Medical expert of the article
New publications
Balantidiasis: all about the disease, clinical guidelines
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Balantidiasis is a protozoan infectious intestinal disease caused by ciliated infusoria - balantidia. Balantidiasis is accompanied by ulcerative-inflammatory changes in the walls of the large intestine, which is clinically manifested by abdominal pain, diarrhea, weight loss, signs of intoxication damage. The disease is often severe, with a high probability of patient death if treatment is delayed.
Epidemiology
Balantidiasis is registered mainly in rural areas. The disease is especially widespread in African, Latin American regions and Asian countries. According to statistics, it is the representatives of these regions who suffer from balantidiasis most often: today, about 200 million people are considered infected.
The disease spreads primarily due to the lack of adequate methods for treating patients who are carriers of the pathogenic microorganism.
The mortality rate of balantidiasis is quite high – about 10-30%. Such a high rate is due to the frequent development of complications and rapid depletion of the patient’s body.
In our country, the disease is also relatively common: this is facilitated by the widespread disregard for sanitary and hygienic standards, insufficient social support of the population, and the lack of necessary attention from the medical community (weak educational and preventive activities).
 [ 9 ]
[ 9 ]
Causes balantidiasis
The causative agent of the zoonotic intestinal disease called "balantidiasis" is the unicellular organism Balantidia coli, which exists in a vegetative and cystic variant. Balantidia coli is the largest pathogenic protozoan. The vegetative variant is represented by an ovoid form with an oral cavity gap on the anterior edge. The body is covered with longitudinally localized cilia (the microorganism needs them to move). The diameter of the cyst is approximately 50 µm.
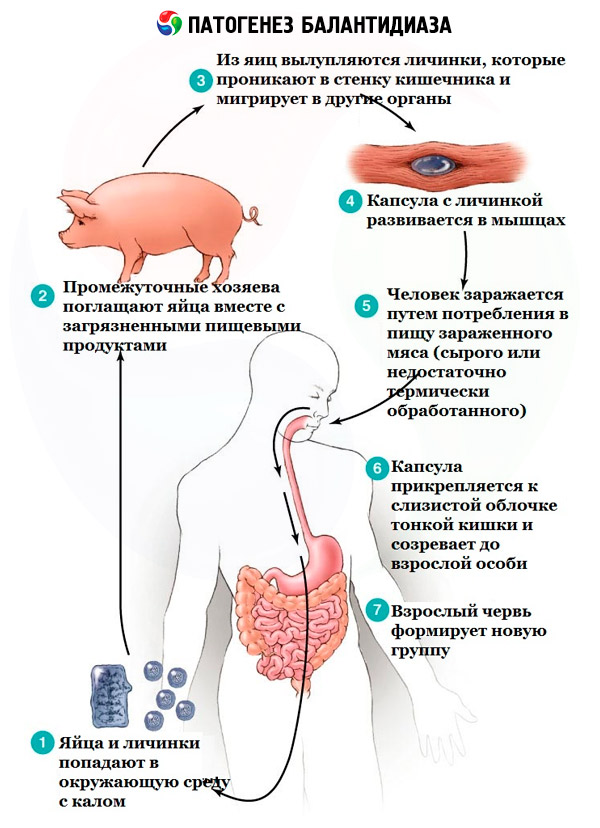
Balantidiasis is acquired by people who have direct contact with pigs or with plant products or water infected with cysts.
The immediate causes are considered to be:
- ignoring sanitary and hygienic standards;
- failure to comply with sanitary conditions for the care of pigs;
- failure to observe personal hygiene rules;
- consumption of contaminated drinking water, unwashed vegetables, etc.
Risk factors
The incidence is higher in rural areas: approximately 5% of villagers suffer from balantidiasis. Workers at pig farms and pig complexes are at particular risk, since pigs are the creatures most often affected by the pathogen. People become infected through the feco-oral route, through unwashed hands, and by consuming contaminated water or food products.
