Medical expert of the article
New publications
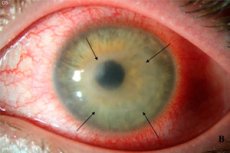
Acanthamoeba keratitis
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Among the many eye diseases, Acanthamoeba keratitis is not particularly common, although it does not have any particular gender or age selectivity. This serious disease, which affects the functionality of the cornea, is encountered mainly by people with problematic vision who use contact lenses. Therefore, it would be very useful to know what patients may encounter when choosing this method of vision correction, and how to avoid unpleasant consequences, without bringing the situation to the point of needing surgical treatment and blindness.
What does the diagnosis mean?
In the medical community, it is common to name inflammatory diseases identically, by adding the suffix "-itis" to the root of the word. When it comes to inflammation of the cornea of the eye, the diagnosis sounds like "keratitis". But the causes of inflammation can be different, so to specify them, phrases are used:
- if the cause was an eye injury - traumatic keratitis,
- in case of a viral nature of the disease – viral keratitis (in case of infection with the herpes virus – herpetic),
- in case of parasitic nature of the pathology – parasitic keratitis (acanthamoeba, onchocerciasis), etc.
There are also other types of keratitis caused by fungi, bacteria, and sunburn of the eyes (one of the types of traumatic form of the disease).
Acanthamoeba keratitis is one of the varieties of the parasitic form of the disease. Its causative agent is a protozoan called "acanthamoeba". When this small parasite gets into the eye and subsequently multiplies, a person begins to feel discomfort in the eye and see poorly both when wearing lenses and when removing them. And instead of correction, he gets a progressive deterioration in vision. And the reason here is not in the lenses themselves, but in their improper use. [ 1 ]
Epidemiology
Statistics confirm that swimming in open water bodies with direct contact of lenses with water is the leading cause of acanthamoeba keratitis. About 90-96% of cases of detection of the disease belong to this category. Moreover, the probability of corneal inflammation is much higher when using soft contact lenses.
Previous studies have estimated the incidence to be 1.2 per million adults and 0.2 (US) to 2 (UK) per 10,000 soft contact lens wearers per year.[ 2 ] Parmar et al. suggested that the incidence may be tenfold higher.[ 3 ] A sharp increase in the incidence of acanthamoeba keratitis was observed in the 1980s, largely due to the increased availability of soft contact lenses and the use of non-sterile contact lens solutions.[ 4 ] Additional outbreaks in the late 1990s and 2000s have been reported in the US and in Europe and have been epidemiologically linked to a number of possible sources, including municipal water supply contamination,[ 5 ] regional flooding,[ 6 ] and the use of widely available multipurpose contact lens disinfectant solution.[ 7 ],[ 8 ]
As a survey of patients showed, most of those who fell ill swam in open water bodies (rivers, lakes, ponds, the sea). Apparently, water disinfection does reduce the number of bacteria and protozoa, leaving only microorganisms in the cyst stage unaffected. It is the latter that enter the body with tap water. And in a suitable environment, cysts pass into the vegetative stage.
Other routes of infection with the single-celled parasite are not so relevant. For example, infection with Acanthamoeba after surgery or trauma is much less common (approximately 4% of cases).
The eye is a very sensitive structure. It is not surprising that even the smallest speck of dust or eyelash in the eye seems to be a big nuisance and causes very unpleasant sensations. Even the softest lenses, especially if used carelessly or incorrectly, can become a traumatic factor for the cornea. Rubbing its surface and scratching it with stuck microparticles (when using solutions that do not clean lenses well), they facilitate the penetration of infection deep inside, and tightly adhering to the eye, they provide ideal contact between the cornea and pathogens that accumulate on the lens after interaction with an infected environment (in particular, with water). Acanthamoeba is, as it were, “locked” in ideal conditions of existence, where it subsequently parasitizes.
As for the epidemiological situation, it has improved significantly over the past half-century. Doctors first encountered an outbreak of the disease in 1973, when inflammation bypassed only 10% of patients using contact lenses. Nowadays, keratitis is rarely diagnosed (4.2% of patients among those diagnosed with inflammatory eye diseases), but most patients come to see doctors because of wearing lenses.
Thanks to a thorough study of the causes of the disease and the development of effective measures to prevent keratitis, doctors have managed to reduce the incidence. But despite the comforting statistics on keratitis, we should not forget that inflammatory eye diseases are associated with about 50% of hospitalizations and 30% of cases of vision loss.
Causes acanthamoeba keratitis.
Given the ability of Acanthamoeba to survive even in adverse conditions, it is safe to say that this microorganism is part of our normal environment. It is not surprising that we encounter it everywhere. But why then does the disease not develop widely?
