles, narrowing, embrace the rectum in the form of a loop. The muscle originates on the lateral wall of the pelvis in several bundles. The anterior bundles begin on the inner surface of the lower branch of the pubic bone, the lateral ones - on the tendinous arch of the muscle that lifts the anus (arcus tendineum musculi levatoris ani). The tendinous arch is an arcuate thickening of the pelvic fascia in the place where it forms the obturator fascia. The bundles of the right and left muscles that lift the anus are directed downward and backward, connect with each other, and embrace the rectum. Some of the fibers of these muscles are woven into the prostate gland (in men), the wall of the vagina (in women), and also into the wall of the bladder and rectum; the muscles themselves end at the top of the coccyx in the form of the anococcygeal ligament (lig. anococcygeum). When the muscle that lifts the anus contracts, the pelvic floor is strengthened and raised, the lower (terminal) section of the rectum is pulled forward and upward, which is compressed. In women, this muscle also compresses the entrance to the vagina and brings the back wall of the vagina closer to the front.
The coccygeus muscle (m.coccygeus) is paired, originates on the sciatic spine and sacrospinous ligament, runs medially and posteriorly; attaches to the lateral edge of the coccyx and the apex of the sacrum. The bundles of this muscle are adjacent to the sacrospinous ligament on the medial side, and are partly woven into it, strengthening the posterior part of the pelvic diaphragm.
The bottom of the pelvic cavity is closed by the pelvic diaphragm (diaphragma pelvis), which is complemented in front by the urogenital diaphragm (diaphragma urogenitale).
The pelvic diaphragm consists of both muscles that lift the anus (m. levator ani), the coccygeal muscle and the external sphincter of the rectum (m. sphincter ani externum).
The muscle that lifts the anus is paired, has a triangular shape and consists of the pubococcygeus (m. pubo-coccygeus), iliococcygeus and ischiococcygeus (m. ileo-coccygeus). The entire muscular mass of the pelvic diaphragm has the shape of an inverted bowl or dome, with the concave surface facing upward and the convex surface facing downward. In the middle of this dome there is a genital slit through which the urethra, vagina and rectum come out.
The urogenital diaphragm has a triangular shape. In its anterior section is the urogenital sphincter (sphincter uro-genitale), in the posterior section is the transverse deep muscle of the perineum (m. transversus perinei profundus), connected with the muscles of the superficial layer and levators.
The outer layer of the pelvic floor muscles includes the external and internal anal sphincters (m. sphincter ani externus, internus), the bulbocavernosus muscle (m. bulbo-cavernosus), the superficial transverse perineal muscle (m. transversus perinei superficialis) and the ischiocavernosus muscle (m. ischiocavernosus). The outer layer of the pelvic floor muscles merges with its tendons into a strong fibrous formation - the tendinous center of the perineum (centrum tendineum perinei).
The blood supply to the floor of the pelvic cavity is carried out mainly by branches of the internal genital vessels (a. pudenda interna). The blood supply to the perineum is carried out by the external and internal genital vessels (a. pudenda externa et interna).
The innervation of the pelvic floor muscles occurs through the branches of the sacral plexus (pli. sacralis), the external genital nerve (n. pudendus), and the lumbar plexus (pl. lumbalis).
The muscles of the pelvic floor are essential in maintaining intra-abdominal pressure and fixing the abdominal and pelvic organs.
Vessels and nerves of the perineum
The blood supply to the perineum is provided by the branches of the internal (deep) pudendal artery, which exits the pelvic cavity through the large sciatic opening, goes around the sciatic spine, and then enters the ischiorectal fossa through the small sciatic opening. Here the artery gives off several large branches: the inferior rectal artery, the perineal artery, and the dorsal artery of the penis or clitoris. Venous blood flows through the veins of the same name into the internal iliac vein. The lymphatic vessels flow into the superficial inguinal lymph nodes.
The perineum is innervated by the branches of the genital nerve: by the nerve fibers of the lower rectal nerves, perineal nerves, and also the anal-coccygeal nerves - branches of the coccygeal nerve.
Development of the perineum
In the embryo, during development, the cloacal cavity is divided into a ventral section, the urogenital sinus, and a dorsal section, the rectum, due to the urethra-rectal septum growing into it frontally. The urethra-rectal septum grows caudally, reaching the cloacal plate, which is then divided into an anterior part, the urogenital plate, and a posterior part, the anal plate. Each plate breaks through independently, resulting in the formation of the openings of the anus and the urogenital opening. Around these openings, muscle fibers are formed from the mesoderm grown into the thickness of the anal and urogenital plates. Initially, sphincters are formed from these fibers, and then the muscle that lifts the anus (in the area of the anal plate), the perineum, and the remaining muscles that form the basis of the urogenital diaphragm.


 [
[