Medical expert of the article
New publications
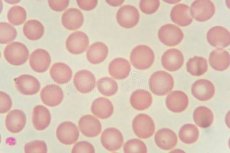
Blood in the smear
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Blood in a smear after a gynecological examination may be normal, but it may indicate a serious pathology. It is necessary to distinguish conditions in which blood in a smear can be a dangerous symptom. To do this, you need to consider all possible options and causes of this problem.
Morphological features of a blood smear
Most women receive normal Pap smear results after a gynecological examination, but many do not know what to do with the results when they come back abnormal. However, abnormal results do not usually indicate a serious pathology. Knowing the causes of an abnormal Pap smear and protecting yourself from the risk factors associated with this result can reduce your chances of having a serious uterine pathology.
The reasons for the appearance of blood in a smear depend on which cells are predominantly found in this smear. After all, blood consists of different cells, and each performs its own function. Accordingly, the detection of predominantly certain cells indicates a certain pathology.
White blood cells in a blood smear are the most important cells that protect the human body. All white blood cells have nuclei, which distinguishes them from others. There are five types of white blood cells. They are divided into two main classes: granulocytes (including neutrophils, eosinophils, and basophils) and agranulocytes (including lymphocytes and monocytes). This classification depends on whether granules can be distinguished in their cytoplasm using a light microscope and conventional staining techniques. All white blood cells are amoeba-like and can migrate from blood vessels into surrounding tissues.
The white blood cell count is often an indicator of disease, and therefore, counting it is an important blood test. The normal white blood cell count in a peripheral blood smear is usually between 4,000 and 10,000 white blood cells per microliter of blood. They make up about 1% of the total blood volume in a healthy adult, making them significantly less numerous than red blood cells at 40-45%. This is normal when it is part of healthy immune responses, which occur frequently. It is sometimes abnormal when it is neoplastic or autoimmune in origin. A decrease below the lower limit is called leukopenia. This indicates a weakened immune system.
Leukocytes in a gynecological smear may also be in small quantities, but their number should not exceed 10 cells. If their number is greater, one can think about inflammatory changes in the cells of the cervix or body of the uterus.
Platelets in a blood smear are a component of blood whose function (along with clotting factors) is to stop bleeding by initiating clotting in blood vessels. Platelets do not have a cell nucleus: they are fragments of cytoplasm that are derived from megakaryocytes in the bone marrow, which then enter the bloodstream. These unactivated platelets are biconvex, discoid (lens-shaped) structures, 2-3 µm in greatest diameter. On a stained blood smear, platelets appear as dark purple spots, about 20% the diameter of red blood cells. The smear is used to examine platelets for size, shape, qualitative count, and clumping. The platelet to red blood cell ratio in healthy adults ranges from 1:10 to 1:20.
The primary function of platelets is to promote hemostasis: the process of stopping bleeding at the site of an interrupted endothelium. They aggregate at the site and, if the vessel interruption is physically too great, they plug the opening. First, platelets attach to substances outside the interrupted endothelium: adhesion. Second, they change shape, turn on receptors, and secrete chemical messengers: activation. Third, they link to each other across receptor bridges: aggregation. The formation of this platelet plug (primary hemostasis) is associated with activation of the coagulation cascade with resulting fibrin deposition and binding (secondary hemostasis). The end result is a clot.
A low platelet count is thrombocytopenia and is due to either decreased production or increased destruction. An elevated platelet count is thrombocytosis and is either congenital or due to unregulated production.
Platelet concentration is measured either manually using a hemocytometer or by placing blood in an automated platelet analyzer. The normal range of these cells in peripheral blood is 150,000 to 400,000 per microliter.
Red blood cells in a blood smear are the most common type of blood cell and the primary means of delivering oxygen to the body's tissues through the circulatory system. The cytoplasm of red blood cells is rich in hemoglobin, an iron-containing biomolecule that can bind oxygen and is responsible for the cells' red color. The cell membrane is composed of proteins and lipids, and this structure provides properties essential to the cells' physiological function, such as stability as they traverse the circulatory system and, in particular, the capillary network.
In humans, mature red blood cells are flexible, oval, biconvex discs. They lack a cell nucleus and most organelles to provide maximum space for hemoglobin; they can be thought of as sacks of hemoglobin. Approximately 2.4 million new red blood cells are produced per second in adults. The cells develop in the bone marrow and circulate for about 100-120 days in the body before their components are recycled by macrophages. Each circulation takes about 60 seconds (one minute). About a quarter of the cells in the human body are red blood cells.
