Medical expert of the article
New publications
Cerebral hypoxia
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
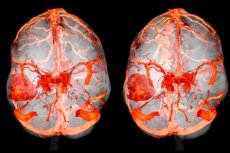
Cerebral hypoxia (sometimes called hypoxic cerebral ischemia) is a condition in which the brain does not receive enough oxygen, which can lead to brain damage or even necrosis (tissue death). Hypoxia can occur for a variety of reasons, including:
- Choking or suffocation: Lack of oxygen in the body can result from asphyxia, anemia, choking, or other problems with the respiratory system.
- Heart problems: Heart disorders can reduce the flow of oxygen to the brain.
- Stroke: Blockage of blood vessels or bleeding in the brain can also lead to hypoxia.
- Trauma: Traumatic injury associated with reduced blood supply to the brain can cause hypoxia.
- Airway obstruction: For example, asphyxia from gasping for breath or airway blockage.
Cerebral hypoxia can be a dangerous condition and can potentially lead to serious consequences including impaired brain function, paralysis and even death. Treatment depends on the cause and extent of hypoxia and may include restoring normal oxygen metabolism, treating the cause and rehabilitation. It is important to see a medical professional promptly if you suspect cerebral hypoxia.
Causes of the cerebral hypoxia
Cerebral hypoxia can occur due to various causes that can lead to a lack of oxygen to the brain. Some of the major causes include:
- Lack of oxygen in the inhaled air: This can occur when there is insufficient oxygen in the environment, such as in high altitude areas, underwater, or in situations involving breathing harmful gases.
- Respiratory problems: Lung disease, asthma, obstructive pulmonary disease, chronic obstructive pulmonary disease (COPD) and other breathing disorders can lead to difficulty getting oxygen to the lungs.
- Heart problems: Heart disease such as myocardial infarction, arrhythmias, or heart failure can reduce blood flow and therefore oxygen supply to the brain.
- Stroke: A stroke caused by a blocked blood vessel or brain hemorrhage can temporarily or permanently interrupt blood flow to part of the brain, which can lead to hypoxia.
- Trauma: Traumatic damage associated with a reduction in blood supply to the brain, such as when blood vessels are compressed as a result of a head injury, can also cause hypoxia.
- Asphyxia: Airway obstruction, such as that caused by gasping, choking, or airway blockage, can lead to rapid deterioration of oxygen supply.
- Blood abnormalities: Some blood disorders, such as anemia, can reduce the blood's ability to carry enough oxygen.
- Airway obstruction: For example, an allergic reaction resulting in swelling of the airways.
Pathogenesis
The pathogenesis (mechanism of development) of cerebral hypoxia is complex and includes several key steps:
- Reduced oxygen supply: Hypoxia can be caused by various factors such as suffocation, cardiovascular disease, choking, carbon monoxide poisoning and others. These factors can lead to a decrease in oxygen supply to the lungs and therefore to the bloodstream.
- Impaired oxygen transport: Oxygen must be bound to hemoglobin in red blood cells to be transported to tissues. Any abnormalities in the circulatory system, which may include anemia or other blood diseases, can reduce the blood's ability to transport oxygen.
- Decreased oxygen utilization: The brain is an organ that is highly dependent on oxygen to perform its functions. Hypoxia can lead to a decrease in the brain's ability to use oxygen to produce energy and maintain vital processes.
- Inflammation and Oxidative Stress: Hypoxia can cause inflammatory and oxidative processes in brain tissue, which can lead to brain cell damage. This can include activation of microglia and astrocytes, as well as increased free radical formation.
- Apoptosis (programmed cell death): In response to hypoxia, the brain can initiate the processes of apoptosis, which means the death of some brain cells in an attempt to preserve viable cells.
- Recovery from hypoxia: After a period of hypoxia has ended, the brain may attempt to restore normal functioning and utilize adaptation mechanisms.
Symptoms of the cerebral hypoxia
Symptoms of cerebral hypoxia can vary depending on the severity and duration of the lack of oxygen, but may include the following:
- Headache: Head pain can be one of the first and most common symptoms.
- Vague consciousness: The patient may experience slowed thought processes, drowsiness, and confusion.
- Dizziness and unsteadiness: The patient may experience dizziness, loss of balance and coordination.
- Decreased activity level: The patient may become weak, apathetic, and unable to perform normal physical and mental tasks.
- Difficulty breathing: Shortness of breath, shortness of breath, and cyanosis (bluish coloration of the skin and mucous membranes) may be signs of hypoxia.
