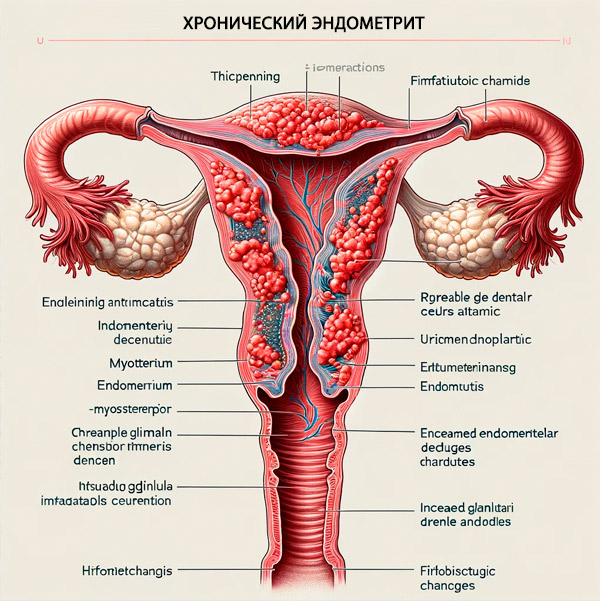
Chronic endometritis
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Protracted inflammation of the inner mucous membrane of the uterus, the endometrium, is defined as chronic endometritis.
Epidemiology
In advanced cervical inflammation (cervicitis), chronic endometritis is detected by endometrial biopsy in nearly 40% of women; concomitant endometritis may occur in 70-90% of reported cases of fallopian (fallopian) tube inflammation.
According to clinical statistics, chronic endometritis occurs in 3-10% of women who undergo endometrial biopsy for abnormal uterine bleeding; patients with gonococcal or chlamydial infections have chronic endometritis in 2735% of cases.Studies have shown that the prevalence of chronic endometritis is approximately 10% to 11% based on biopsies of patients who have undergone hysterectomy due to benign gynecologic disease. [1], [2]
The prevalence of chronic endometrial inflammation in infertile women is estimated to be 45%; in women with habitual spontaneous abortion, 60%; in women who have had repeat abortions, 68%; and in women with recurrent IVF (In vitro fertilization ) failure, 42%. [3], [4]
After a cesarean section - compared to a vaginal delivery - this disease occurs 15 times more often.
Causes of the chronic endometritis
The main causes of most inflammatory uterine diseases, including acute or chronic endometritis, are infection. In chronic endometritis, infectious lesions of the uterine mucosa can be caused by group A and B streptococci, bacteria of the genus Staphylococcus; Escherichia coli, Chlamydia trachomatis, Neisseria gonorrhoeae, Mycobacterium tuberculosis, Mycoplasma genitalium and Ureaplasma urealyticum; protozoal infection - flagellated protozoa Trichomonas vaginalis (trichomonads), intracellular parasites Toxoplasma gondii (toxoplasma), and Herpes simplex virus.
Gynecologists attribute pelvic inflammatory diseases in women to ascending infection of the female genital tract caused by the spread of bacteria - vaginal and endocervical contamination in STDs (sexually transmitted diseases), bacterial vaginosis or colpitis, and through the endocervical canal (the cervical canal) when it becomes inflamed, so that chronic endometritis and cervicitis (Cervical inflammation ) are etiologically related. [5], [6], [7]
Similarly, inflammation of the uterine appendages (salpingoophoritis) or chronic adnexitis and endometritis are related. In many cases there is no isolated pathogen and the infection is considered polymicrobial.
In addition, obstetric or postpartum endometritis - chronic endometritis after childbirth can occur in prolonged labor and after cesarean delivery. Chronic endometritis after hysteroscopy (diagnostic or operative) can occur as an infectious complication.
Risk factors
Chronic endometritis can be associated with a number of triggering factors, including persistent infections (particularly STDs), frequent sprays, the presence of an IUD, repeated abortions, and sexual intercourse during menstruation.
Pathogenesis
The healthy endometrium, which is constantly undergoing changes during the active reproductive phase of a woman's life, contains a number of immunocompetent cells, including macrophages, killer cells (NK cells or granular lymphocytes), subpopulations of B-lymphocytes and T-lymphocytes (T-helper cells). During the cycle, when the functional endometrial layer peels off during menstruation, the composition and density of these endometrial defense cells change periodically. [8]
In the chronic form of endometritis, the pathogenesis is explained by a chronic inflammatory response to bacterial colonization of the inner uterine mucosa and disruption of its integrity - with secretion of pro-inflammatory cytokines (including interleukins IL-6 and IL-1β); expression of chemotactic cytokines and extracellular adhesion molecules; activation of macrophages and influx of neutrophils (polymorphonuclear leukocytes that can directly penetrate tissues to destroy invading bacteria); and increased secretion of immunoglobulins (antibodies). [9], [10]
Chronic endometritis associated with pelvic infectious and inflammatory diseases is considered plasma cell endometritis with the accumulation of lymphocytic plasmacytes, plasma cells that play an important role in the adaptive immune response, as they are able to secrete immunoglobulins, in the affected endometrium.