 [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
Pathogenesis
Human infection can occur after the causative agent of balantidiasis (mainly cysts) enters the digestive system. Balantidia can exist in the human intestinal cavity for a long time without developing pathology. The infectious agent usually settles in the lower segment of the small intestine. Penetration into intestinal tissue does not occur in all cases, and the exact reason for such selectivity is unknown.
Tissue damage by balantidia mainly affects the cecum, sigmoid colon and rectum. At the initial stage of balantidiasis, zones of swelling and redness are formed in the folded structure of the mucous membranes. Then an erosive focus is formed. Pathogens penetrate deep into the tissues, hemorrhages appear, and necrotic processes occur. Necrotic masses are rejected, and a cavity is formed in their place, which goes into the intestinal lumen. Ulcers are characterized by irregularly shaped borders, thick and excised edges, an uneven bottom covered with purulent-bloody secretion. There is a high probability of ulcerative perforation, with a further inflammatory process in the form of peritonitis.
Stages of balantidiasis according to pathogenetic data:
- Infection stage (balantidia enter the human digestive system, as a result of which the person becomes a carrier or the disease develops).
- The stage of penetration of an infectious agent into the intestinal wall with further development of the inflammatory process (the enzyme hyaluronidase facilitates the penetration of the agent into the intestinal wall, inflammation develops, the composition of the intestinal flora changes, and the large intestine is affected).
- Intoxication stage (as a result of the inflammatory process, toxic components are absorbed into the bloodstream and an intoxication syndrome develops, which manifests itself as fatigue, headache, and insomnia).
- Diarrheal stage (the intestines are affected, frequent loose stools with mucous and bloody particles and a “rotten” odor appear, symptoms of dehydration occur, the patient rapidly loses weight).
- Abdominal stage (pain appears in the lower abdomen, tenesmus, pain when palpating the intestinal projection area).
- The stage of dissemination of Balantidia (the pathogen spreads through the bloodstream into the mesenteric lymph node system, into the liver, genitourinary system, and lungs).
- Stage of development of complications (ulcer perforation, peritonitis, internal bleeding, secondary infection are observed).
Source of distribution of balantidiasis
Pigs are considered to be the main source of the spread of the balantidiasis pathogen: their invasion is determined by 60-80 percent. In some cases, a person can be a carrier, but infection from them is practically excluded: in the human body, the formation of cysts occurs rarely and in small numbers.
Infection with the vegetative variant is considered impossible, since such forms quickly die both outside a living organism and in the acidic contents of the stomach.
The cystic variant can remain viable in a pig-breeding environment for up to 14 days, and in the ground for up to 244 days. When treated with disinfectant liquids, the cysts die within a few hours.
 [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ]
[ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ]
Routes of infection
The route of infection is feco-oral. Infection occurs through dirty hands, contaminated drinking water, unwashed vegetables or fruits (water, food and contact routes).
Symptoms balantidiasis
The duration of the incubation period for balantidiasis is determined by an average of 2 weeks (the minimum recorded period was five days, and the maximum was 30 days).
Balantidiasis does not always manifest itself with any symptoms, as it can occur in a latent form and in the form of a carrier. In other cases, acute and chronic forms of the pathology are diagnosed, often in combination with other inflammatory and parasitic processes (for example, amebiasis, shigellosis, etc.).
- The acute form of balantidiasis is characterized by an acute onset. The first signs of the problem are general fatigue, headache, loss of appetite, nausea, and a marked increase in temperature. Soon, symptoms of intestinal damage are added: abdominal pain, spasms, frequent and ineffective urge to defecate, and diarrhea. The feces are liquid, with particles of blood and pus, foul-smelling; defecation is observed from 3-4 to 18-20 times a day. The patient becomes very and quickly exhausted, loses weight; the surface of the tongue becomes covered with a "dirty" coating, palpation of the abdomen is painful along the intestine. Liver enlargement is possible. Endoscopically, a catarrhal-hemorrhagic inflammatory process and the formation of ulcers can be detected. Biopsy analysis indicates the accumulation of balantidia in the submucosal tissues, as well as at the edges of ulcers and in abscesses. If left untreated for 6-8 weeks, the acute course of balantidiasis transforms into a chronic one.