And the reason is that nature has taken care of the natural protection of the eyes. It is not so easy for microorganisms to penetrate the cornea, so they are usually just transit passengers in the eye. But some negative factors can help the parasite penetrate the structures of the eye, where it can stay longer and acquire offspring, simultaneously destroying the tissues of the cornea. Such factors include:
- incorrect use of contact lenses,
- eye injuries,
- corneal scratches or any other violation of its integrity, including surgical procedures and postoperative care.
Acanthamoeba does not need a host to exist, but this does not mean that it cannot harm the organs of vision, which are an ideal nutrient medium, containing substances of organic origin. [ 9 ]
Acanthamoeba keratitis is an inflammation of the cornea caused by Acanthamoeba, which has penetrated deep into the eye tissue or multiplies in the ideal environment created for it by contact lenses. It is not surprising that most patients with this diagnosis actively use lenses in everyday life. And, as is usually the case, they do not always manage to adhere to the rules for using and caring for contact lenses. Moreover, the disease can affect one or both eyes.
Ophthalmologists consider the following risk factors for infection of the eyes with Acanthamoeba and the development of an inflammatory process in the cornea:
- swimming with contact lenses, especially in natural bodies of water,
- Improper lens care:
- rinsing with running water,
- using tap water or non-sterile solutions to store lenses,
- improper or lack of disinfection of lenses,
- inadequate care (cleaning and disinfection) of the lens storage container,
- saving solutions for storing lenses (reuse, adding fresh solution to used one),
- failure to observe hand and eye hygiene when using contact lenses.
Although the last point seems to be the most likely factor of infection, it is more dangerous as one of the causes of bacterial keratitis. Acanthamoeba keratitis most often occurs when in contact with water, i.e. as a result of swimming without removing contact lenses, or handling lenses with wet hands. Thus, in natural water bodies it is very difficult to maintain the necessary hand hygiene when removing or installing contact lenses, in addition, there are not always conditions for storing them, so swimmers prefer not to remove them. But this is a double-edged sword: caring for the preservation of the properties of the lenses can be detrimental to the eyes.
The literature has established that contact lens wear is the strongest risk factor for the development of acanthamoeba keratitis, with an association between the disease and contact lenses reported in 75–85% of cases. [ 10 ]
A correlation with herpes simplex keratitis has been previously reported,[ 11 ],[ 12 ]: approximately 17% of AK cases demonstrate a history of ocular HSV disease or active HSV coinfection.
Pathogenesis
The pathogenesis of acanthamoeba keratitis involves parasite-mediated cytolysis and phagocytosis of corneal epithelium, as well as invasion and dissolution of corneal stroma.[ 13 ]
The disease is classified as infectious and inflammatory, since the development of the pathological process is associated with a parasitic infection. The causative agent of the disease (acanthamoeba) is a single-celled parasite, whose usual habitat is water. It is usually found in natural reservoirs, from where the parasite also gets into tap water. But this does not mean that the water in an artificial reservoir (pond or even a swimming pool) can be considered absolutely safe, here you can also find acanthamoeba, as well as in the soil moistened with the same water.
The genus Acanthamoeba includes several types of free-living amoebas, 6 of which are dangerous to humans. These are aerobes that live in soil and water, especially that which is contaminated with sewage. They can also be found in dust, where they get after water bodies or soil dry up. In this case, the microorganisms simply go into a low-activity stage (cysts), when they are not afraid of either temperature changes or disinfection procedures.
Acanthamoebas thrive in tap water and sewage, in liquid circulating in the heating and hot water supply system. High water temperatures only promote the reproduction of microorganisms.
Water containing microorganisms can get into the eyes during bathing, washing, contact with the eyes of wet or dirty hands. But the very contact of water or soil contaminated with parasites with the eyes does not cause disease. Moreover, acanthamoeba can be found in healthy people (in the nasopharynx and feces).
Our eye is designed in such a way that the lacrimal glands present in it facilitate physiological moistening and cleansing of the cornea. Dust and microorganisms that get on it are removed through the drainage system of the lacrimal apparatus into the nasopharynx, from where they are excreted together with mucus. The parasite simply does not have time to "settle" in the eye and begin to actively reproduce.
If there is a disruption of the drainage function, Acanthamoeba not only settles comfortably in an ideal environment (warm and humid), but also begins to actively multiply, causing diffuse inflammation of the cornea.
Symptoms acanthamoeba keratitis.
Acanthamoeba keratitis is an inflammatory eye disease that is not without the symptoms inherent to this process: redness of the eyes, a sensation of a foreign body and associated discomfort in the eye, pain (a frequent companion of inflammation), which intensifies when removing contact lenses. They can be considered the first signs of inflammation of the cornea, although many other eye diseases, including a speck in the eye, have the same symptoms. Then patients may complain of causeless tears that flow against the will of a person, pain in the eyes, deterioration in the clarity of vision (as if there is a film in front of the eyes). [ 14 ]
All these symptoms are similar to the sensations when a small speck of dust gets into the eye, but in this case you won’t be able to “blink”. The clinical picture is notably persistent, but as the inflammation develops, the symptoms of acanthamoeba keratitis tend to intensify. At first, only discomfort behind the eyelid is felt, then soreness and, finally, sharp cutting pains like an open wound, provoking and intensifying lacrimation.
