Medical expert of the article
New publications
Causes and pathogenesis of hypothyroidism
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
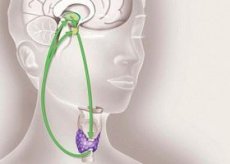
In the vast majority of cases (90-95%), hypothyroidism is caused by a pathological process in the thyroid gland itself, which reduces the level of hormone production (primary hypothyroidism). Disruption of the regulatory and stimulating effect of pituitary thyrotropin or hypothalamic releasing factor (thyroliberin) leads to secondary hypothyroidism, which is significantly less common than primary hypothyroidism. The issue of peripheral hypothyroidism, which occurs either due to disruption of thyroid hormone metabolism in the periphery, in particular the formation of inactive, reverse T3 from T4, or as a result of decreased sensitivity ofnuclear receptors of organs and tissues to thyroid hormones, remains controversial. The issue of age-related degradation of the level of active thyroid hormones as a result of disrupted peripheral metabolism and of changes in the thyroid gland itself during aging remains controversial. When screening populations over 60 years of age, in some studies overt hypothyroidism was detected in 3.4%, preclinical hypothyroidism in 5.2% of subjects, while in others the detection rate was significantly lower.
Evaluation of thyroid function and its role in various clinical syndromes and diseases can be complicated by changes in the peripheral metabolism of thyroid hormones, leading to a decrease in T3 levels in a number of diseases and conditions, for example, in nephrotic syndrome, in liver cirrhosis, and sometimes during pregnancy.
Obviously, the importance of peripheral thyroid hormone insensitivity syndrome in the genesis of hypothyroidism is underestimated in real clinical practice.
Currently, primary hypothyroidism, which occurs on the basis of chronic autoimmune thyroiditis, is the most common among adults. In this regard, the idea of so-called idiopathic hypothyroidism as the main variant of spontaneous thyroid insufficiency has been significantly transformed. In chronic thyroiditis, the thyroid tissue, having passed the stage of lymphoid infiltration, gradually atrophies and is replaced by fibrous tissue. The gland may decrease in size, and not change significantly, and hypertrophy due to compensatory hyperstimulation of TSH (Hashimoto's goiter).
Primary hypothyroidism in various combinations with damage to the adrenal glands, gonads, parathyroid and pancreas, and in young people and in children with fungal skin diseases, alopecia and vitiligo is known as primary polyendocrine deficiency syndrome, the autoimmune nature of which is indisputable. At the same time, along with damage to the endocrine system, patients may have other immune diseases (bronchial asthma, pernicious anemia, atrophic gastritis). Primary hypothyroidism occurs for a number of reasons.
- Complications of treatment after:
- surgical treatment of various thyroid diseases;
- treatment of toxic goiter with radioactive iodine;
- radiation therapy for malignant diseases of organs located in the neck (lymphoma, laryngeal carcinoma);
- poorly controlled treatment with thyrotoxic agents (mercazolil, lithium);
- the use of iodine-containing drugs, including radiographic contrast agents;
- taking glucocorticoids, estrogens, androgens, sulfonamide drugs.
- Destructive lesions of the thyroid gland: tumors, acute and chronic infections (thyroiditis, abscess, tuberculosis, actinomycosis and, very rarely, amyloidosis, sarcoidosis, cystinosis).
- Dysgenesis (aplasia or hypoplasia) of the thyroid gland due to defects in intrauterine development, usually in newborns and children aged 1-2 years, often combined with deafness and cretinism. Sometimes the remainder of the thyroid tissue is located in the sublingual-thyroid region and at the root of the tongue. Thyroid malformation can be caused by iodine deficiency in the environment, untreated maternal hypothyroidism, or hereditary predisposition.
Secondary hypothyroidism develops with inflammatory, destructive or traumatic lesions of the pituitary gland and/or hypothalamus (tumor, hemorrhage, necrosis, surgical and radiation hypophysectomy) with insufficient secretion of TRH and TSH and subsequent decrease in the functional activity of the thyroid gland. Isolated disorder of TSH synthesis is observed very rarely. More often, secondary hypothyroidism occurs within the framework of general pituitary pathology (mainly the anterior lobe) and is combined with hypogonadism, hypocorticism, excess of somatotropic hormone.
Pathogenesis of hypothyroidism
The pathogenesis (especially primary) of hypothyroidism is determined by a decrease in the level of thyroid hormones, which have a spectrum of influence on physiological functions and metabolic processes in the body. As a result, all types of metabolism are suppressed, oxygen utilization by tissues is inhibited, oxidative reactions are slowed down, and the activity of various enzyme systems, gas exchange and basal metabolism are reduced. Slowing down the synthesis and catabolism of protein and protein fractions, as well as the process of their elimination from the body leads to a significant increase in protein breakdown products in the extravascular spaces of organs and tissues, in the skin, in skeletal and smooth muscles. In particular, creatine phosphate accumulates in the myocardium and other muscle groups. At the same time, the content of nucleic acids (DNA, RNA) decreases, the protein spectrum of the blood changes towards an increase in globulin fractions, and a significant amount of albumin is concentrated in the interstitium, the structure of hemoglobin changes. The pathogenesis of increased membrane and transcapillary permeability for protein, characteristic of hypothyroidism, is largely unexplored. The possible involvement of vasoactive substances (for example, histamine) is assumed; a more probable connection is with a slowdown in lymphatic drainage, which reduces the return of protein to the vascular bed.
In the heart, lungs, kidneys, serous cavities and, above all, in all layers of the skin, acidic glycosaminoglycans (GAGs), primarily glucuronic acid and, to a lesser extent, chondroitin sulfuric acid, are excessively deposited. The level of glycosaminoglycans in blood fibroblasts, which are under the direct influence of thyroid hormones, rarely increases. In studies conducted by the authors together with A. N. Nazarov, it was shown that the level of glycosaminoglycans increases with the duration of the disease.