- Chronic balantidiasis often has a recurring ability: exacerbations last from one week to a month, and the period of calm of the disease - from three months to six months. Signs of intoxication are not fully manifested, the temperature does not always rise. The main clinical picture is manifested by local signs: frequent loose stools with inclusions of mucus, pus, blood. Examination allows you to pay attention to the "coated" surface of the tongue, pain when palpating the large intestine. It is also possible that chronic balantidiasis is not recurrent, but continuous. This option is always manifested by increasing exhaustion and cachexia of the patient.
 [ 30 ]
[ 30 ]
Balantidiasis in men
Cases of balantidiasis can be recorded in homosexuals, during anal sexual contact with a carrier, sick with a chronic form of the disease. In a sick man, a combined inflammatory process of the skin of the head and the inner leaflet of the foreskin of the penis develops. It is possible to form painful ulcers covered with granulations, with purulent foul secretion, inflammation and enlargement of the inguinal lymph nodes. Sometimes, representatives of non-traditional sexual orientation are found to have warty ulcers in the genital area and anus. Complications in this case are prostatitis, epididymitis.
 [ 31 ]
[ 31 ]
Balantidiasis in children
Children can become infected with balantidiasis by drinking contaminated water or eating unwashed vegetables. Deaths among sick children are often the result of improper treatment: the disease is mistaken for ordinary diarrhea or food poisoning, so it is treated fundamentally incorrectly. In addition, a latent form of balantidiasis is often registered.
Balantidiasis in childhood manifests itself as bloody diarrhea of the dysenteric type. General symptoms are supplemented by damage to other internal organs (liver, lungs). As a rule, the disease begins with "indigestion", general weakness, loss of appetite, frequent loose stools. For several days, the child is bothered by tenesmus: he may ask to go to the toilet, but there is no stool output. Mucus mixed with pus and blood may be released. The clinical picture is supplemented by vomiting, pain in the lower abdomen, and fever. The child's body quickly becomes dehydrated.
Forms
Balantidiasis can proceed typically (with full clinical manifestations) and atypically (in the form of a latent form, or carriage).
The following course variants are characteristic of balantidiasis:
- monodisease;
- combined disease (most often combined with lesions caused by amoebas, shigella, etc.).
Balantidiasis is differentiated depending on the severity:
- light type;
- medium-heavy type;
- severe type of pathology.
The nature of the disease can be:
- uncomplicated;
- complicated.
Complications and consequences
The main complications of balantidiasis are considered to be the following diseases:
- Ulcer perforation is the formation of a through hole in the intestinal wall. The contents of the intestine enter the abdominal cavity, as a result of which peritonitis develops.
- Intraintestinal bleeding is the release of blood into the intestinal cavity with subsequent shortage of circulating blood volume. This complication is quite serious and requires immediate medical attention.
- General exhaustion, weight loss, cachexia are critical conditions that include profound metabolic disorders with an increasing deficiency of fats and carbohydrates, with increased protein catabolism and a slowdown in its synthesis.
- The addition of a secondary infection consists of infection with another type of microorganism, against the background of existing balantidiasis.
Resistance to balantidiasis
Acquired immunity in balantidiasis is usually unstable and non-sterile, so a person who has recovered from the disease is not protected from relapses or reinfection.
 [ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ]
[ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ]
Diagnostics balantidiasis
Diagnosis begins with a physical examination:
- the general condition of the patient is assessed;
- the presence of symptoms of dehydration is checked;
- the functionality of the heart and vascular network is assessed (blood pressure is measured, heart sounds are listened to);
- The abdominal area is palpated, signs of peritoneal irritation are checked, and the condition of the liver is determined.