When red blood cells are stressed by narrowed vessels, they release ATP, which causes the vessel walls to relax and dilate to promote normal blood flow. When hemoglobin molecules are deoxygenated, red blood cells release S-nitrosothiols, which also act to dilate blood vessels, thereby sending more blood to oxygen-depleted areas of the body.
Red blood cells can also synthesize nitric oxide enzymatically using L-arginine as a substrate, as do endothelial cells. Exposure of red blood cells to physiological levels of shear stress activates nitric oxide synthase and nitric oxide export, which may contribute to the regulation of vascular tone.
Red blood cells also play a role in the body's immune response: when lysed by pathogens such as bacteria, their hemoglobin releases free radicals that destroy the pathogen's cell wall and membrane, killing it.
Women have about 4-5 million red blood cells per microliter (cubic millimeter).
Reticulocytes in a blood smear are immature red blood cells that typically make up about 1% of the red blood cells in the human body. During the process of erythropoiesis (the formation of red blood cells), reticulocytes develop and then circulate for about a day in the bloodstream before developing into mature red blood cells. They are called reticulocytes because of the mesh-like network of ribosomal RNA that becomes visible under a microscope with certain stains. Reticulocytes appear slightly bluer than other red blood cells. The normal percentage of reticulocytes in the blood depends on the clinical situation, but is typically between 0.5% and 2.5%. This percentage is in the normal range for normal red blood cell levels; for example, if someone is anemic but has a reticulocyte percentage of only 1%, the bone marrow is probably not producing new blood cells at a rate that will correct the anemia.
The reticulocyte count is a good indicator of bone marrow activity because it represents recent production and allows the reticulocyte count and reticulocyte production index to be determined. These values can be used to determine whether a production problem is contributing to anemia and can also be used to monitor the progress of treatment for anemia.
Mononuclear cells in a blood smear are any cell in the peripheral blood that has a round nucleus. These cells consist of lymphocytes (T cells, B cells, NK cells) and monocytes. Mononuclear cells are the largest type of white blood cell and can differentiate into macrophages and the myeloid lineage of dendritic cells. In humans, lymphocytes make up the majority of the mononuclear cell population, followed by monocytes and only a small percentage of dendritic cells. Monocytes are produced in the bone marrow from precursors called monoblasts, bipotent cells that differentiate from hematopoietic stem cells. Monocytes circulate in the bloodstream for about one to three days and then typically travel to tissues throughout the body, where they differentiate into macrophages and dendritic cells. They make up three to eight percent of the white blood cells in the blood. About half of the body's monocytes are stored as a reserve in the spleen. Monocytes that migrate from the blood to other tissues will then differentiate into tissue-resident macrophages or dendritic cells. Macrophages are responsible for protecting tissues from foreign substances, but are also suspected of being important in the formation of important organs such as the heart and brain. They are cells that have a large, smooth nucleus, a large cytoplasmic area, and many internal vesicles for processing foreign material.
Mononuclear cells perform three major functions of the immune system. These are phagocytosis, antigen presentation, and cytokine production. Phagocytosis is the process of ingesting microbes and particles and then breaking down and destroying that material. Monocytes can perform phagocytosis using intermediate (opsonizing) proteins such as antibodies or complement that coat the pathogen, as well as by binding to the microbe directly through pattern recognition receptors that recognize pathogens. Monocytes are also capable of killing infected cells through antibody-dependent cell-mediated cytotoxicity.
Eosinophils in a blood smear are one of the components of the immune system responsible for fighting multicellular parasites and some infections. These cells are eosinophilic or "acid-loving" due to their large acidophilic cytoplasmic granules, which show their affinity for acids. Inside the cells are small granules that contain many chemical mediators such as eosinophil peroxidase, ribonuclease (RNase), deoxyribonuclease (DNase), lipase. These mediators are released by a process called degranulation after eosinophil activation and are toxic to the parasite tissue.
Eosinophils make up about 1-3% of white blood cells. Eosinophils persist in the circulation for 8-12 hours and can survive in tissue for an additional 8-12 days in the absence of stimulation.
There are also eosinophils, which play a role in fighting viral infections, as evident from the abundance of RNases they contain within their granules and in the removal of fibrin during inflammation. Eosinophils, along with basophils and mast cells, are important mediators of allergic reactions and the pathogenesis of asthma and are associated with the severity of the disease.