- Seizures: In some cases, cerebral hypoxia can cause seizures and loss of consciousness.
- Visual and auditory disturbances: The patient may experience changes in visual and auditory perception.
- Thought and behavioral changes: Hypoxia can cause changes in memory, attention, and behavior and emotional state.
- Loss of consciousness: In cases of severe cerebral hypoxia, loss of consciousness may occur.
Acute and chronic cerebral hypoxia are two different conditions that involve insufficient oxygen supply to the brain. They have different causes, symptoms and treatment.
-
Acute cerebral hypoxia:
- Causes: Acute cerebral hypoxia is usually associated with a sudden cessation of oxygen to the brain due to events such as asphyxiation, respiratory arrest, cardiac arrhythmia or heart attack, neonatal asphyxia, trauma with respiratory arrest, and other extraordinary circumstances.
- Symptoms: Symptoms of acute cerebral hypoxia may include loss of consciousness, confusion, unconsciousness, agitation, seizures and loss of motor function. This condition requires immediate medical attention and resuscitation.
-
Chronic cerebral hypoxia:
- Causes: Chronic cerebral hypoxia develops gradually and can be caused by chronic medical conditions such as chronic obstructive pulmonary disease (COPD), sleep apnea, heart failure, anemia, hyperventilation, chronic hypoxia at high altitudes, and other factors that reduce oxygen supply to the brain over time.
- Symptoms: Symptoms of chronic cerebral hypoxia may include headaches, increased fatigue, difficulty breathing, decreased cognitive function (memory, concentration, mental clarity), mood changes, and other neurological and psychological symptoms.
Treatment of acute cerebral hypoxia usually involves immediate restoration of oxygen supply and active resuscitation, while treatment of chronic cerebral hypoxia depends on the underlying cause and may include treatment of the underlying disease, reduction of risk factors, and long-term supportive therapy. It is important to see a physician for evaluation and treatment for any symptoms of cerebral hypoxia.
Cerebral hypoxia in cervical osteochondrosis
Cervical osteochondrosis (also known as cervical spine osteochondrosis) can be one of the causes of cerebral hypoxia, as it can affect the blood supply to the brain through compression of blood vessels and nerve structures in the cervical spine area.
Cervical osteochondrosis can cause the following changes that can affect the blood supply to the brain:
- Vascular compression: The anterior and lateral cervical vertebrae can displace or put pressure on the blood vessels traveling to the brain. This can reduce blood flow to the brain and therefore oxygen levels.
- Nerve root compression: Compression of nerve roots in the cervical spine can also affect the function of the heart and blood vessels, which can impair blood supply to the brain.
- Muscle tension: The pain and muscle tension associated with osteochondrosis can also increase the need for oxygen and increase the risk of hypoxia.
Symptoms of cerebral hypoxia may include headaches, dizziness, memory impairment, impaired motor coordination, and other neurological symptoms. However, it is important to realize that brain hypoxia can be caused by other reasons as well, and only a doctor can diagnose and determine the exact cause of the symptoms.
If you suspect cerebral hypoxia associated with cervical degenerative disc disease, you should see your doctor for necessary tests, including a cervical spine examination and evaluation of blood flow to the brain. Treatment may include osteochondral management, physical therapy, medications to improve blood flow, and other interventions depending on the problems identified.
Cerebral hypoxia in a child
It is a serious condition in which the brain does not get enough oxygen. Hypoxia can occur in newborns and children for different reasons and have different degrees of severity. This problem requires immediate medical attention and treatment as it can lead to serious consequences for the child's health and development. Here are some of the causes and factors that can cause cerebral hypoxia in children:
- Perinatal asphyxia: This is a condition where a baby does not get enough oxygen at birth or during the first few minutes of life. Causes may include problems with the placenta, cord compression, or difficulty breathing for the baby after birth.
- Congenital heart defects: Some children may have congenital heart abnormalities that can lead to a lack of oxygen in the blood and therefore hypoxia of the brain.
- Respiratory infections: Diseases such as viral or bacterial infections of the respiratory tract can cause breathing difficulties and hypoxia.
- Injury: Injuries such as concussions or strangulation can lead to lack of oxygen and brain damage.
- Sudden Infant Death Syndrome (SIDS): This is a tragic condition in which a baby dies suddenly in his or her sleep, often due to breathing problems and lack of oxygen.
- Anesthesia and surgical procedures: In rare cases, hypoxia can result from impaired oxygen metabolism during anesthesia or surgical procedures.
Treatment of cerebral hypoxia in children will depend on its cause and severity. It usually involves restoring normal oxygen metabolism, maintaining vital functions and rehabilitation.