It is important to visually examine the patient's feces. Only after this do they begin laboratory research methods.
A clinical blood test for balantidiasis reveals hypochromic anemia, neutrophilic leukocytosis, slight eosinophilia, and an accelerated ESR.
Blood biochemistry shows hypoalbuminemia and hypoproteinemia.
Laboratory tests can detect vegetative variants and cysts of Balantidia; leukocytes, erythrocytes, and mucus in feces (coprogram) are also determined. In addition, genetic material of Balantidia is found in feces.
Instrumental diagnostics consists of the following procedures:
- comprehensive ultrasound examination of internal organs (helps to identify complications of balantidiasis);
- endoscopy (fibrocolonoscopy, helps to detect ulcerative-erosive changes in the mucous membrane of the large intestine);
- general radiography of internal organs (helps to detect free gas in the abdominal cavity caused by intestinal perforations).
 [ 47 ]
[ 47 ]
Differential diagnosis
Differential diagnostics should be carried out with acute bacterial intestinal lesions that occur with signs of bleeding intestinal inflammation: this may be a lesion by shigella, campylobacter, salmonella. Differentiation with other parasitic pathologies that involve gastrointestinal inflammation (this is possible with amebiasis, schistosomiasis, ankylostomiasis), as well as with ulcerative colitis, Crohn's disease, acute appendicitis, intestinal obstruction, intestinal tuberculosis is also important.
To clarify the diagnosis, it is necessary to take into account epidemiological, symptomatic, laboratory and instrumental information, as well as the results of additional diagnostic methods.
Who to contact?
Treatment balantidiasis
The use of medications for balantidiasis involves the inclusion of antiparasitic, symptomatic drugs, as well as agents to stabilize the balance of intestinal flora and immune protection.
A sick person is subject to isolation - at home or in a hospital (placed in a separate ward-box, or in a ward with other patients with a similar nosology).
The infectious focus (place of residence, work of the patient) is treated according to preventive recommendations used to prevent infectious diseases with a fecal-oral method of infection. The patient is given individual dishes and household items. People who have been in contact with the sick person undergo a stool test for the presence of balantidia: they do not need quarantine isolation. It is possible to register for a dispensary during the year.
Asymptomatic carriage may result in spontaneous recovery, but in some cases treatment with metronidazole or iodoquinol is prescribed.
Clinical guidelines for the treatment of balantidiasis
Clinical guidelines are a normative and standard health document that defines the requirements for providing medical care to a patient with balantidiasis. Such care is provided in stages:
- A patient with suspected balantidiasis undergoes laboratory diagnostics.
- After laboratory confirmation of balantidiasis is received, additional studies are carried out to assess the likelihood of complications.
- Treatment is prescribed according to the severity of the disease. If necessary, therapy is adjusted depending on the appearance of new symptoms or if individual medications are ineffective.
- After recovery, the patient is placed on dispensary register.
Medicines: what can a doctor prescribe for balantidiasis?