But it should be noted that the sudden onset of the disease or rapid progression of inflammation is observed in no more than 10% of patients. In the rest, the disease is characterized by a slow, but not mild course.
Regardless of the cause of inflammation, keratitis manifests itself with a specific symptom complex, which doctors call corneal syndrome. It is characterized by:
- sharp, severe pain in the eye,
- increased lacrimation,
- spasmodic contraction of the orbicularis oculi muscle, which leads to involuntary closing of the eye (blepharospasm),
- painful reaction of the eyes to bright light (photophobia).
This syndrome is specific and helps differentiate corneal inflammation from conjunctivitis before testing for the causative agent of inflammation.
In advanced stages, if the inflammation was not treated or was inadequate, one may notice clouding of the cornea (impaired transparency is one of the characteristic signs of keratitis), the formation of a light spot (leukoma) on it, a noticeable deterioration in vision up to blindness. In some cases, a purulent ulcer forms on the cornea, which indicates the penetration of infection into the deep tissues of the eye.
Complications and consequences
Let us repeat once again that the tissues of the visual organ are highly sensitive, which is why they react so sharply to any negative conditions. This complex optical structure turns out to be very delicate and susceptible to degenerative changes. Inflammation that occurs in the cornea is difficult to treat, while a long-term inflammatory process can easily change the properties and functionality of the organ.
Acanthamoeba keratitis is a disease with pronounced unpleasant symptoms that cause significant discomfort and worsen the patient's quality of life. Is it easy for you to do your previous job if a speck of dust flies into your eye and irritates it? All thoughts immediately switch to how to remove it. But with inflammation of the cornea, such a speck is an amoeba, which is no longer so easy to remove from the eye, so painful symptoms torment a person constantly, sometimes weakening somewhat, then falling with renewed vigor.
It is clear that such a state of affairs will affect a person's ability to work and their mental state. Pain-related attention deficit combined with deteriorating vision can become an obstacle to fulfilling their work obligations. Spontaneous eye closure and poor vision increase the risk of domestic and industrial injuries.
These are the consequences of keratitis of any etiology, if the patient does not seek professional help or self-medicates without understanding the cause and mechanism of the disease. But there are also complications that can arise both in the absence of treatment and with the incorrect selection of effective therapeutic methods, which often results from incorrect diagnostics. After all, keratitis of various etiologies require their own, unique approach to treatment.
The most common complication of the inflammatory process in the cornea is its clouding. Long-term inflammation causes cicatricial changes in the tissues of the eye and it is not always possible to achieve their complete resorption. In some cases, changes in the transparency of the cornea progress with the formation of a local light spot (leukoma) or a general decrease in vision in one eye, up to complete blindness in the future. [ 15 ]
Any inflammation is a breeding ground for a bacterial infection, which can easily join a parasitic one. In this case, the inflammation can also affect the deepest structures of the eye, causing the development of purulent inflammation of the inner membranes of the eyeball (endophthalmitis), as well as inflammation of all membranes and media of the eye (panophthalmitis).
Against the background of reduced immunity, the addition of a herpes virus infection is not uncommon.
The deeper the inflammation, the more severe the consequences can be expected. It is not always possible to preserve vision and the aesthetic appearance of the eye, quite often the disease recurs after seemingly effective therapy, so doctors sometimes resort to surgical treatment, which consists of replacing (transplanting) the cornea.
Acanthamoeba keratitis, like any inflammation of the cornea, has 5 degrees of severity (stages):
- superficial epithelial lesion,
- superficial punctate keratitis,
- stromal annular,
- ulcerative (with the formation of wounds on the cornea)
- scleritis (inflammation extends to the sclera)
The first 2 stages are treated with medication. But the treatment does not always give good results. As the disease progresses, surgical treatment is indicated in combination with medication.
Diagnostics acanthamoeba keratitis.
Discomfort and pain in the eye sooner or later force patients to seek help from specialists. And then it turns out that the cause of pain and deterioration of vision was not contact lenses and dust sticking to them, but protozoa that once settled in the tissues of the eye due to human carelessness. But it is difficult for a doctor to tell by the patient's appearance what is causing the redness of the eyes, pain and tearfulness, because these symptoms are also present in other diseases. Redness and pain in the eyes in combination with photophobia are noted even with the flu, not to mention eye diseases. [ 16 ]
Only a specialist (ophthalmologist), to whom the patient is referred, can make an accurate diagnosis. For this doctor, the very fact of corneal opacity caused by the accumulation of leukocytes, lymphocytes and other small cellular elements, the level of which increases during inflammation, will be an indicator of the inflammatory process.