Cerebral hypoxia in newborns
It is a serious condition where the baby's brain does not get enough oxygen, which can cause various complications and damage to the brain tissue. Neonatal cerebral hypoxia can occur due to various reasons such as complications during pregnancy, during the birthing process or in the period after birth.
Major factors that may contribute to the development of cerebral hypoxia in newborns include:
- Asphyxiation during labor: The birthing process may result in cord compression or other factors that can temporarily cut off oxygen to the baby.
- Premature birth: Premature babies have a more immature respiratory system and may be more susceptible to hypoxia.
- Maternal infections: Infections such as viral or bacterial infections in pregnant women may increase the risk of hypoxia in the newborn.
- Placental insufficiency: Problems with the placenta, which can reduce the flow of oxygen and nutrients to the fetus, can lead to hypoxia.
- Abnormalities of the umbilical cord: Abnormalities in the structure of the umbilical cord can cause a disruption in the oxygen supply to the baby.
- Maternal diabetes mellitus: Pregnant women with uncontrolled diabetes mellitus may be at risk of hypoxia in the baby.
Neonatal cerebral hypoxia can range in severity from mild to severe. The effects of hypoxia can also vary and include:
- Hypoxic-ischemic encephalopathy (HIE): This is a condition that manifests as damage to brain tissue and can have varying degrees of severity. It can lead to delayed psychomotor development, motor impairment and mental retardation.
- Epilepsy: Hypoxia may increase the risk of epilepsy in newborns.
- Developmental Delay: Hypoxia can affect brain development and lead to developmental delays in children.
- Other neurological findings: In some cases, hypoxia can cause different neurological symptoms such as sleep disturbances, specific motor problems, and others.
Treatment and prognosis depend on the severity and duration of hypoxia, as well as the timing of treatment. It is important to seek medical attention in a timely manner and provide the necessary treatment and rehabilitation to minimize the effects of neonatal hypoxia. Generally, milder cases of hypoxia have a more favorable prognosis than more severe cases with long-term consequences.
Stages
Brain hypoxia can have different stages depending on the duration and severity of the oxygen deficiency. The following stages are generally accepted:
- Acute hypoxia: This initial stage is characterized by inadequate oxygen supply to the brain for a short period of time, usually a few minutes. Neurologic symptoms such as dizziness, tingling in the extremities, difficulty breathing, etc. May occur during this stage. If oxygen supply is quickly restored, the brain may recover without significant damage.
- Sub-acute hypoxia: This stage is characterized by a longer period of oxygen deprivation that can last from a few minutes to hours. More serious symptoms such as seizures, unconsciousness, and impaired brain function can occur in this stage. The longer the oxygen deprivation lasts, the greater the likelihood of brain damage.
- Chronic hypoxia: This stage is characterized by a prolonged and persistent lack of oxygen. It may be due to chronic lung disease, heart disease, or other factors that lead to a permanent impairment of oxygen metabolism. Chronic brain dysfunction and dementia may develop in this stage.
- Ischemic Stroke: Hypoxia of the brain can lead to stroke when blood vessels supplying blood to a specific area of the brain become blocked or clogged, resulting in tissue necrosis.
Understanding the stages of cerebral hypoxia is important in determining proper treatment and prognosis. The sooner medical intervention and restoration of normal oxygen exchange is provided, the better the chances of preventing serious brain damage.
Complications and consequences
Brain hypoxia, especially if not detected and treated in a timely manner, can lead to serious complications and long-term consequences. The effects of hypoxia can depend on the severity and duration of the lack of oxygen, as well as the age and general condition of the patient. Some of the possible complications and effects of cerebral hypoxia include:
- Neurological deficits: Hypoxia can lead to impaired brain function, which can manifest as a variety of neurological symptoms such as impaired motor coordination, seizures, insomnia, headaches, loss of consciousness, and paralysis.
- Brain cell die-off: With prolonged and severe hypoxia, brain cell die-off can occur, which can leave lasting and permanent brain damage.
- Long-term sequelae syndrome: Long-term effects can develop after hypoxia, such as hypoxia long-term effects syndrome (HIE), which can include developmental disorders, psychomotor developmental delays, and mental retardation.
- Epilepsy: Hypoxia may increase the risk of epilepsy, which can lead to seizures.
- Cognitive impairment: The effects of hypoxia may include impairment of cognitive functions such as memory, attention, and learning ability.
- Emotional and psychological disturbances: Hypoxia can cause emotional and psychological problems such as depression, anxiety, and personality changes.
