Medical expert of the article
New publications
Osteochondropathies of the bones
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Osteochondropathies are a group of diseases of the bone and joint system. They are characterized by aseptic subchondral infarction of the marginal area of spongy bone tissue in areas with increased load.
The main types of degenerative-dystrophic processes in bones:
- The epiphyseal ends of the tubular bones are the head of the femur, the head of the second and third metatarsal bones, and the sternal end of the clavicle.
- Spongy bones - patella, navicular bone of the foot and hand, lunate bone of the hand, body of the vertebrae, sesamoid bone of the first metatarsophalangeal joint.
- Apophyses of bones - tibial tuberosity, calcaneal tuberosity, vertebral apophyses, pubic bone.
- Partial damage to the articular surfaces - the head of the femur, the distal end of the femur, the elbow and ankle joints, the head of the humerus, radius, ulna.
Aseptic bone necrosis can be primary and secondary:
- Primary – develops in childhood, associated with the action of vascular, age and endocrine factors. The rapid rate of skeletal growth in children and constitutional features of the skeletal system have a significant impact on the development of the disease.
- Secondary (symptomatic) – is a complication of the underlying disease. Develops against the background of bone tissue ischemia, vasculitis, degenerative and metabolic disorders, neurotrophic and endocrine disorders and other pathological processes.
In most cases, the disease has a monoarticular character of the lesion. Most often, it is localized in the head of the femur, the navicular bone of the foot, and the metatarsal bones. Rarely, multiple lesions of the epiphyses of the phalanges of the upper limbs, bilateral lesions of the tuberosity of the tibia and the tuberosity of the calcaneus are found.
Osteochondropathies of bones are characterized by pronounced pain sensations at the site of the lesion, which increase with load and decrease at rest. Local painful swelling is observed due to reactive synovitis, which occurs when the affected part of the bone is injured. A slight deterioration in general well-being is also possible.
The pathological process is characterized by a long course with gradual disappearance of clinical and diagnostic signs. A set of laboratory and instrumental studies is used to establish a diagnosis. Treatment consists of a course of drug therapy, physiotherapy, and limited physical activity. In particularly severe cases, surgery is performed.
Osteochondropathy of the foot
The degenerative-dystrophic process in the bones of the foot is associated with necrosis of the spongy bone, which is subject to the greatest mechanical load. The disease is also characterized by damage to the apophyses of tubular bones. It is most often diagnosed in children and adolescents; adults get sick extremely rarely.
In most cases, the pathology has a benign course, not affecting the functioning of the joints. Self-healing is typical for the disease. In this case, the presence of aseptic necrosis can only be judged by X-rays and the presence of deforming arthrosis.
The mechanism of the disease is not fully understood. Most often, it is associated with local vascular disorders that arise due to the action of various factors: trauma, infection, congenital and metabolic disorders.
Osteochondropathy of the foot has several forms:
- Scaphoid bone lesion (Kohler's disease I) - most often develops in boys aged 3-10 years. Both unilateral and bilateral processes are possible. Scaphoid bone necrosis in adults is Müller-Weiss syndrome.
- Aseptic necrosis of the metatarsal heads (Kohler disease II) - this form of the disease occurs in less than 1% of cases of foot damage. Most often diagnosed in female patients aged 10-20 years. With multiple necrosis, static deformation of the foot is observed: flat-valgus and valgus deformity, transverse and longitudinal flatfoot, dysplastic development.
- Destruction of the sesamoid bone of the first metatarsophalangeal joint (Renander-Muller disease) - occurs in women aged 15-30, manifested by acute pain under the head of the first metatarsal bone, which intensifies when straightening the finger and while walking. Radiographic signs indicate a change in the structure of the affected bone, its fragmentation.
- Tuberosity lesion of the 5th metatarsal bone – develops due to ossification disorder, from additional ossification points. X-ray shows an ununited tuberosity fracture, persistent apophysis or additional Vesalius bone. The disease is diagnosed in childhood with increased load on the foot. Patients have a limping gait with increased load on the inner part of the foot.
