Medical expert of the article
New publications
Compression fracture of thoracic vertebrae and back pain
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
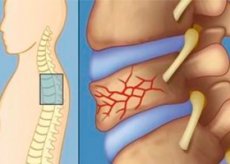
Compression fracture of the thoracic vertebrae is one of the most common causes of thoracic spine pain. Compression fracture of the spine is often a consequence of osteoporosis, but can also occur as a result of a spinal acceleration-deceleration injury. In patients with osteoporosis, primary tumor, or metastatic disease affecting the thoracic vertebrae, the fracture may occur with coughing (cough fracture) or spontaneously.
The pain and disability associated with a vertebral fracture are determined by the severity of the injury (i.e., the number of vertebrae involved) and the nature of the neural damage (compression of spinal nerves or spinal cord). The pain associated with a thoracic vertebral compression fracture can range from a dull, deep ache (with minimal vertebral compression and no nerve compression) to a severe, sharp, shooting pain that limits the patient's ability to walk or cough.
Symptoms of compression fracture of the thoracic vertebrae
Compression fractures of the thoracic vertebrae are aggravated by deep breathing, coughing, and any movement of the spine. Palpation and percussion of the affected vertebra may cause pain and reflex spasm of the paravertebral muscles. If trauma is the cause of the fracture, a hematoma or ecchymosis may be present over the fracture site, and the clinician must be aware of the possibility of injury to the rib cage, thoracic organs, and abdominal organs. Injury to spinal nerves may cause intestinal obstruction and severe pain, leading to axial muscle rigidity and further impairment of breathing and ambulation. Failure to aggressively treat this pain and muscle rigidity may lead to hypoventilation, atelectasis, and eventually pneumonia.
Survey
A general radiography of the spine is indicated to exclude other hidden fractures and bone pathology, including a tumor. MRI can reveal the nature of the fracture and differentiate benign causes of pain from malignant ones. In the presence of trauma, radionuclide scanning (scintigraphy) of the bone can be informative to exclude hidden fractures of the vertebrae and sternum. If there was no trauma, then bone densitometry, serum protein electrophoresis and a study for hyperparathyroidism are prescribed to assess osteoporosis. Based on the clinical picture, a study of the general blood test, the level of prostate-specific antigen, ESR, and the level of antinuclear antibodies may also be possible.
If hidden tumor processes and significant injuries are suspected, CT of the chest organs is prescribed. Electrocardiography is indicated to exclude closed heart injuries in all patients with traumatic sternum fractures or crushing trauma to the anterior spine. Injection techniques should be used early to prevent pulmonary complications.
Differential diagnosis
In trauma, the diagnosis of a thoracic vertebral compression fracture is usually clear. In cases of spontaneous fracture secondary to osteoporosis and metastatic disease, the diagnosis may be less clear. In such cases, pain from an occult vertebral compression fracture is often mistaken for pain of cardiac or visceral (cholelithiasis) etiology, leading to a visit to the emergency department and unnecessary cardiac and gastrointestinal care. An acute strain of the thoracic axial muscles may be mistaken for a thoracic compression fracture, especially if the patient is coughing. Because the pain of herpes zoster precedes the rash by 3 to 7 days, it may be mistaken for a vertebral compression fracture.
Clinical features of compression fracture of the thoracic vertebrae
Compression fractures of the thoracic vertebrae are a common cause of spinal pain. Accurate diagnosis is necessary to properly treat these painful conditions and avoid missing serious thoracic and abdominal pathology. Pharmacological agents usually provide adequate pain control. If necessary, a thoracic epidural block can provide significant pain relief.
Treatment of compression fracture of the thoracic vertebrae
Initial treatment of pain in thoracic vertebral compression fractures includes a combination of simple analgesics and nonsteroidal anti-inflammatory drugs. Antiresorptive drugs with analgesic effect (synthetic salmon calcitonin) may be prescribed. If these drugs do not sufficiently relieve pain, short-acting opioid analgesics such as tramadol may be a reasonable next step. Because opioid analgesics can depress the cough and respiratory centers, the patient should be instructed in adequate airway clearance techniques. Local heat and cold applications or orthopedic devices (Cash corset) may provide symptomatic relief. In patients who do not respond to such therapy, thoracic epidural block with local anesthetics and steroids is indicated. Kyphoplasty with cemented fixation of the fracture site is a good choice if decreased mobility becomes a problem due to pain.
Complications and diagnostic errors
The main problem in the management of patients with suspected thoracic vertebral compression fractures is the late diagnosis of spinal cord compression or recognition of the metastatic nature of the fracture. In patients with thoracic vertebral compression fractures, early pain control and early ambulation are necessary to prevent complications such as pneumonia and thrombophlebitis.


 [
[