Medical expert of the article
New publications
Complications after coronary stenting
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
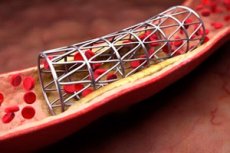
Stenting of heart vessels is considered one of the most reliable operations that allows restoring blood flow in a stenotic vessel. This, in turn, has a positive effect on the work of not only the heart itself, but also other organs, which, together with the blood flow, receive oxygen and nutrients necessary for their normal functioning.
The main advantage of the coronary stenting method is considered to be the low-trauma nature of the operation. After all, it does not require making incisions in the chest and exposing the heart, which is considered very dangerous with a high risk of fatal outcomes. And the recovery period after the same bypass surgery is much longer, plus it is more difficult.
Minimally invasive stenting rarely has negative consequences. The mortality rate of such operations is within 1-1.5%, which is considered low, and the risk of complications rarely exceeds 2% (most often we are talking about vascular complications). It is clear that the presence of pathologies listed in the paragraph describing relative contraindications to surgery somewhat worsens the prognosis, as a result of which the number of fatal outcomes and the likelihood of complications increases.
The risk of death increases if the operation is performed in case of myocardial infarction in combination with cardiogenic shock or if there is tandem stenosis, which increases the complexity and time of the operation.
As we mentioned, complications of coronary stenting are rare, but you still need to know about them. Some of them can occur in the coming days and weeks after the operation, others remind of themselves after six months or more. Early postoperative complications, given that operations are performed even on people with serious health pathologies, occur in 3-4 patients out of 100.
What immediate complications of coronary stenting can be diagnosed in patients undergoing surgery or during the operation:
- damage to the vessel during stent placement, internal bleeding,
- heart attack,
- stroke,
- allergic reactions or intolerance reactions that occur in response to the administration of contrast,
- the formation of a hematoma at the site of a puncture in the tissues of the thigh or arm, caused by bleeding from a damaged artery,
- severe bleeding from a wound, which is usually diagnosed in the case of a blood clotting disorder or failure to comply with the requirement to limit physical activity,
- disruptions in the functioning of the central nervous system and kidneys due to impaired cerebral or renal circulation,
- infection of the wound and penetration of infection into the bloodstream,
- vascular thrombosis (a “bare” stent creates irregularities on the vessel wall, as a result of which blood clots can actively stick to it, although this process can be prevented by using a frame with a drug coating).
The likelihood of such complications increases in the following cases:
- the patient has a history of allergic reactions,
- metabolic disorders (diabetes, obesity),
- problems with blood clotting,
- recent severe lung and heart diseases (pneumonia, arrhythmia, heart attack, etc.),
- kidney pathologies,
- old age,
- bad habits, such as smoking.
A remote complication that cannot be completely avoided even using the innovative stenting method is restenosis of the coronary arteries approximately six months after surgery (and sometimes much earlier). Restenosis is a repeated narrowing of the lumen of the vessels, which results in impaired blood circulation in them.
Restenosis can develop for 3 reasons:
- thrombus formation (drug-eluting stents solve this problem),
- collapse of the vessel lumen (a complication typical of balloon angioplasty, but the introduction of a stent creates a stable frame and does not allow the vessel walls to bend inward, changing the shape of the vessel),
- hyperplasia or proliferation of epithelial tissues of the intima (inner lining) of the coronary vessels.
The latter reason is precisely what causes restenosis inside the stent. However, none of the methods for solving the problem today gives a positive result that allows reducing the risk of developing such a complication, which, according to statistics, is about 20-40%.
Doctors call the following risk factors for the development of restenosis:
- hereditary predisposition to increased proliferation of vascular tissue,
- metabolic disorders, such as diabetes,
- large size of the stenotic area,
- discrepancy between the size of the stent and the parameters of the damaged area of the vessel (during urgent operations, the doctor does not have the opportunity to accurately select the appropriate stent, so they use the ones available).
When performing coronary stenting, doctors may use different types of stents:
- uncoated metal-based products (BMS - the simplest and oldest type of stent, which does not protect against stent formation at the site of frame placement and restenosis with increased proliferative activity of the neointima),
- products, the outer part of which, adjacent to the walls of blood vessels, is coated with medicinal substances that prevent cell proliferation (DES is a modernized stent that prevents intimal hyperplasia, but does not reduce the risk of thrombosis),
- bioengineered products (BES – stents, the coating of which contains antibodies that prevent the formation of blood clots in the early and late periods after surgery),
- biodegradable (decomposing inside the vessel) products (BVS – drug-coated stents that block the growth of connective tissue inside the vessel),
- dual drug-eluting stent products (DTS – the newest model of stent, which significantly reduces the risk of thrombosis and proliferative reactions).
Studies have shown that the use of drug-eluting stents reduces the likelihood of early and late complications by approximately 20-25%. Thanks to such products, coronary stenting is currently considered the most effective method for restoring the patency of heart vessels.


 [
[