- Dissecting osteochondrosis of the talus - most often occurs due to trauma to the ankle joint. The pathological process occurs in the area of the talus block and is manifested by aseptic inflammation. On the X-ray, there is a focus of destruction with scalloped contours, delimited from healthy tissue by a zone of sclerosis.
- Aseptic necrosis of the calcaneal tuberosity (Gaglund-Schinz disease) - pain during load and palpation of the calcaneus occurs in patients aged 7-14 years. The disorder manifests itself as periostitis or bursitis, atrophy of the calf muscles is possible. X-ray shows damage to the apophysis of the calcaneus, loosening of the cortex under the apophysis.
All of the above osteochondropathy go through several stages of development. Treatment depends on the stage of the disease, the presence of complications and the characteristics of the patient's body. Most often, conservative therapy is carried out, but in particularly severe cases, surgical intervention is possible.
Osteochondropathy of the calcaneus
This form of degenerative-necrotic disease is more often diagnosed in children than in adults. The risk group includes girls aged 7-9 and boys aged 9-11. Osteochondropathy of the calcaneus is typical for professional athletes and people who regularly experience increased physical activity.
Schinz disease, or aseptic necrosis of the calcaneus, develops due to a disruption in the nutrition of bone tissue. The main causes of the disorder include:
- Endocrine and metabolic disorders.
- Poor absorption of calcium.
- Injuries and increased physical activity.
The symptoms of the disease depend on its stage and the presence of complications. In some, it proceeds sluggishly over a long period of time, while in others it causes acute pain. The disruption of bone tissue nutrition is manifested by swelling in the affected area, problems with flexion and extension of the foot, pain when trying to palpate. It is also possible to have an increase in local body temperature, limping when walking, pain in the place where the Achilles tendon attaches to the heel bone.
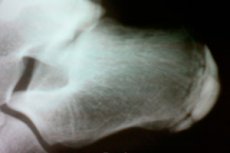
Diagnostics include radiography, CT, and MRI. The radiograph shows abnormalities in the structural patterns of the apophysis and fragmentation, distorted distances between the heel bone and the apophysis. In the diseased leg, the unevenness of the contours is more pronounced than in the healthy one. Differential diagnostics are mandatory. The pathology is compared with changes in the bones that are similar in symptomatology.
Treatment consists of a course of drug therapy. Patients are prescribed chondroprotectors and calcium preparations, analgesics. Physiotherapy procedures are indicated to relieve pain and stimulate regenerative processes. It is also necessary to minimize the load on the affected limb and choose the right shoes.
Osteochondropathy of the calcaneal tuberosity
Destruction and slow restoration of the spongy bone tissue of the calcaneal tuberosity occurs predominantly in female patients aged 12-15 years. The disease can have either a unilateral or bilateral lesion.
Causes of the degenerative process in bones:
- Microtraumas.
- Increased physical activity.
- Endocrine, vascular and neutrophic factors.
The main symptoms include: severe pain when walking, swelling of the affected tissues, altered structure and muscle atrophy. Diagnostics consists of a complex of laboratory and instrumental methods. Differentiation with bone tuberculosis, malignant tumors, bursitis, periostitis, osteomyelitis, inflammatory lesions is also carried out.
Treatment begins with conservative methods. Immobilization of the affected limb, pain relief, physiotherapy, and taking multivitamin complexes are indicated. If the above methods do not bring the desired therapeutic result, then surgical intervention is indicated. Particular attention is paid to preventive measures aimed at preventing relapses of the disease.
Osteochondropathy of the metatarsal bones
Metatarsal bones are five tubular short bones that are part of the foot. They are subject to degenerative-dystrophic processes. Alban-Kohler II disease or aseptic necrosis of the metatarsal bones is more common in young women. The main cause of the development of pathology is frequent and prolonged wearing of high-heeled shoes.