Tetracycline |
The course of treatment is designed for 10 days. Adults take 500 mg 4 times a day, children (starting from the age of seven) - at the rate of 10 mg/kg 4 times a day (the maximum daily amount for a child is 2 g). |
Monomycin |
Monomycin is taken orally at 0.6-1.5 g/day, in two cycles of five days, with an interval between cycles also of five days. |
Metronidazole |
Metronidazole is prescribed in two or three five-day cycles, 500 mg three times a day. The time interval between cycles is 5 days. |
Dextrose |
It is used for dehydration according to indications. |
Sodium chloride |
It is used for dehydration according to indications. |
Enterol |
Take 1-2 sachets twice a day for 10-14 days. Rarely, the drug can cause allergic reactions. |
Linex |
Adults take two capsules of Linex three times a day. Side effects are practically absent, only rarely can hypersensitivity reactions be discussed. |
Dioctahedral smectite |
Prescribed according to individual indications. In large doses or with prolonged use, it can cause constipation. |
Ibuprofen |
Prescribed at a rate of 20-30 mg per kilogram of body weight per day. The average amount of the drug is 200-400 mg every 4-6 hours. Do not take more than 1200 mg per day. Side effects: stomach pain, allergy. |
Paracetamol |
Take 500-1000 mg every five hours, not exceeding the daily dosage of 4000 mg. It is not recommended to use the drug for more than 3-4 days. |
No-shpa |
Prescribed at 120-240 mg/day, divided into 2-3 doses. Side effects: headache, decreased blood pressure, sleep disorders. |
Papaverine |
Administer intramuscularly 0.5-2 ml of 2% solution. The duration of the treatment course is determined individually. During treatment, the patient may experience headaches and dry mouth. |
Cetirizine |
The drug is prescribed in the amount of 10 mg once a day. Side effects of Cetirizine are thrombocytopenia, dizziness, hypersensitivity reactions. |
Azoximer bromide |
An immunostimulant that is administered subcutaneously at 6-12 mg daily for 5-10 days. Intramuscular, sublingual and rectal administration of the drug is also possible. Contraindications: children under 12 years of age, pregnancy. |
Vitamins for balantidiasis
In addition to antibacterial treatment, balantidiasis is treated with medications that help increase the body's immune defense: tinctures of eleutherococcus, magnolia vine, and ginseng. Vitamin therapy is also indicated.
Most existing vitamins can be used to support immunity, but in case of balantidiasis, their dosage should be increased at least twice. This is due to the increased consumption of nutrients during infection, as well as their increased excretion as a result of dehydration.
Vitamin deficiency should be compensated for by taking multivitamins – both throughout the entire treatment period and during the recovery phase of the body.
In the fight against infection, it is necessary to focus on such vitamins as ascorbic acid, riboflavin (vitamin B 2 ), retinol (vitamin A), tocopherol (vitamin E). These vitamins participate in the work of the immune system, increase the protective functions of the skin and mucous membranes, activate the reaction of leukocytes, and accelerate regenerative processes.
Vitamins for balantidiasis are an integral part of complex treatment. According to research results, enhanced vitamin therapy in combination with a balanced vitamin-rich diet can shorten the period of the disease and reduce the risk of complications.
Physiotherapy treatment for balantidiasis
There are many known physiotherapy methods that can speed up the recovery of the body after the acute period of balantidiasis. These are, first of all, thermal procedures (ozokerite, therapeutic mud, peat and paraffin applications, UHF therapy), hydrotherapy, electrophoresis with novocaine and papaverine.
After the main symptoms have subsided, the following are indicated:
- taking baths (pine, radon, pearl, oxygen);
- the effect of heat on the epigastric region (ozokerite, therapeutic mud, paraffin).
The indicated methods are used only in inpatient or outpatient settings.
Outside the acute period, treatment with baths and applications is allowed at home. After 8-12 weeks, at the recovery stage, spa treatment, peat and mud therapy, sea and pine baths, hydrotherapy, etc. are indicated. Patients are especially recommended to visit such sanatoriums as Essentuki, Zheleznovodsk, Dorokhovo, etc.
Folk treatment for balantidiasis
To quickly relieve the unpleasant symptoms of balantidiasis, some traditional medicine recipes may be useful:
- For 200 ml of boiling water take 2 tbsp. of blackberry leaves, boil for five minutes, then cover with a lid and a towel, leave for half an hour, filter. Drink the potion three times a day, one glass at a time.
- Add a quarter spoon of ground cinnamon and a pinch of ground hot pepper to a glass of boiling water. Cover with a lid and let steep for 20-30 minutes. Drink warm, all at once. The procedure can be repeated 2-3 times a day.