But clouding of this part of the eye can also be caused by degenerative-dystrophic changes, so it is important for the doctor to determine whether there is inflammation and what it is associated with. A thorough description of the patient's symptoms and anamnesis will help him in this: does the patient wear contact lenses, how does he care for them, does he take them off while swimming, has there been any previous eye injuries, etc.
Instrumental diagnostics of acanthamoeba keratitis usually comes down to one main method – biomicroscopy of the eye, which is a contactless study of various structures of the eye using special equipment. During the study, a microscope and various types of illumination are used, which help to visualize even those structures of the complex optical system of the eye that are not visible under normal lighting. [ 17 ]
Ultrasound biomicroscopy (contact with anesthetic and non-contact method) is increasingly used in modern clinics. In any case, the doctor receives reliable information about the various structures of the eye, their condition, the presence of inflammation, its nature and prevalence. Biomicroscopy allows you to detect the disease even in the early stages, when the symptoms are not yet expressed.
But identifying corneal inflammation is only half the battle. It is important to determine the cause of the disease. And this is where problems often arise. Differential diagnostics of bacterial, viral, allergic, fungal and other types of keratitis is quite difficult. There is a high risk of making an inadequate diagnosis.
Specific tests help to determine the cause of the disease or exclude its various variants. A blood test will help to identify inflammation, but nothing more. However, microbiological studies can provide an answer about the causative agent of the disease. For this purpose, the following is carried out:
- bacteriological examination of material taken during scraping from the cornea (most often using the polymerase chain reaction (PCR) method, [ 18 ], [ 19 ]
- cytological examination of the epithelium of the conjunctiva and cornea,
- allergy tests with different antigens,
- serological studies based on the interaction of antigens and antibodies.
But the problem is that the diagnosis of "acanthamoeba keratitis" is often made based on the absence of signs of other pathogens, and not on the presence of cysts and active acanthamoeba individuals. Laboratory tests do not always provide an accurate answer as to whether there are protozoa in the eye tissues or not.
Recently, a specific method of confocal laser scanning microscopy, which has excellent contrast and spatial resolution, has become increasingly popular. It makes it possible to identify the pathogen and its cysts in any of the corneal layers, to determine the depth and extent of the eye lesion. This allows for a diagnosis to be made with maximum accuracy, excluding diseases with similar symptoms.
Treatment acanthamoeba keratitis.
Since the inflammatory process in the eye structures can be caused by various reasons, the doctor can prescribe effective treatment only after making sure that the diagnosis is correct. But often diagnostic errors are discovered after some time, when the prescribed course (most often antibiotic therapy due to suspected bacterial nature of the disease) does not give results. The drugs used must be effective against protozoa, and not just bacteria, i.e. the selection of antibiotics and antiseptics should not be random, as with conjunctivitis.
By the way, this problem often occurs during self-medication, because people's knowledge of eye diseases is limited, so patients attribute all symptoms to conjunctivitis, without taking into account the pathogen. This means that they try to treat it with medications that were once prescribed for conjunctivitis. Often this only worsens the situation, because time is not in the patient's favor. In addition, patients often continue to wear contact lenses, which is not allowed.
Thus, therapy for acanthamoeba keratitis begins with an accurate diagnosis and the refusal to wear contact lenses at least for the duration of treatment. Mild forms of the disease, detected at an early stage, are treated on an outpatient basis. Inpatient treatment is indicated for severe and complicated forms of keratitis. In these cases, the possibility of surgical treatment is also considered (layered superficial and deep keratoplasty, penetrating keratoplasty, phototherapeutic keratectomy).
In mild cases, medication is used to destroy the pathogen (Acanthamoeba and its cysts) and restore corneal tissue. For these purposes, eye drops, ointments, instillations of drugs and medicinal films containing antibacterial (antiprotozoal), anti-inflammatory, and sometimes antiviral (if a herpes infection occurs) components are used.