The painful condition gradually progresses, causing acute pain when walking. Changing shoes and reducing the load on the feet alleviates the discomfort, but bone necrosis continues, developing into deforming arthrosis. X-rays reveal a compacted metatarsal head and its fragmentation.
Treatment is conservative in most cases. Patients are shown to reduce the load on the leg, undergo physiotherapy procedures, and wear insoles. In particularly severe cases, resection of the metatarsal bone is performed to remove extensive bone growths.
Osteochondropathy of the metatarsal head
Aseptic lesion of the metatarsal head is most often diagnosed in female patients aged 12-18 years. In 10% of cases, necrosis affects several metatarsal bones, less often bilateral lesions occur.
The main cause of the disease is a violation of bone nutrition. This occurs due to injuries, wearing tight or ill-fitting shoes, overloading the lower limbs, flat feet (static transverse, longitudinal). Tissue destruction occurs gradually, so the symptoms appear incrementally. Signs of the disorder include:
- Painful sensations when putting weight on the foot.
- Lameness.
- Inability to walk barefoot, in soft shoes and on uneven ground.
- On the dorsum of the foot at the level of the lesion there is a small swelling extending proximally along the metatarsal bone.
- Palpation of the head is painful.
- Shortening of the finger adjacent to the head.
- Deformation of the metatarsophalangeal joint and limitation of movement in it.
X-ray, computed tomography, and magnetic resonance imaging are used for diagnostics. Laboratory tests and differential methods are also indicated.
Radiological signs of the disease:
- The first stage is manifested by a slight compaction of the structure of the bone tissue of the affected area.
- At the second stage, there is a thickening of the articular surface of the head of the metatarsal bone and an increase in the density of its bone tissue.
- The third stage is characterized by fragmentation, that is, the resorption of necrotic bone tissue.
- The fourth stage is the restoration of the structure of the deformed bone and the disappearance of signs of fragmentation.
When differentiating, the disease is compared with complications of a fracture of the head of the metatarsal bone, inflammatory processes, and Deichlander's disease (march fracture).
At the first and second stages, immobilization of the affected limb is indicated. At later stages, it is necessary to wear an orthopedic insole with the layout of the transverse and longitudinal arches of the foot. It is also necessary to completely exclude any overload of the foot. Physiotherapy procedures are carried out to reduce painful sensations and stimulate regenerative processes.
If conservative therapy does not give the expected results, then surgery is performed. Surgical intervention is aimed at removing bone growths that increase pain and interfere with normal shoe wearing. Restoring joint mobility is also possible. The prognosis is favorable in most cases. Advanced forms of the disease develop into deforming arthrosis with dysfunction of the forefoot.
Osteochondropathy of the scaphoid bone
Köhler I disease is rarely diagnosed and usually after injuries. Boys aged 3-10 years and older often encounter this pathology. Both unilateral and bilateral aseptic necrosis of the scaphoid bone is possible. If the disorder is detected in adults, it refers to an independent nosological form of osteochondropathy and is called Müller-Weiss syndrome.
In children, the disease occurs when the ossification process of the navicular bone is disrupted. On an X-ray, this is manifested by the following signs:
- Increased density of the affected bone.
- Flattening of the ossification nucleus.
- Fragmentation of the scaphoid bone in the sagittal direction.
- Enlargement of the interosseous space.
On the back of the foot at its inner edge, swelling and pain appear. Because of this, the patient limps, stepping with the affected limb. The disease can occur against the background of flat feet, deformation of the foot and toes. When differentiating, the possibility of a fracture, an inflammatory process, an isolated tuberculous lesion is taken into account.
Treatment is conservative. It is necessary to immobilize the affected limb with a plaster cast. Physiotherapeutic procedures are mandatory, which improve the blood supply to the affected tissues, relieve pain and promote recovery. Surgical intervention is not performed. The duration of complete restoration of the bone structure takes 1.5-2 years.
Osteochondropathy of the talus
The talus or calcaneal bone is one of the bones that forms the lower part of the ankle. It is 60% covered with articular cartilage and is responsible for transferring body weight to the surface of the foot. The bone consists of several parts: block, head, posterior process.