Symptoms of the chronic endometritis
Although chronic endometritis can cause abnormal uterine bleeding and intermenstrual bleeding, in almost one-third of cases, patients have no symptoms. [11]
The first indirect signs of chronic endometritis may also be absent or manifested by general discomfort in the pelvis and deterioration of well-being, which patients do not focus on.
This disease can cause abdominal bloating, dyspareunia (painful sensations during sexual intercourse).
Discharge in chronic endometritis in the form of leucorrhea (whites), in severe cases of vaginal discharge purulent. And pain in chronic endometritis of a pulling or aching nature, in the lower abdomen or pelvis.
If there is an exacerbation of chronic endometritis, the symptomatology becomes more pronounced: there may be an increase in temperature in the form of fever, increased pain and discharge (which may be serous-purulent).
The intensity of the inflammatory process can vary, and its degrees (determined by endoscopic diagnosis or by histologic examination of a sample of injured tissue) are described as follows:
- Chronic inactive endometritis;
- Minimal chronic endometritis;
- Chronic endometritis of weak activity, sluggish or chronic weak endometritis;
- Moderately active chronic endometritis;
- Chronic active endometritis or severe chronic endometritis.
Chronic endometritis and pregnancy
According to experts, it is problematic to bear a child with chronic endometritis, as this disease leads to an unintended pregnancy. This is due to the fact that the ability of the immune system of the maternal body to accept the zygote and embryo is reduced, because with chronic inflammation of the endometrium in its mucous epithelium, the balance of NK-cells (natural killer cells) is disturbed: against the background of a decrease in CD56-lymphocytes producing immunoregulatory cytokines, there is an increase in cytotoxic CD16-lymphocytes. Another factor is morphological changes in the structure of the endometrium, as a result of which the mechanisms of introduction of the fertilized egg into it are disturbed.
Pregnancy after chronic endometritis - that is, after its effective treatment - is possible, and if normal reproductive function of the endometrium is restored in the process of pregravidar preparation of women leads to childbirth.
By the way, chronic endometritis must be treated before IVF: untreated inflammatory disease of the uterus reduces the likelihood of success of this procedure, and can also lead to intrauterine infections of the fetus and premature labor. [12]
Forms
Although there is no single classification of this inflammatory disease of the uterus, gynecologists distinguish several types of chronic inflammation of the endometrium.
According to the degree of involvement of the inner mucous membrane of the uterus in the inflammatory process distinguish focal chronic endometritis (limited or localized) and widespread or chronic diffuse endometritis.
When the causative agent causes minor inflammation and most patients do not have significant symptoms or have nonspecific clinical manifestations, chronic nonspecific endometritis is defined.
Increased division of plasma cells with an increase in their number is characterized by chronic proliferative endometritis. But due to the inflammatory process proliferative endometrium in chronic endometritis is damaged. Proliferative endometrium is called when the healthy inner mucous membrane of the uterus in a certain period of the menstrual cycle is preparing for the attachment of a fertilized egg. In endometritis, the proliferative function of the endometrium is impaired, resulting in bleeding and disrupting the conditions under which pregnancy can occur.
Chronic hyperplastic endometritis is accompanied by hyperplasia of the endometrium polyposis form, and hypertrophic - overgrowth of the mucosal epithelium of the inner uterine lining. Chronic inflammation of the endometrium caused by Mycobacterium tuberculosis is called chronic granulomatous endometritis.
Given the fact that the cause of chronic endometritis remains unidentified in almost 15% of cases, chronic autoimmune endometritis is also recognized, which may be the result of transformation of chronic inflammation into an autoimmune disease. One version of this transformation is based on the fact that T-lymphocyte-mediated inflammatory reactions play an important role in the development of autoimmune diseases through the reactions of T-helper (Th) cells of the adaptive immune system, which include Th1, Th2 and Th17 lymphocytes.
Complications and consequences
Chronic endometritis and infertility is a serious problem: inflammation leads not only to changes in the structure of the endometrium, but also to its endocrine dysfunction, which negatively affects the implantation of the embryo and may be the cause of infertility or habitual non-pregnancy. [13]
Among the complications of chronic inflammation of the endometrium are also noted: circulatory disorders in the uterine vessels and pelvic vascular pool, menstrual disorders, chronic pelvic pain, inflammation of the ovaries and fallopian tubes, the development of mucosal fibrosis and the formation of intrauterine synechiae (adhesions).
In severe cases, pelvic peritonitis (generalized infection of the pelvic organs), formation of uterine or pelvic abscess, septicemia.