To combat the pathogen, a combination of antibiotics and antiseptics is used, since there is currently no specific monodrug active against Acanthamoeba. Most often, a combination of chlorhexidine (in the form of instillations) and polyhexamethylene biguanide (included in the Opti-Free contact lens care solution, which is used for eye instillation, and Comfort-Drops moisturizing eye drops) is used. This complex is effective against both active forms of amoeba and its cysts. Biguanides are the only effective therapy for the resistant encysted form of the organism in vitro and in vivo. The use of modern steroids is controversial, but probably effective, for the treatment of severe inflammatory complications of the cornea that were not effective when treated with biguanides. Acanthamoeba-associated scleritis is rarely associated with extracorneal invasion and is usually treated with systemic anti-inflammatory drugs in combination with topical biguanides. Therapeutic keratoplasty may be used in the treatment of some severe complications of Acanthamoeba keratitis.[ 20 ]
In more severe cases, with complicated course of the disease and in the absence of effect from specific therapy, the following drugs are additionally prescribed:
- antiseptic drops "Vitabact" based on picloxidine or "Okomistin" based on miramistin,
- diamedins (propamidine is a substance with pronounced bactericidal and antiprotozoal action, included in imported eye drops, for example, the drug "Brolene"),
- antibiotics from the aminoglycoside group (neomycin, gentamicin) and fluoroquinolones (there is information about the high efficiency of the antimicrobial drug from the fluoroquinolone group based on moxifloxacin "Vigamox" in the form of eye drops),
- polypeptide antibiotics (polymyxin),
- mycostatics (fluconazole, intraconazole),
- iodine preparations (povidone-iodine),
- anti-inflammatory drugs:
- NSAIDs (for example, Indocollyre drops based on indomethacin - relieves pain and inflammation) are prescribed rarely and for a short course,
- corticosteroids, such as dexamethasone, are used mainly after surgery or in the non-acute period of the disease, since they can provoke activation of the disease; antiglaucoma drugs are prescribed in combination with them (for example, "Arutimol", which normalizes intraocular pressure),
- mydriatics (these drugs are prescribed both for diagnostic purposes to dilate the pupil and for treatment of inflammatory eye diseases),
- preparations with a regenerating effect (Korneregel, Lipoflavon, Tauforin),
- artificial tear installations,
- vitamins, biogenic stimulants.
Reduced visual acuity is also treated with the help of physiotherapeutic procedures: electrophoresis, phonophoresis with enzymes, ozone therapy, VLOC.
There are different approaches to the treatment of acanthamoeba keratitis, drugs and treatment regimens are prescribed individually, based on the diagnosis, stage and severity of the disease, the presence of complications, the effectiveness of the therapy, etc.
Medicines
Experience shows that conventional broad-spectrum antibiotics are effective in complicated cases of acanthamoeba keratitis, but they do not have a detrimental effect on acanthamoeba. Antiseptics, especially chlorhexidine, and a disinfectant included in eye drops and contact lens care solutions have a more pronounced bactericidal effect. Using the Opti-Free solution, you can avoid a disease that is dangerous for the eyes. [ 21 ]
As for antiseptics, the drug "Okomistin" in the form of eye drops has become widely used in the treatment of inflammatory eye diseases. Its active ingredient - miramistin - is active against a large number of bacteria, fungi, protozoa, and it also increases the sensitivity of pathogens to stronger antimicrobial agents.
For the treatment of keratitis, Okomistin is used in combination with antiprotozoal agents and antibiotics. The drug is prescribed to adults and children 4-6 times a day. It is instilled into the conjunctival sac of the eye 1-2 (for children) and 2-3 (for adults) drops for a course of no more than 14 days.
The medicine is also used in the postoperative period: 1-2 drops three times a day for up to 5 days, and also to prepare for surgery (2-3 drops three times a day for 2-3 days).
The only contraindication to the use of the antiseptic is hypersensitivity to its composition.
The use of the drug is rarely accompanied by discomfort (a slight burning sensation that goes away within a few seconds). This side effect is not dangerous and is not a reason to stop therapy. But hypersensitivity reactions require discontinuing the drug and revising the treatment.
"Okomistin" is often used in combination with local antibiotics.
No less popular in the treatment of acanthamoeba keratitis is the antiseptic "Vitabact" based on picloxidine - a biguanide derivative considered active against a large number of infections, including protozoan ones.
The medicine is available in the form of eye drops. It is usually prescribed 1 drop 3-4 times a day (up to 6 times) for a ten-day course. Before eye surgery, it is also recommended to inject 2 drops of the solution into the conjunctival sac.
The drug is not prescribed in case of intolerance to its components, hypersensitivity to biguanides. During lactation, it is better not to breastfeed the child during the period of using the drug. It is also undesirable to use the drug during pregnancy.
When instilling the solution into the eyes, a burning sensation may be felt, local hyperemia is noted, which does not require treatment.
Brolene eye drops with propamidine are a good alternative to combined treatment with Comfort Drops and chlorhexidine or another antiseptic. Propamidine reduces the activity of pathogens, inhibits their reproduction, so they are easier to remove from the eye using instillations.
The solution is administered into the eye 1-2 drops up to 4 times a day.
The drops are not recommended for use by pregnant and nursing women, as well as patients with hypersensitivity to the components of the drug.
The use of the drug is painless, but blurred vision may be felt for some time. During this period, it is better to refrain from performing potentially dangerous actions. If vision becomes worse or the symptoms of the disease worsen, you should consult a doctor.