Aseptic necrosis of this localization is rare, threatens with limited mobility, disability. Men face this problem more often than women. The main age group of patients is 20-45 years.
Causes of degenerative-dystrophic processes:
- Complications of fracture.
- Circulatory disorders.
- Ankle injuries.
- Increased physical activity.
The disease is characterized by a slow progression. Necrosis goes through several stages. The main symptoms include local swelling and painful sensations when walking.
In the diagnostic process, X-ray, CT, MRI, and a set of laboratory tests are used. The X-ray clearly shows a lesion with a cellular structure, delimited by a zone of sclerosis from the healthy bone. Also, a protrusion and thinning of the endplate over the lesion is observed. In this case, both one- and two-sided processes are possible.
Treatment is conservative in most cases. Patients are prescribed medications and physiotherapy to improve blood circulation, restore bone cell density and stimulate regenerative processes. If medical help is sought in a timely manner, the prognosis is favorable.
Osteochondropathy of the hip joint
Legg-Calve-Perthes disease accounts for about 2% of all orthopedic pathologies. It is most often diagnosed at the age of 4-14 years. At the same time, male patients are more often ill than females. The pathological process can be bilateral, but unilateral localization of necrosis is more common.
Causes of hip joint damage:
- Myelodysplasia of the lumbar spinal cord.
- Inflammation of the hip joint.
- Injuries with compression of blood vessels and disruption of blood supply.
- Infectious diseases.
The early stages of the degenerative process are asymptomatic. As they progress, pain in the hip and knee joints and lameness appear. Later, deformation of the femoral head and limitation of movement in the diseased joint occur. The deformation depends on the size of the lesion and determines the outcome of the pathology.
MRI, ultrasound of the hip joints and X-ray are used for diagnostics. Treatment is aimed at restoring the anatomical structure of the bone to prevent gait disorders and eliminate pain. Patients are prescribed medications, physiotherapy, and therapeutic exercises. Surgical treatment is indicated for severe forms of the disease. The operation is aimed at improving the blood supply to the hip and eliminating disorders in the joint. The duration of treatment is from 3 to 4 years.
Osteochondropathy of the femur
Perthes disease is a pathological condition in which the blood supply to the femoral head is disrupted, with subsequent aseptic necrosis. It occurs in childhood and adolescence from 3 to 14 years old, and is one of the most common osteochondropathy. Boys are more often affected than girls, but in the latter, the disease proceeds with severe complications.
Causes and factors of bone tissue nutrition disorders:
- Metabolic disorders.
- Impact of external factors.
- Injuries and damages.
- Myelodysplasia.
- Inflammatory and infectious diseases.
- Hormonal changes in adolescence.
- Disruption of metabolism involved in the formation of bone tissue.
- Genetic predisposition.
- Anomalies of the structure of the hip joint.
Aseptic necrosis of the femur goes through five main stages of development:
- Disruption of blood supply and formation of a necrotic focus.
- Impression fracture in the destroyed area.
- Resorption of necrotic tissue, shortening of the femoral neck.
- Proliferation of connective tissue in the lesion.
- Replacement of connective tissue with new bone, fracture healing.
In the early stages, there is slight pain when walking, localized in the hip joint. Discomfort may radiate to the knee joint or affect the entire leg. The patient begins to limp, dragging the affected limb. Further destruction of the head and its impression fracture provokes acute pain and severe lameness. Against this background, mobility is limited, the patient cannot turn the leg out, flexion and extension movements in the hip joint are limited. Vegetative disorders in the distal sections are also observed - pale and cold feet, increased sweating.
X-ray, MRI, and CT are used for diagnostics. Treatment depends on the stage of the disease, its complications, and symptoms. In most cases, therapy is conservative. Complete unloading of the limb, taking medications to improve blood circulation and stimulate bone tissue growth are indicated. Physiotherapy procedures that maintain muscle tone and accelerate the regeneration process are no less effective.