Reasons for the appearance of blood in a smear
It is natural to have blood in the smear after a vaginal examination, because although it is a non-traumatic method, a small injury to the endothelial mucosa may occur. This happens to both pregnant women and women who are not pregnant. The cervix and vaginal area are very delicate and have blood cells very close to the surface. During a normal routine smear, even normal cleaning can cause a small amount of bleeding. Usually, the bleeding stops on its own. But if there is a significant amount of blood in the smear and there are different blood cells, then you need to look for the cause of this condition.
Why is a smear test performed in women? At each preventive examination, a smear is taken for its examination. The very concept of "preventive examination" suggests that it is carried out in order to exclude any pathology in a timely manner. Cervical screening is the process of detecting abnormal tissue. In an effort to detect and treat early neoplasia, screening is aimed at secondary prevention. Several screening methods are the Pap test (also known as the Pap smear), liquid-based cytology, HPV DNA testing, and visual inspection with acetic acid. Promising screening methods that can be used in low-resource areas in developing countries are HPV DNA testing and visual inspection.
Conventional cytology allows us to identify cells and suspect pathology.
The reasons for the appearance of blood in a gynecological smear in women of reproductive age are as follows:
- Hormonal imbalance;
- Tubal or ectopic pregnancy (during examination, incorrect fixation of the embryo can cause partial or complete detachment of the placenta and bleeding);
- Placenta accreta is a pregnancy in which the placenta is located near or near the cervix;
- Uterine fibroids (the nodular form can often bleed during examination);
- Certain types of cysts and tumors (for example, a polyp is a finger-like protrusion from the cervix filled with blood that may bleed);
- Endometriosis (involves the location of areas of the endometrium outside the uterine cavity, which are prone to periodic bleeding);
- Use of birth control (in non-pregnant women, bleeding is more likely if you take birth control pills, which increase hormone levels and make the cervix more sensitive);
- Intrauterine devices (create the risk of additional trauma);
- Infections: Vaginitis can be caused by yeast, bacteria, and trichomonas.
In postmenopausal women, the reasons for the appearance of blood in a smear may be limited to the following cases:
- Effect of hormone replacement therapy;
- Cervical cancer or other cancer sites;
- Some tumors (non-cancerous);
- Atrophic vaginitis (makes the mucous membrane very dry and easily injured).
Risk factors
The risk factors for blood in a smear during pregnancy are higher, but in such cases it is usually not caused by pathology. In pregnant women, blood vessels are more sensitive and bleed more easily. Pregnant women should have a smear test early in pregnancy as part of a routine prenatal check.
Clinical manifestations of pathologies accompanied by an abnormal smear
When it comes to a particular pathology of the female reproductive system, symptoms may not appear immediately. That is why it is so important to undergo an annual examination with a smear test. But sometimes there are manifestations of pathologies that a woman does not pay attention to.
Blood may appear when taking a smear from the cervical canal when a woman is in the secretory phase of the cycle and the vessels are located superficially. But if we talk about pathology, then blood may appear with cancer. It is associated with abnormal growth of cells that have the ability to penetrate or spread to other parts of the body. The first signs are most often local changes, which are determined in the smear. Later symptoms may include abnormal vaginal bleeding, pain.
Human papillomavirus infection causes more than 90% of cases.
Vaginal bleeding, contact bleeding (one of the most common forms of bleeding after intercourse), or (rarely) a vaginal mass may indicate malignancy. With advanced disease, metastases may be present in the abdomen, lungs, or elsewhere.
Another reason for bleeding after a pap smear may be a benign tumor, uterine fibroids. Uterine fibroids are nodules of smooth muscle cells and fibrous connective tissue that develop in the wall of the uterus. The nodules may grow inside the wall of the uterus, or they may project into the internal cavity or onto the external surface of the uterus. Most fibroids occur in women of reproductive age, and they are rare in younger women.
The first signs of uterine fibroids may appear only when they reach significant sizes. If a woman is not examined in time, then fibroids are detected late. Symptoms of fibroids may manifest as bleeding after taking a smear. This is explained by the fact that the node is traumatized, which causes minor bleeding. But, nevertheless, this contributes to early diagnosis.
Endometriosis is a common cause of blood on a pap smear in women of reproductive age. The name endometriosis comes from the word "endometrium," the tissue that lines the inside of the uterus. In endometriosis, tissue that looks and acts like endometrial tissue is located outside the uterus, usually inside the abdominal cavity.
At the end of each cycle, when hormones cause the uterus to secrete, the endometrial tissue growing outside the uterus bleeds. The tissue surrounding the area of endometriosis may become inflamed or swollen. Inflammation can cause scar tissue around the area of endometriosis.