- Potato starch (1 tsp) is poured into 100 ml of water at room temperature, stirred and drunk immediately.
- Drink 100-150 ml of vodka tincture made from walnut partitions at a time.
- Mix a third of a teaspoon of salt and 75-85 ml of vodka and drink in one go.
The arsenal of folk recipes can be successfully supplemented by the use of herbal infusions and herbs. Herbal treatment will help with this.
Herbal treatment
The following herbal infusions will help ease the course of balantidiasis and speed up recovery:
- Take 2 tablespoons of cinquefoil rhizome, alder cones, and nettle rhizome. Keep in a water bath in 500 ml of water for ten minutes, then leave for about two hours under a lid. Take 100 ml 4 times a day before meals.
- Take equal amounts of cinquefoil, burnet rhizome and shepherd's purse. Infuse 5 tbsp of the mixture in 1 liter of boiling water for several hours. Take 100 ml on an empty stomach 4 times a day.
- Take equal amounts of wormwood, lady's mantle and marshmallow root. Steam 2 tbsp of the mixture in 500 ml of boiling water, leave for 2 hours. Take 100 ml of the infusion on an empty stomach 4 times a day.
- Take equal parts of silverweed, deadnettle, plantain and knotweed. About 50 g of the mixture is poured with 500 ml of boiling water, and infused for 30 minutes. Take 50-60 ml three times a day.
- An equal mixture is prepared from the rhizome of knotweed, blueberries and burnet. One teaspoon of the mixture is poured with a glass of boiling water and infused for an hour. The infusion is taken during the day, 100 ml (approximately 5 times a day).
Homeopathy for Balantidiasis
Homeopathic treatment has many advantages: it is effective, safe, suitable for adults, children and pregnant women. However, at the acute stage of balantidiasis, it is recommended to take homeopathic drugs only after consulting a doctor, since additional medications can "blur" clinical manifestations and make it difficult to determine the tactics of traditional treatment.
What medications does homeopathy recommend for balantidiasis:
- Colocynth - can be prescribed to relieve spasms and painful attacks;
- Lycopodium – helps eliminate flatulence and excess gas in the intestines;
- Nux vomica – normalizes digestive processes, removes toxic substances from the body;
- Hina is a drug that is usually prescribed at the stage of recovery of the body after balantidiasis. The course of taking the drug is designed for five days;
- Baptisia – helps to alleviate the main symptoms of the disease (indigestion, fatigue, muscle pain);
- Veratrum album - helps with severe vomiting and diarrhea, general weakness and low blood pressure.
Prevention
Preventive measures include maintaining personal safety (following hygiene rules, boiling water, washing plant products), preventing faecal contamination of water and soil (monitoring zoological hygiene on farms and livestock bases, neutralizing manure, etc.).
There is no specific prevention for the development of balantidiasis.
Additionally, it is necessary to pay attention to the implementation of such events:
- sanitary and hygienic rules, sanitary supervision of places of breeding and keeping pigs;
- control of meat processing plants, food service facilities, water supply systems;
- compliance with regular disinfection;
- strict adherence to personal hygiene standards, washing hands with soap, eating only thoroughly washed vegetables and fruits;
- maintaining food hygiene (eating fresh, high-quality food, eating in adequate conditions);
- strengthening the immune system;
- refusal to share things and utensils in everyday life.
Forecast
If the treatment of the disease was started in a timely manner, and the therapeutic scheme included complex and competent prescriptions, then the prognosis can be classified as favorable. In the absence of treatment, the mortality rate is 10-30%.
Most often, balantidiasis is treated in a hospital setting. The patient is discharged after the acute period of the disease has ended, after the general condition has normalized and the basic pathological signs have been eliminated (after about three weeks). After recovery, the patient can return to his previous rhythm of life (go to work or school), if the results of stool tests for the presence of balantidia were negative (three times during the week).
 [ 56 ]
[ 56 ]