Osteochondropathy of the femoral head
This is one of the most common forms of degenerative-dystrophic bone disease. It occurs in patients aged 5-12 years. Most often, unilateral damage occurs, but a bilateral pathological process is also possible. The main causes of the disorder include circulatory disorders, injuries, past illnesses, and genetic predisposition.
In the early stages of the disease, the symptoms are blurred. As it progresses, severe pain occurs when walking, muscle atrophy, lameness, and shortening of the affected limb by 1-2 cm. Diagnostic signs of necrosis appear after 6 months. On X-ray, this is determined by uniform darkening of the femoral head due to necrosis and an impression fracture.
Treatment is aimed at restoring the functional capabilities of the affected limb. Limitation of hip joint mobility, use of crutches and orthopedic devices are indicated. Surgical intervention is rarely performed and is aimed at improving blood circulation in the femoral head.
Apophyseal osteochondropathy
Scheuermann-Mau disease is an aseptic necrosis of the apophyses, i.e. the processes of the vertebral bodies. This form of the disease is most often diagnosed in patients during the period of intensive growth, i.e. 11-18 years. The main cause of the pathology is congenital defects in the development of intervertebral discs, a violation of the strength of the endplates of the vertebral bodies. Risk factors include endocrine diseases, functional overloads, injuries. That is, a violation of the ossification process in the growth zone of the vertebral bodies leads to their necrosis and deformation.
Degenerative-dystrophic processes are typical for the VII, VIII, IX and X thoracic vertebrae. It is also possible to affect the lumbar-thoracic and lumbar regions. Symptoms of the disease depend on its stage.
The main signs of necrosis:
- At the first stage, painful sensations are minimal. Asymmetry of the shoulder blades, slightly increased thoracic kyphosis, paravertebral asymmetry are possible. At the level of pathological changes, spinous processes protrude, palpation of which causes pain. Limitation of body tilts is also possible.
- The second stage is characterized by the appearance of ossification of the apophyses. Back pain occurs during prolonged walking or sitting, increased fatigue and muscle weakness of the legs and back. Increased thoracic kyphosis, deformation. Radicular syndrome with limited mobility of the vertebrae develops.
- The third stage is the fusion of the apophyses with the vertebral bodies. It is characterized by kyphosis and wedge-shaped deformation of the vertebral bodies, signs of spinal arthrosis with acute pain syndrome. Fixed kyphosis and lumbar lordosis cannot be corrected.
Diagnostics consists of a set of instrumental and differential methods. Treatment is conservative in most cases. Patients are prescribed general strengthening procedures, vitamins, and a gentle work and rest regime. To develop correct posture, it is necessary to choose a hard mattress, and it is also possible to wear a special corset - a posture corrector.
Swimming, back massage, and physiotherapy procedures have a therapeutic effect. In case of severe kyphosis with neurological complications, surgical intervention is performed. If treatment is started in a timely manner, the disease has a favorable prognosis.
Osteochondropathy of the knee joint
This type of aseptic necrosis is most often diagnosed in children and adolescents. The main cause of knee joint damage is increased mechanical loads and injuries.
The degenerative-dystrophic process includes several pathologies in the knee area, each of which has its own symptoms and localization:
- Koenig's disease is a lesion of the surface of the knee and patellofemoral joint.
- Osgood-Schlatter disease is a necrosis of the tibial tuberosity.
- Sinding-Larsen-Johansson disease is a lesion of the superior/inferior patella.
At the initial stages, the disease does not manifest itself with bright symptoms. Pathology can be suspected by pain syndrome, which increases with physical exertion on the knee. At the same time, discomfort goes away at rest. At later stages of necrosis, the pain becomes permanent.
The disease is diagnosed using ultrasound, MRI, scintigraphy, arthroscopy and differential methods. Both conservative and surgical methods can be used for treatment. In the first case, it is indicated to reduce the load on the knee by fixing it. During the operation, the cartilaginous body is removed with subsequent chondroplasty.