The most common symptom is bleeding when the smear is taken. Other symptoms may include pain, especially excessive menstrual cramps (dysmenorrhea), which may be felt in the abdomen or lower back during or after sexual activity. Infertility occurs in 30-40% of women with endometriosis.
Infections are one of the causes that can cause vaginitis of varying severity. Chlamydia is a pathogen that can cause vaginitis. These parasites are inside the cells, so they are rarely detected when examining a smear. Symptoms in women may include vaginal discharge, including bloody discharge. In women of reproductive age, this pathogen can cause infertility. But since it is difficult to detect in a vaginal smear, it is necessary to conduct a blood test for the pathogen even with a negative cytological smear. When antibodies to chlamydia are present in the blood, but not in the smear, this indicates that the woman has an active chlamydial infection.
The situation is similar with ureaplasma. The pathogen also belongs to intracellular parasites, so if there are antibodies to ureaplasma in the blood, but not in the smear, then the infection still exists in the body.
Trypanosoma in a blood smear is a symptom of a serious disease. Trypanosoma is a genus of single-celled parasitic flagellate protozoa. Most species are transmitted by blood-sucking invertebrates, but there are different mechanisms between different species. Trypanosomes infect many hosts and cause a variety of diseases, including fatal diseases. If this pathogen is suspected, a thorough examination is carried out, including blood. Since the intracellular stages of the trypanosome life cycle are usually found in human red blood cells, a smear is necessarily examined, and if trypanosoma is in the smear, the diagnosis is confirmed.
Cytomegalovirus is an intracellular persistent virus in humans. Often, women are worried about the results when they are tested for this virus before planning a pregnancy. When cytomegalovirus is present in a smear but not in the blood, this does not indicate an active infection. After all, it can be inside cells all life, but the woman does not get sick. Therefore, if the acute phase antibodies (M) are negative, there is no need to worry.
The consequences and complications depend on the pathology that caused the bleeding or bad smear. If the process is malignant, the consequences of untreated pathology can be fatal.
Treatment
What to do if the smear on cytology is bad? Of course, it all depends on what cells are detected. If suspicious cells are noted in the cervical cytology that accompanies the sample, the laboratory should make a recommendation for a colposcopy. Colposcopy is a procedure that looks at the uterus by magnifying it under a microscope. The doctor can see the endometrium and the openings of the fallopian tubes, which is not visible during a normal examination. This procedure is minimally invasive and allows for a direct view of the endometrium and a sample for biopsy.
Treatment must be etiologic. If the cause of blood in the smear is confirmed cancer, then treatment should not be delayed under any circumstances. Since cervical cancer is radiosensitive, radiation can be used at all stages. Surgery can have better results than radiological approaches. In addition, chemotherapy can be used at certain stages or in combination with other methods.
Uterine fibroids are not treated actively if they are in the early stages of development. As they grow, hormonal combination drugs can be used, and when they reach large sizes, surgical treatment is required.
Although there is no cure for endometriosis, there are two types of interventions: pain management and treatment of endometriosis-related infertility. In many women, menopause (natural or surgical) will reduce the process. In women of reproductive years, endometriosis is simply managed: the goal is to provide pain relief, limit progression of the process, and restore or preserve fertility where necessary. In general, the diagnosis of endometriosis is confirmed at the time of surgery, at which time ablative steps can be taken. Endometriosis ablation (burning and vaporizing the lesions with an electrical device) has shown a high rate of short-term recurrence after the procedure.
Conservative treatment may increase the risk of recurrence.
Infections that cause blood in a smear or other types of discharge require active drug treatment. Drugs are used according to the pathogen and its sensitivity to certain drugs. It should be taken into account that genital tract infections are mostly caused by intracellular pathogens, so the course of antibacterial drugs can be long.
Traditional methods of treatment and homeopathy are not used, since active infectious processes or neoplastic ones are not subject to such types of treatment. If traditional methods are used for a long time without drug therapy, this can lead to complications.
Prevention
Prevention of bad results in smear cytology is maintaining the health of a woman's reproductive system. It is very important to undergo preventive examinations in a timely manner, because this is the key to a timely diagnosis of the disease.
Forecast
The prognosis in most cases when blood appears in a smear is positive, because this is usually a normal reaction. If there is a pathology, the smear will allow you to determine its type quite informatively and start treatment in time.
The appearance of blood in a smear for cytology during a gynecological examination can sometimes frighten women. But it is not always so scary, because everything depends on what blood elements are found there. You should always wait for the full results of the examination and discuss them with the doctor, without panicking ahead of time and without self-medication.


 [
[