Excess glycosaminoglycans change the colloidal structure of connective tissue, increase its hydrophilicity and bind sodium, which, under conditions of difficult lymph drainage, forms myxedema.
The mechanism of sodium and water retention in tissues can also be affected by excess vasopressin, the production of which is inhibited by thyroid hormones, as well as a decrease in the level of atrial natriuretic factor. Along with the tendency to increase the level of intracellular and interstitial sodium, there is a tendency to hyponatremia and a decrease in the degree of concentration of intracellular potassium. The saturation of tissues with free calcium ions also decreases. The utilization and removal of lipolysis products slows down, the level of cholesterol, triglycerides, and beta-lipoproteins increases.
Thyroid hormone deficiency inhibits brain tissue development and suppresses higher nervous activity, which is especially noticeable in childhood. However, hypothyroid encephalopathy also develops in adults, which is characterized by decreased mental activity and intelligence, weakening of conditioned and unconditioned reflex activity. The physiological activity of other endocrine glands is limited, primarily the adrenal cortex, which rapidly reduces its function under hypothermia. Peripheral metabolism of corticosteroids and sex hormones is also impaired (the latter leads to anovulation). However, the level of catecholamines increases compensatorily, but in the absence of thyroid hormones, their physiological effects are not realized due to decreased sensitivity of beta-adrenergic receptors. A decrease in the level of thyroid hormones in the blood by the mechanism of negative feedback increases the secretion of thyroid-stimulating hormone and often prolactin. TSH stimulates compensatory hyperplasia of thyroid tissue, the formation of cysts, adenomas, etc.
Hypothyroid coma is based on depression of the respiratory center and progressive decrease in cardiac output, increasing hypoxia of the brain and hypothermia as a result of general hypometabolism as a result of a decrease in the rate of basic metabolic reactions and oxygen utilization. Along with depression of the respiratory center, pulmonary ventilation is hampered by the accumulation of bronchial secretions and a decrease in the cough reflex. The most important link in pathogenesis, determining the severity and prognosis, is hypocorticism. Loss of consciousness is usually preceded by a pre-comatose period, when the main symptoms of hypothyroidism are concentrated and aggravated. Under conditions of severe hypothermia (30 °C and even lower), the functions of all internal organs, primarily the adrenal glands, are reduced. However, body temperature in hypothyroid coma can rarely be normal. Diagnosis and differential diagnosis may be difficult in the absence of a history of hypothyroidism or radioactive iodine therapy. It is this type of therapy that leads to late hypothyroidism, the main symptoms of which stimulate age-related involution.
Pathological anatomy
The cause of decreased thyroid function is most often its atrophic changes, expressed to varying degrees. In severe atrophy, the gland weighs no more than 3-6 g and is represented by a thickened capsule with well-developed connective tissue layers and vessels, between which there are a few islets of thyroid tissue from small follicles with thick colloid and flat follicular cells or Hürthle-Ashkenazi cells. In the stroma there are a few lymphoid infiltrates with an admixture of macrophages and other cells. Sometimes pronounced fatty infiltration is noted. Such changes usually occur in hypothyroidism caused by a violation of the thyrotropic function of the hypothalamus and / or pituitary gland.
If congenital hypothyroidism is caused genetically and is accompanied by the inability of the thyroid gland to produce hormones, goiter formation is observed. The gland increases in size due to hyperplasia and hypertrophy of the thyroid epithelium, forming strands, solid clusters, tubular and, rarely, follicular structures with virtually no content. The thyroid epithelium is large, often with light vacuolated cytoplasm. The nuclei are especially hypertrophied. They can be giant and ugly. Such epithelium proliferates intensively, which leads to rapid goiter growth. Subtotal thyroid resection performed on these patients often turns out to be non-radical. Goiter quickly recurs. Solidification and dysplastic changes in the thyroid epithelium become even more pronounced. Often these cases are interpreted as thyroid cancer. However, the absence of angioinvasion and capsule growth phenomena of the gland does not allow us to consider this pathology as malignant neoplasms. Relapses and increased proliferation of the thyroid epithelium in these cases are caused by hyperstimulation of their TSH. Numerous adenomas of various structures, especially of the embryonic type, are often formed in such glands.
In skeletal muscles, hypothyroidism is characterized by hypertrophy of some muscle fibers with the disappearance of transverse striations, rupture of myofibrils, disruption of the integrity of the sarcolemma, edema of individual fibers, and an increase in the number of nuclei with their redistribution along the fiber. Sometimes, lymphoplasmacytic infiltration is observed, as in polymyositis. All these changes are characteristic of myxedema and are considered myxedematous myopathy.
In the heart of patients with myxedema, pericardial edema is often found, and in the coronary arteries - multiple atheromas. The basement membrane of the myocardial capillaries is usually sharply thickened.
The pituitary gland is often enlarged, and various changes can be detected in it: a sharp decrease in the granulation of acidophils, an increase in the number of weakly granulated basophils.
The adrenal cortex is atrophied. Autoimmune hypothyroidism can be combined with autoimmune damage to the adrenal cortex (Schmidt syndrome).
Hypothyroid polyneuropathy is caused primarily by neuroaxonal degeneration, which in turn aggravates myxedema myopathy.
Hypothyroidism may accompany various types of nodular goiter, mainly colloid, as well as generalized or isolated amyloidosis of the thyroid gland, in which atrophy of its parenchyma occurs due to massive deposition of amyloid in the basement membrane of the follicles and in the stroma of the gland.


 [
[