"Indocollyre" is a non-hormonal drug with anti-inflammatory and analgesic effects. It is prescribed mainly after eye surgeries, but can also be used in complex drug treatment without surgery.
The medicine is prescribed 1 drop 3-4 times a day, including the day before the operation (this reduces the risk of complications).
The drug is relevant for severe pain syndrome. But it has a number of serious contraindications: hypersensitivity to the drug, a history of "aspirin" asthma, gastric ulcer and duodenal ulcer, severe liver and kidney pathologies, the second half of pregnancy, breastfeeding. The drug is not used in pediatrics.
"Indocollyre" belongs to the category of NSAIDs, which, due to their effect on the blood, inhibit regenerative processes in the cornea, therefore it is not recommended to use it for a long time or without a doctor's prescription.
The use of the drug may cause side effects on the eyes: redness, itching, slight burning, temporary deterioration of visual acuity, increased sensitivity to light. However, such complaints from patients are rare.
"Korneregel" is an ophthalmic preparation in the form of a gel based on dexpanthenol. It promotes the regeneration of the mucous membranes of the eye and the skin around them, easily penetrating deep into the tissues. It is actively used in the complex therapy of keratitis of various etiologies.
The gel is applied locally, taking into account the severity of the disease. Start with 1 drop 4 times a day plus 1 drop before bedtime. Place the gel in the conjunctival sac.
The duration of treatment is strictly individual and is determined by the doctor depending on the observed therapeutic effect. It is advisable not to use the drug often and for a long time due to the preservative contained in the gel, which causes irritation and even damage to the mucous membrane. When used in combination with other eye drops, gels, ointments, the interval between drug use should be at least 15 minutes.
Among the contraindications for the use of "Korneregel" the only one listed is hypersensitivity to dexpanthenol or any other component of the drug.
Side effects include mainly hypersensitivity reactions accompanied by itching, redness, rashes on the skin, and eye symptoms. The latter include redness, burning, foreign body sensation, pain, lacrimation, and swelling.
"Lipoflavon" is a wound healing and regenerating agent based on quercetin and lecithin. It has antioxidant properties, is effective against viruses, inhibits the production of inflammation mediators, and improves the trophism of eye tissues.
The drug is available as a powder in a bottle, which comes with a sterile bottle with 0.9% sodium chloride solution (saline) and a dropper cap. It is used for instillations in keratitis of various etiologies in the form of eye drops, as well as in the postoperative period. The drug reduces the risk of keratitis as a result of damage to the cornea during surgical interventions.
When used in ophthalmology, saline solution is added to the bottle with powder, shaken well until completely dissolved and a dropper cap is put on. The medicine is dripped into the conjunctival sac 1-2 drops up to 8 times a day. The number of drops is halved when the inflammation subsides. The course of treatment usually lasts from 10 to 30 days.
The drug has contraindications: hypersensitivity to the composition, allergic reactions to protein and vaccines in the anamnesis, alcohol consumption. During pregnancy and lactation, "Lipoflavon" is used only with the permission of a doctor due to the lack of data on the effect of the drug on the fetus and the course of pregnancy. In pediatrics, it is used from the age of 12.
Among the side effects with local application, only allergic reactions are possible (itching, skin rashes, fever).
Since the eye is a very sensitive organ, it is not recommended to use any of the drugs without a doctor's prescription. If the doctor prescribes drops for both eyes, even if only one is affected, his prescription must be followed, since there is a high probability of transmitting the infection, activating the virus living in the body, etc.
A new treatment option may be the use of alkylphosphocholines. These are phosphocholines esterified to aliphatic alcohols. They exhibit antitumor activity in vitro and in vivo and have been shown to be cytotoxic against Leishmania species, Trypanosoma cruzi, and Entamoeba histolytica. A recent study has shown that hexadecylphosphocholine (miltefosine) in particular is also very effective against various strains of Acanthamoeba. [ 22 ], [ 23 ]
Folk remedies
Doctors consider acanthamoeba keratitis a serious eye disease, because with the wrong approach to treatment, the disease can progress and lead to blindness. Traditional methods of treating corneal inflammation do not replace traditional drug therapy, but can only complement it, removing painful symptoms. In addition, given the fact that our eye is a delicate structure, it is highly inadvisable to instill questionable solutions into it. Any prescription should be discussed with a doctor in advance.
Plants and products used in folk medicine are not able to destroy the pathogen, but they can reduce pain and discomfort, relieve increased sensitivity to light, relieve redness and swelling of the eyes, and help restore damaged tissue. But the proposed recipes must be used consciously, carefully assessing the possible risks.
What do folk healers offer us for keratitis?
- Sea buckthorn oil. This is an excellent source of vitamins for the eyes, which also has a regenerative effect. It is better to take sterile oil, it is sold in pharmacies. Drip 2 drops into the sore eye. The interval between procedures is from 1 to 3 hours.