- Paralysis: In some cases, hypoxia can lead to paralysis or loss of control over certain parts of the body.
- Death: In cases of severe and prolonged hypoxia, death can be one of the most serious consequences.
Cerebral hypoxia may be associated with clinical death, sometimes called "clinical death due to respiratory and cardiac arrest" or "clinical death due to asphyxia". Clinical death is a state in which the heart stops beating and respiratory functions cease. In this condition, there is no blood flow and the brain does not receive enough oxygen and nutrients to maintain viability.
However, it is important to note that clinical death does not always mean irreversible death. In some cases, if resuscitation is started immediately, circulation is restored, and breathing and cardiac activity are maintained, an attempt can be made to bring the patient back to life. This process is called "clinical recovery" and can be successful if started as soon as possible and with the right medical care.
Clinical recovery requires professional skills and medical equipment such as defibrillators and trained medical personnel. The likelihood of successful recovery depends on many factors, including the duration of the absence of circulation, the cause of clinical death, and the patient's general condition.
It is therefore important that in the event of clinical death, adequate resuscitation and care is immediately available in medical facilities. The sooner resuscitation is started, the better the chances of successful recovery and reduction of possible brain damage due to hypoxia.
Diagnostics of the cerebral hypoxia
Diagnosing cerebral hypoxia may involve various medical tests and procedures to assess the oxygen levels in the brain and determine the cause of the problem. The following are the main methods of diagnosis:
- Computed tomography (CT) scan of the brain: CT scans can be used to detect structural changes in the brain and assess vascular health. However, it is not always able to detect hypoxia.
- Magnetic resonance imaging of the brain (MRI): MRI can provide more detailed images of brain structures and blood vessels, which can help identify hypoxia.
- Electroencephalography (EEG): EEG measures the electrical activity of the brain and can help identify abnormalities associated with hypoxia.
- Oximetry: This test uses a special device (oximeter) to measure the level of oxygen in the blood. The results can be used to assess whether hypoxia is present.
- Blood gas analysis: Measuring oxygen and carbon dioxide levels in arterial blood can help determine if there is hypoxia and assess its severity.
- Other laboratory tests: Laboratory tests may be performed to determine the cause of hypoxia, such as blood tests, electrolytes, and other biochemical parameters.
- Functional tests: Some functional tests, such as a physical activity test or cardiac tests, may be performed to assess how the body responds to exercise and oxygen supply to the brain.
Ultrasound (ultrasound) of the brain can be used to diagnose a variety of conditions, including cerebral hypoxia. Cerebral hypoxia refers to insufficient oxygen supply to the brain, which can lead to serious consequences.
Brain ultrasound can help detect the following changes associated with hypoxia:
- An increase in the size of the ventricles of the brain (hydrocephalus): Hypoxia can cause fluid to build up in the ventricles of the brain, causing them to enlarge.
- Changes in brain structure: Ultrasound can help detect changes in brain structure, such as decreased brain mass or developmental abnormalities.
- Assessment of blood supply: Ultrasound can be used to assess the blood supply to the brain, which can be useful in determining the degree of hypoxia.
However, it should be noted that brain ultrasound may be a limited investigation and more specialized techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) may be required to more accurately diagnose cerebral hypoxia.
The diagnosis and treatment of cerebral hypoxia requires medical expertise and extensive research based on clinical symptoms and additional medical evidence. If you or your child suspects cerebral hypoxia, be sure to consult your doctor to get the diagnosis and treatment you need.
Diagnosis usually involves a combination of these methods, and it aims to identify the cause and extent of hypoxia, which will help determine appropriate treatment and management of the patient's condition.
Differential diagnosis
Differential diagnosis of cerebral hypoxia involves identifying and distinguishing this condition from other medical problems that may have similar symptoms. It is important to consider clinical findings, the patient's medical history, and the results of examinations and laboratory tests. Below are some conditions and diseases to consider in the differential diagnosis of cerebral hypoxia:
- Epilepsy: Epileptic seizures may have similar symptoms to some forms of hypoxia, such as seizures and loss of consciousness.
- Stroke: Stroke can cause similar symptoms such as motor impairment, speech disorders and loss of consciousness and often requires urgent differential diagnosis and treatment.
- Heart problems: Heart disease, such as heart failure or arrhythmias, can lead to symptoms related to lack of oxygen, such as fatigue and shortness of breath.
- Metabolic disorders: Some metabolic disorders, such as hypoglycemia (decreased blood sugar levels) or hyponatremia (decreased blood sodium levels), can cause symptoms similar to hypoxia.