The outcome of the disease depends on its stage and the presence of complications. If you seek medical help in a timely manner, the prognosis is favorable. At later stages, there is a risk of developing gonarthrosis, lameness, and limited movement of the knee joint. Complete recovery of the affected limb takes about 1 year.
Osteochondropathy of the patella
Sinding-Larsen-Johansson disease is an aseptic necrosis in the patella area. Most often, this pathology is detected in patients aged 10-15 years. The disease is polyetiological. The degenerative process can be associated with rupture and separation of a section of bone tissue from the patella due to increased function of the quadriceps muscle.
Symptoms of pathology:
- Increasing pain in the knee joint.
- Swelling of soft tissues in the affected area.
- Quadriceps atrophy/strain.
In some cases, osteochondropathy of the patella occurs against the background of necrosis of the tibial tuberosity, that is, Osgood-Schlatter syndrome.
Various instrumental methods are used for diagnostics. The radiograph shows damage to the cortex of the anterior-lower part of the patella, fragmentation of its lower pole, and periostitis.
Treatment consists of a complex of conservative methods. Patients are shown joint unloading, physiotherapy, massage. If the disease does not respond to conservative treatment, then surgical intervention is performed with the removal of the affected bone.
Osteochondropathy of the clavicle
Destruction and slow restoration of spongy bone tissue of the clavicle is extremely rare. This pathology is called Friedrich syndrome. It is most often diagnosed in adolescent patients. The etiology in most cases is associated with microtrauma.
Signs of the disease:
- Painful swelling in the area of the sternoclavicular joint.
- Pain that increases with physical exertion.
- The radiograph shows thickening of the sternal end of the clavicle and focal enlightenment; the bone tissue is fragmented.
CT, MRI, and X-ray are used for diagnostics. When differentiating, the disease is compared with periostitis, osteomyelitis of the clavicle, and other pathologies. Treatment is conservative. The orthopedist fixes the upper limb on the affected side for 7-10 days. Physiotherapy procedures and taking mineral complexes are also indicated. The prognosis is favorable.
Osteochondropathy of the humerus
The humerus is a part of the skeleton of the upper limb, between the scapula at the top, the ulna and radius at the bottom. It is a long tubular bone, takes part in the formation of the shoulder and elbow joints, ensuring freedom of their movements. The degenerative-dystrophic process is the destruction of bone matter with areas of necrosis and their replacement with fatty tissue.
Damage to the humeral head is one of the causes of aseptic necrosis. The development of the disease may also be associated with the following factors:
- Disruption of blood supply to the bone.
- Compartment syndrome.
- Rough medical manipulations.
- Long-term hormonal therapy with corticosteroids.
- Thrombosis and inflammatory pathologies.
- Immunodeficiency states.
- Radiation or chemotherapy.
- Decompression states.
Aseptic necrosis of the humerus manifests itself as painful sensations upon palpation of the bone and during increased physical activity. As necrosis progresses, the mobility of the affected limb is impaired, the muscles of the shoulder girdle atrophy, and the bone becomes fragile.
Diagnostics consists of a visual examination of the affected area, X-ray, MRI, and laboratory tests. Treatment is drug-based, with a course of physiotherapy. Surgery is performed only in severe cases. With timely treatment, the disease has a positive prognosis.
Osteochondropathy of the tibia
This pathology is a severe degenerative-dystrophic process in bone tissue due to disruption of its blood supply, structure and fatty degeneration of the bone marrow. The disease is polyetiological, but a number of main factors are identified that increase the risk of necrosis:
- Trauma and dysplasia.
- Toxic effects of drugs.
- Osteopenia.
- Osteoporosis.
- Rheumatoid arthritis.
- Ischemic heart disease.
The pathological condition manifests itself in pain in the hip joint and groin area, which can radiate to the knee, lower back, and sacrum. As the disease progresses, the discomfort becomes permanent. The patient begins to limp, the affected limb loses its mobility due to muscle atrophy.
