Medical expert of the article
New publications
Babesia
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
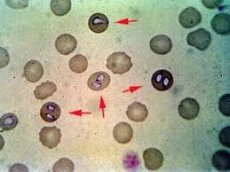
Babesia is an intracellular parasite that affects red blood cells in the blood of animals and humans. Let's consider the pathogenesis of babesia, structure, diseases caused by parasites, the main symptoms of babesiosis and treatment methods.
Babesia belongs to the order of the simplest piroplasms of the sarcod class. The parasite received its name in honor of the scientist V. Babesh, who was the first to discover babesia in the blood of cattle. The parasite has four species: Piroplasma, Nuttallia, Babesiella, Francaiella, which cause babesiellosis.
The main carriers of babesia are Ixodidae ticks. Human babesiosis was first diagnosed in Europe. Later, the disease was recorded in the United States and spread to other countries. Today, babesia causes serious diseases not only in animals, but also in humans, which are difficult to diagnose and treat.
Structure of Babesia
The structure of babesia corresponds to the structure of any parasitic microorganisms. Babesia belongs to the type of aplicomplexes, the order of paraplasmids and the family of babesia. The genus Babesia does not have a single classification, so some scientists divide babesia into four species that correspond to the simplest piroplasms: piroplasmosis, nuttalliosis, babesiosis and francaiellosis.
Babesia is an intracellular parasite that affects red blood cells. By dividing, microorganisms multiply in red blood cells. Thus, in acute forms of babesiosis, the infection of red blood cells is up to tens of percent, and asymptomatic forms of damage occur with minimal damage to blood cells. Today, about 100 species of Babesia are known, but few of them are human pathogens. The main pathogens of babesiosis in humans are: microti, divergens, bovis, odocoilei.
The main route of infection of humans with babesia is the transmission of parasitic microorganisms with saliva when a tick feeds. As a rule, people who come into contact with ticks get sick: agricultural workers, tourists, livestock breeders. The disease has a pronounced seasonality, which occurs from May to September and is due to the activity of carriers. Babesiosis caused by microti is most often found in the United States. The first case of the disease was recorded in 1969 and since then about a hundred cases of human infection have been recorded every year. In Europe, the main causative agent of babesiosis in humans is divergens.
Life cycle of babesia
The life cycle of babesia consists of a change of two hosts: intermediate - vertebrate (human, animal) and definitive - invertebrate, i.e. tick. People become infected due to tick bites, which leads to babesiosis. In this process, parasitic microorganisms go through several stages of development.
- Babesia trophozoites are single-celled microorganisms that feed on the contents of red blood cells, i.e. hemoglobin, and develop in blood cells. They reproduce by dividing, affecting more and more red blood cells.
- Some species of Babesia do not reproduce in red blood cells and are called gamonts. In this case, the parasite enters the gastrointestinal tract and turns into gametes. The fusion of two gametes forms a zygote, which in turn transforms into a kinet.
- The kinet reproduces by division and forms sporokines. After the parasitic mite, the sporozoites infect erythrocytes and turn into trophozoites. The life cycle of Babesia is repeated.
Pathogenesis of Babesia
The pathogenesis of babesia has not been studied sufficiently, but scientists know that parasitic microorganisms are transmitted through the bites of Ixodidae ticks, which are better known as Dermacentor, Hyalomma. The natural habitat of parasites are infected animals, with small rodents acting as an intermediate reservoir.
After a tick bite, the babesiosis pathogen penetrates into the erythrocytes and blood capillaries. Clinical manifestations of infection occur when the number of infected erythrocytes exceeds 3-5%. Due to the destruction of erythrocytes, waste products of parasitic microorganisms constantly enter the blood, which causes a strong pyrogenic reaction of the body and general toxic symptoms.
Due to increasing anemia, microcirculation disorders and pronounced tissue hypoxia begin. Free hemoglobin and erythrocyte cell membranes settle in the renal capillaries, which leads to acute renal failure and hematuria. If there is a massive release of erythrocytes, then pigment metabolism disorders develop, accompanied by the accumulation of indirect bilirubin in the blood.
Diseases that cause babesia
Diseases caused by babesia have a negative impact on the functioning of all organs and systems. In the international classification of diseases ICD-10, human babesiosis is under the code B60.0.
- Babesiosis affects people with reduced immune system defenses. The disease affects elderly people, patients with severe diseases that have undermined the immune system, and those who have undergone splenectomy.
- In most cases, parasitic microorganisms appear in people with the human immunodeficiency virus. If Babesia affects people with a well-functioning immune system, the disease is asymptomatic, even with parasitemia reaching 2%.