The product reduces pain, relieves photophobia, and promotes corneal tissue restoration. But don't expect miracles from it. The oil is neutral in relation to the pathogen, so antiprotozoal and antiseptic agents should be used in parallel with it.
- Water extract of propolis (1 part) and celandine juice (3 parts). The composition is used in the form of eye drops for bacterial complications of keratitis. The recommended dose is 2 drops in the eye at night.
- Clay. Used for poultices, relieves pain. Wet clay is placed on a napkin in a layer of about 2-3 cm. The bandage is applied to the eyes for an hour and a half.
- Liquid honey. Mix one part of May honey with 3 parts of warm water and stir until the liquid becomes clear. Use the product for eye drops or eye wash 2 times a day.
Honey is a strong allergen, so if you are allergic to bee products, such treatment can only increase inflammation.
- Aloe. The juice of this plant has remarkable regenerative properties and is an excellent antiseptic. Its use will help prevent bacterial and viral complications of keratitis. At the beginning of the disease, aloe juice is used by adding a few drops of mumiyo, and then in pure form (1 drop per eye).
Herbal treatment is also used in cases of keratitis, which helps to increase the effectiveness of drug therapy and prevent complications.
The herb eyebright has a beneficial effect on the eyes. It is used to make a liquid medicine that is used internally and for eye drops. To prepare an infusion for internal use, take 3 tablespoons of chopped herb per half a liter of boiling water and leave in a warm place for at least 6 hours. Treatment is carried out three times a day, taking ½ a glass of infusion.
Eye drops are prepared by taking 1 teaspoon of the herb per glass (200 ml) of water. The mixture is boiled for 3 minutes, then removed from the heat and infused for another 3 hours. The strained decoction is used to instill the eyes (2-3 drops) before bedtime.
For compresses and lotions, decoctions of sweet clover flowers (20 g of herb per 1/2 cup of water, boil for 15 minutes) and calendula (1 teaspoon per 1 cup of water, boil for 5 minutes) are used, which have antimicrobial and anti-inflammatory effects. A compress from a sweet clover decoction is left on for half an hour, and a lotion from calendula is left on for 10-15 minutes. The procedure is carried out twice a day. Treatment is carried out until the symptoms of the disease disappear.
It is useful to use chamomile infusion for washing eyes. Since the use of anti-inflammatory drugs for acanthamoeba keratitis is limited, chamomile turns out to be a real find, because it does not cause unwanted side effects.
To prepare the infusion, take 2 tablespoons of dried flowers and pour 2 cups of boiling water over them. The medicine is infused for 15-20 minutes or until it cools completely under the lid.
Eye washes can be done 3-4 times a day. Additionally, the infusion can be used for lotions.
When preparing eye drops and eye washes at home, remember about sterility. It is better to use purified water, boil the dishes thoroughly. Eye drops devices should also be sterile: droppers, pipettes. Otherwise, it is easy to introduce a bacterial infection into the acanthamoeba infection.
When instilling drops into the eyes, you need to try to ensure that the dropper does not touch the eye tissue. When rinsing the eyes, it is important to use a separate bandage or cotton pad for each eye, changing them as often as possible during the procedure.
Homeopathy
In the case of a disease such as acanthamoeba keratitis, even treatment with folk remedies may seem questionable, not to mention homeopathy. However, homeopaths insist on the beneficial effect of some drugs of this kind. And it must be said that their arguments are very convincing.
Acanthamoeba infection is one of the types of infectious process. The causative agent of the disease is considered to be a protozoan infection, namely Acanthamoeba. If we go the traditional way, then identifying the causative agent of the disease using laboratory tests can be considered a long process. Analysis of corneal epithelium and tear fluid samples by PCR allows us to isolate amoeba DNA even with their minimal content, but this takes a lot of time.
Staining scrapings with different methods does not always give accurate results, which require professional interpretation. The histochemical method is relevant at more severe stages of the disease, but at first it can give a negative result and cysts can only be detected by biopsy.
The confocal microscopy method shows the fastest way to obtain an up-to-date result, but it is not yet used in all clinics. So in most cases, several days or even weeks are needed to clarify the diagnosis and begin effective treatment.
All this time, the inflammation will progress, which negatively affects the functionality of the cornea. Homeopaths offer a good solution - to begin treatment with anti-inflammatory and regenerating agents immediately after the patient consults a doctor. At the same time, the homeopathic remedies used, unlike corticoids and NSAIDs, will not potentiate or aggravate the inflammation.
Among homeopathic remedies used for any type of keratitis, a special role is given to Mercurius corrosivus, often prescribed for sharp tearing pain in the eyes at night, photophobia, and the appearance of deep ulcers on the cornea.
For burning pain in the eyes and profuse discharge, homeopathic remedies such as Mercurius solubilis (relevant in the initial stages of the disease), Pulsatilla, Bryonia, Belladonna, Aurum, Arsenicum album, Apis, Aconitum, etc. have proven themselves to be effective.