Diagnostics of aseptic necrosis of the tibia consists of plain radiography, MRI, CT, soft tissue scintigraphy. Treatment is conservative: physiotherapy, medication, exercise therapy. Surgery is possible in case of serious degenerative changes.
Osteochondropathy of the fibula
The fibula is a tubular, thin, and long part of the leg. It connects to the tibia, consists of a body and two ends. It functions as an external stabilizer of the ankle joint.
Degenerative-dystrophic lesion of the fibula often occurs against the background of necrosis of the pelvic bones and is manifested by the following symptoms: widening of the joint space, decrease in the height of the epiphyses, and death of bone tissue.
The disease causes pain when moving and palpating the affected area. The pathology is characterized by a cyclical course. Its total duration is from 2 to 4 years. Treatment is complex: medications, physiotherapy, exercise therapy, mineral complexes.
Osteochondropathy of the tibial tuberosity
Osgood-Schlatter disease is one of the most common forms of aseptic necrosis in children. The lesion of the tibial tuberosity is diagnosed in patients aged 10-18 years who are actively involved in sports. The disease can be either unilateral or with symmetrical lesions of both limbs.
The main cause of the disorder is frequent injuries and increased physical activity. The degenerative-dystrophic process manifests itself with the following symptoms:
- Swelling of the lesion.
- Local pain upon palpation and flexion of the limb.
- On palpation, a hard bone growth is detected.
In the early stages, discomfort is intermittent. As it progresses, the pain becomes persistent and intensifies when walking and squatting. Due to swelling, moderate deformation of the anteroproximal part of the shin is observed. This is clearly visible from the side when the knee joint is bent. The tuberosity can be elastic or of dense bone structure.
When making a diagnosis, radiographic signs of pathology are taken into account. A change in the structure and contours of the tibial tuberosity is observed - light areas alternate with dark and structureless ones, a marginal cavity is formed. Differentiation is carried out with recurrent subluxation of the patella, tumors of the cartilaginous tissue, an avulsion fracture of the tibial tuberosity, osteomyelitis, infrapatellar bursitis.
Treatment consists of limiting flexion movements in the knee joints of the affected limb. Patients are prescribed painkillers, medications that strengthen bone tissue and the body. Physiotherapy is aimed at stimulating regenerative processes. Surgical intervention is extremely rare, since there is a risk of damage to the growth zone and the development of synostosis. The disease lasts 1-1.5 years and ends with the restoration of the bone structure. In advanced cases, deformation of the lesion is possible.
Osteochondropathy of the ischium
One of the three parts that form the pelvic bone is the ischium. Aseptic necrosis of this localization is Van Neck syndrome. The disease manifests itself at the age of 6-10 years, in boys more often than in girls. The pathology manifests itself as pain in the hip and groin, reflex lameness, and an increase in body temperature. In some cases, limited pain is observed in the symphysis area.
Instrumental methods are used for diagnostics: radiography, MRI. X-rays reveal spherical expansion in the ischial bone area, one- or two-sided necrosis. The degenerative process is differentiated from tumor lesions of the pelvis, bone tuberculosis, osteomyelitis. Treatment and prognosis depend on the severity of the disease.
Osteochondropathy of the sphenoid bone
Aseptic necrosis of the tarsal bones of the foot (shaped like a wedge) is Künscher's syndrome. The wedge bone is damaged due to impacts, excessive pressure, twisting or bending of the foot. One of the most common causes of the disease is wearing improper shoes that do not correspond to the size and width of the foot.
The degenerative process manifests itself as pain in the foot area, which intensifies during walking. The patient begins to limp, trying not to step on the sore limb. X-rays are taken to confirm the diagnosis. Osteochondropathy of the sphenoid bone is differentiated from its fracture.
Treatment is conservative in most cases. The affected limb is immobilized with a plaster boot, medications are prescribed to improve blood circulation. Physiotherapy procedures that stimulate bone tissue regeneration processes are also recommended.


 [
[