Babesiosis is an acute infectious disease that causes intoxication of the body, fever, anemia and is accompanied by a severe course. Babesiosis is a transmissible parasitic zoonotic infection. The disease causes jaundice and hemoglobinuria.
Babesia affects inhabitants of all continents except Antarctica. Due to the differences in scientists' opinions regarding babesia and insufficient study, babesiellosis is compared with piroplasmosis. But this is not correct, since the parasites have different etiologies and different clinical pictures of diseases.
Symptoms of Babesiosis
Symptoms of babesiosis depend on the type of babesia that caused the infection. If the parasite infects animals, the symptoms are accompanied by high body temperature, cardiovascular problems and rapid breathing. The animal quickly loses weight, suffers from constipation, which alternates with diarrhea. When cows are infected with Babesia, the animals produce yellow or reddish milk, which is bitter in taste. After a couple of days of illness, the animal develops bloody urine, the acute course of the disease lasts for 4-8 days. 40% of cases of infection of cattle are accompanied by a fatal outcome. With babesia in goats or sheep, a fatal outcome occurs in 80% of cases.
In humans, babesiosis develops against the background of a weakened immune system. The first cases of the disease were recorded in the second half of the 20th century. To date, the disease has not been sufficiently studied, so the diagnosis of babesiosis is difficult. The disease is accompanied by complications that cause acute renal failure, polyangiitis, and acute renal and hepatic failure. With babesiosis accompanied by pneumonia, serious complications are possible, which without proper treatment can lead to death.
Diagnosis of babesiosis
Diagnosis of babesiosis is difficult due to insufficient study of the parasitic microorganism. If the patient has severe fever accompanied by anemia and hepatomegaly, it is necessary to conduct laboratory tests for babesiosis. Of particular importance is the consideration of epidemiological indicators: tick and animal bites, long stay in endemic areas, weakened immune system.
To confirm the diagnosis of babesiosis, a blood test is taken from the patient and a reaction for indirect immunofluorescence is carried out. In diagnostics, a reaction for component binding is used. In case of low parasitemic indicators, a biological method is used for diagnostics, which consists of introducing the patient's blood to splenectomized animals. After a couple of weeks, the animals show the first signs of the disease, which allows the presence of Babesia to be detected in a blood smear. Particular attention is paid to the differential diagnosis of babesiosis with sepsis, HIV infections, blood lesions and other diseases.
Treatment of babesiosis
Treatment of babesiosis depends entirely on the effectiveness of diagnostics of the parasitic disease. In the treatment of babesiosis in animals, Berenil, Akaprin, Tiargen, Piroplasmil and a number of other drugs are used. In addition to drug treatment, sick animals are provided with complete rest and regular adequate nutrition.
In the treatment of babesiosis in humans, drug therapy is recommended. For these purposes, antibiotics and antiprotozoal agents, macrolides, lincosamides, antimalarial drugs, antimicrobial and antiparasitic pharmaceuticals are used. In severe forms of babesiosis, a combination of the following drugs is recommended: Quinine and Clindamycin or Atovaquone and Azithromycin. In particularly severe cases and in the acute course of Babesia, patients undergo blood transfusions.
Prevention of babesiosis
Prevention of babesiosis is not specific. Thus, in order to protect yourself from infection with babesia, it is recommended to take anti-tick drugs. Particular attention to drug prevention should be paid to people who graze farm animals or come into contact with stray animals.
Protection against babesiosis consists of destroying rodents and ticks in pastures, as well as specific treatment of animals with preparations that destroy ticks, i.e. acaricides.
Babesiosis prognosis
The prognosis of babesiosis depends on the severity of the parasitic disease and the individual characteristics of the patient's body. Thus, when animals become ill with babesia, without timely drug treatment, 80% of cases end in death. With early antiparasitic therapy, the prognosis for recovery is positive.
If babesiosis affects a person, it is necessary to understand that the parasite puts a heavy burden on the entire body and even after full therapy can cause serious complications and consequences. Intoxication caused by the action of the parasitic microorganism negatively affects the functioning of all organs and systems. Due to incorrect diagnosis and ineffective treatment, babesiosis has a negative prognosis, causes renal and cardiac failure, anemia, hepatitis and damage to the nervous system.
Babesia is a parasite that lives and develops in the cells of the circulatory system. The disease occurs in both animals and humans. Due to insufficient study of the harmful microorganism, the infection is difficult to diagnose and treat.


 [
[