- Traumatic head injuries: Head injuries can interfere with the oxygen supply to the brain and cause symptoms similar to hypoxia.
- Mixed cerebral circulation disorder syndrome: This is a condition in which the brain can face both a lack of oxygen and insufficient blood supply at the same time, which can lead to difficult-to-diagnose symptoms.
- Poisoning: Poisoning from gases such as carbon monoxide (carbon monoxide) or other poisonous substances can cause symptoms that resemble hypoxia.
- Chronic lung disease: People with chronic obstructive lung disease, such as COPD, may experience chronic oxygen deprivation, which can simulate symptoms of hypoxia.
Treatment of the cerebral hypoxia
Treatment of cerebral hypoxia depends on the cause and severity of the condition. Hypoxia can result from a variety of medical conditions such as breathing disorders, cardiovascular disease, poisoning, trauma, and others. Here are some general principles of treatment:
- Ensuring normal oxygenation: The first priority is to ensure that the patient has adequate oxygen. This may include the use of an oxygen mask, intubation and artificial ventilation in severe cases.
- Treatment of the underlying condition: It is important to identify and treat the underlying cause of hypoxia, whether it is treating an infection, removing mechanical airway obstruction, stabilizing blood pressure, or treating other medical conditions.
- Blood pressure maintenance: In cases of hypoxia associated with inadequate blood supply to the brain, it may be necessary to maintain blood pressure with medications and infusions.
- Rehabilitation: Once the patient is stabilized, physical, speech and visual rehabilitation may be required, especially if hypoxia has caused damage to brain tissue.
- Symptom control: Treatment may also include symptomatic therapy to reduce pain, dizziness, nausea, and other symptoms.
- Maintaining an optimal environment: It is important to provide the patient with a suitable environment, including temperature, noise and lighting.
- Organ function control: Hypoxia can cause problems with the function of organs such as the kidneys and liver. Monitoring and maintaining the function of these organs is also important.
Treatment should take place in a hospital under medical supervision and management. The patient may require intensive care depending on the severity of the condition. For each case, treatment should be individualized and determined by the physician based on the specific circumstances.
Drug treatment
Treatment of cerebral hypoxia involves different approaches, and the use of specific medications depends on the cause, severity and phase of hypoxia. Doctors who specialize in treating such conditions prescribe and administer treatment. The following are some of the possible drugs and approaches that can be used in the treatment of cerebral hypoxia:
- Oxygen therapy: The main treatment for cerebral hypoxia is the administration of supplemental oxygen. This can be done using an oxygen mask, continuous breathing pump or inhaler.
- Medications to improve circulation: In some cases, medications are used to help improve blood flow to the brain. This may include anticoagulants (such as heparin), antiaggregants (such as aspirin), or drugs to improve microcirculation.
- Anticonvulsants: If a patient has seizures as a result of cerebral hypoxia, the doctor may prescribe anticonvulsants such as diazepam or phenytoin.
- Corticosteroids: In some cases, corticosteroids may be used to reduce inflammation and swelling of the brain.
- Hypothermia: In some newborns with perinatal asphyxia, the hypothermia technique, in which body temperature is lowered to reduce brain damage, may be used.
- Other medications: Depending on the specific symptoms and circumstances, doctors may prescribe other medications to manage symptoms and support the body's organs and systems.
Forecast
The prognosis of cerebral hypoxia depends on many factors, including the severity and duration of hypoxia, the patient's age, the speed of treatment initiation, and the effectiveness of medical interventions. It is important to note that cerebral hypoxia can have a wide range of clinical manifestations, and each case is unique.
General trends in the prognosis of cerebral hypoxia include the following:
- Degree of damage: The more severe and prolonged the hypoxia, the greater the likelihood of adverse effects. In cases of mild and short-term hypoxia, there may be a full recovery without complications. However, if hypoxia is prolonged and severe, permanent and irreversible brain damage may occur.
- Age: Children and infants may be more likely to recover and compensate for losses after hypoxia compared to adults.
- Speed of treatment: Getting medical attention quickly and starting treatment as soon as hypoxia occurs can greatly increase the chances of improvement.
- Effectiveness of treatment: The effectiveness of medical therapy and rehabilitation also has an impact on prognosis. This aspect includes early rehabilitation, physical and speech therapy, and medication, if necessary.
- Comorbidities: The presence of other diseases or conditions may complicate the prognosis and treatment of hypoxia.
- Individual variability: The prognosis can vary greatly from patient to patient, even under similar hypoxic conditions. This is due to genetic factors and individual body characteristics.