For ulcerations, homeopaths also prescribe Hepar sulphur, Kali bichromicum, Kali iodatum, Conium, Rhus toxicodendron, Syphilinum, Calcarea. For chronic keratitis and severe corneal opacity, Sulphur.
Many of the listed drugs help relieve pain and cope with increased sensitivity of the eyes to light. Almost all of them are prescribed in small dilutions.
The drugs are prescribed orally, 3-6 granules under the tongue 20-30 minutes before meals several times a day. Moreover, we are not talking about monotherapy, but about the use of homeopathic drugs in parallel with classical medications prescribed for keratitis, with the exception of antibiotics. The latter make sense to prescribe when the causative agent of the disease is identified.
Homeopaths today are actively searching for effective complex remedies for the treatment of keratitis (before the introduction of antibiotics and in combination with them). One of the innovative developments is considered to be a preparation based on the following components: Mercurius corrosivus, Belladonna, Apis, Silicea (all of them have the same dilution C3). Conium can also be added to it.
Both versions of the drug reduce pain during the first 2 hours. Also, the sensitivity of the eyes to light and lacrimation decrease. The symptoms are practically not felt the next day.
The developers of the drug, which does not yet have a name, claim that this complex medicine is universal, does not cause allergic reactions, does not enter into dangerous interactions with medications, has no side effects and age restrictions. It can be prescribed by both homeopaths and doctors who do not have special training.
It is clear that it is impossible to cure acanthamoeba keratitis with its help, but the medicine can alleviate the patient’s condition and somewhat slow down the pathological process while the diagnosis is being clarified and the disease is being treated.
Prevention
Any serious disease is easier to prevent than to treat, especially when it comes to parasites, against which there are virtually no effective drugs. But there are certain difficulties here too. The fact is that acanthamoeba cysts are resistant to disinfection. They can be destroyed by chlorinating water, but the concentration of chlorine in this case will be much higher than the permissible norms. So, as they say, a drowning man must save himself."
But acanthamoebas are also scary because, according to the latest research by scientists, they can become carriers of a bacterial infection, which is protected from disinfectants inside the parasite.
However, acanthamoeba keratitis is a fairly rare disease today, which means that protecting your eyes from amoebas and avoiding vision loss is not that difficult. Among the most effective preventive measures are:
- Proper care of contact lenses, use of high-quality sterile solutions for their storage, use of only licensed lenses.
- Maintaining hand hygiene when handling lenses in the eye area, eye hygiene.
- When taking a shower, washing, or swimming in any water environment, contact lenses must be removed and placed in specialized solutions. If water gets into your eyes, it is better to rinse them with a solution such as Opti-Free or Comfort-Drops. Such care for your eyes can reduce the likelihood of infection with Acanthamoeba.
- It is recommended to replace the contact lens container every 3 months.
- It is necessary to visit an ophthalmologist regularly (at least once every six months), even if there seems to be no reason for this. If the patient feels discomfort, burning, pain in the eyes, it is definitely not worth postponing a visit to the ophthalmologist.
Acanthamoeba keratitis is a dangerous disease that can deprive a person of sight, i.e. that valuable functionality thanks to which we perceive the largest part of information about the surrounding world. Such a disease cannot be treated carelessly, putting off a visit to the doctor for later. Timely diagnosis and treatment, as well as prevention, can preserve eye health and the happiness of seeing the world with your own eyes.
Forecast
Doctors agree that acanthamoeba keratitis is one of the most dangerous and insidious eye diseases. This disease is difficult to treat, and traditional antibiotics are often ineffective. If drug treatment of this slowly progressing pathology is ineffective, phototherapeutic keratectomy is considered the most optimal treatment method. If there is deep damage to the cornea, keratoplasty cannot be avoided to save the eye. [ 24 ]
The prognosis of surgical intervention largely depends on the depth of the corneal lesion and the age of the patient.
Acanthamoeba keratitis, if not effectively treated, becomes chronic with periods of remission and exacerbation (depending on the life cycle of the protozoa). The cornea gradually becomes pale, ulcers appear on it, attracting bacterial infection, and vision deteriorates. With severe perforation of the cornea, underlying structures may be involved in the process, which is an indication for eye removal (enucleation).
In general, the prognosis for acanthamoeba keratitis depends on several factors:
- Timeliness of diagnosis and correctness of diagnosis,
- Adequacy of the treatment provided,
- Timing of surgical procedures,
- Efficacy of subsequent treatment with corticoids and immunosuppressants.
There is an opinion that at the stage of diagnosis, acanthamoeba keratitis should be suspected in all patients using contact lenses. This is especially true if the inflammation is intermittent in nature with pronounced periods of exacerbation and remission.