Diagnostics of the chronic endometritis
Laboratory tests in the diagnosis of chronic endometrial inflammation include blood tests (total, for C-reactive protein, for antibodies) bacteriologic analysis of vaginal smear and microscopic examination of vaginal discharge. Although verification of ascending pathogens is considered problematic because of the significant mass of vaginal microorganisms.
The standard of diagnosis is endometrial biopsy: histology of the biopsy specimen determines the thickness of the inner uterine mucosa at a certain phase of the ovarian-menstrual cycle and reveals indirect signs of its inflammation in the form of the presence of at least one plasma cell (differentiated leukocytic B-lymphocyte) and more than five neutrophils in the field of view in the superficial epithelium of the endometrium. [14]
Immunohistochemical diagnosis of chronic endometritis is also performed, which in the framework of reproductive medicine is defined as IHC examination for chronic endometritis. This method makes it possible to detect specific immunohistochemical markers of chronic endometritis: the presence of plasma cells CD 138 and natural killer cells - NK-cells CD 56 in the uterine mucosa. [15], [16]
Instrumental diagnostics is necessary. It is difficult to diagnose chronic endometritis on pelvic and uterine ultrasound, as well as with transvaginal ultrasound, although experts note such echo signs of chronic endometritis as: hyperechogenic endometrial spots, a decrease in the thickness of the superficial mucous epithelium or asynchronous with the phase of the menstrual cycle thickening of the endometrium, Asherman's syndrome - intrauterine synechiae (adhesions), the presence of exudate and blood accumulation in the uterine cavity.
In the proliferative phase of the menstrual cycle, diagnostic hysteroscopy, which allows to detect morphologic signs of chronic endometritis:superficial edematous changes of the endometrium; focal hyperemia; endometrium-covered single or diffuse vascularized mucosal bulges (which are called micropolyps) - with accumulation of inflammatory cells (lymphocytes, plasma cells. Eosinophils); increased stromal density with spindle-shaped cells and inflammatory infiltration by plasmacytes. [17], [18] Even compared to histologic diagnosis of chronic endometritis, liquid hysteroscopy showed a very high diagnostic accuracy (93.4%). [19], [20]
The differential diagnosis differentiates between:
- Endometrial hyperplasia and chronic endometritis;
- Endometrial polyp and chronic endometritis;
- Uterine adenomyosis and chronic endometritis;
- Chronic endometritis and endometriosis (endometrioid disease).
Endometritis should also be differentiated with myometritis and endomyometritis (spread of inflammation to the muscular layer of the uterine wall); endoparametritis - infectious inflammation involving the surrounding uterine tissues; precancerous hyperplastic polyposis of the uterus. [21]
Who to contact?
Treatment of the chronic endometritis
Antibiotics for chronic endometritis are the main drugs for treating infectious lesions of the uterine mucosa. [22]
The therapy regimen or protocol for the treatment of chronic endometritis includes a fairly long-term use of different types of antibacterial drugs in appropriate dosages.
First-line therapy: taking an antibiotic of the tetracycline group Doxycycline - 0.1g twice a day for two weeks). [23]
In second-line therapy, the course of which lasts 14 days, combine an antibiotic of the fluoroquinolone group Ofloxacin (twice a day for 0.4 g) and nitroimidazole antibiotic Metronidazole (orally for 0.5 g twice a day).
If these drugs do not give the expected result, then on the basis of bacteriological examination of a sample of endometrial tissue with a relative antibiogram are used:
- In the detection of gram-negative bacteria - fluoroquinolone antibiotic Ciprofloxacin (C-flox ) 0.5 g twice a day for 10 days; cephalosporin antibiotics ceftriaxone (Cefotaxime, Cefaxone, Ceruroxime) 0.25 g intramuscularly once + Doxycycline (0.1 g twice a day for 14 days);
- For Gram-positive bacteria - Amoxiclav (for 8 days, 1 g twice a day);
- For mycoplasma and ureaplasma - an antibiotic of the macrolide group Josamycin or Vilprafen (twice a day, 1 g for 12 days).
Good effect is given by intrauterine instillations in chronic endometritis - introduction of Ciprofloxacin solution into the uterine cavity (in concentration 200 mg/100 ml every 3 days, 10 procedures) or solution chlorophyllin.
In cases of chronic granulomatous endometritis, antituberculosis therapy is performed: Isoniazid + Rifampicin + Ethambutol + Pyrazinamide.
If uterine adhesions are present, vaginal suppositories are recommended longidase.
Additionally, systemic enzyme therapy with Vobenzyme or Flogenzyme may be performed; immunomodulatory agents such as Inflamafertin or Pyrogenal may also be prescribed.
Synthetic progesterone, that is, a means of hormone replacement therapy - the drug Duphaston in chronic endometritis can be used only in cases of endometrial hyperplasia.
During remission, physiotherapy for chronic endometritis can be used: UHF, electrophoresis, diadynamic therapy and magnetotherapy, which improve vascular hemodynamics in the pelvic basin and can reduce inflammation. Cavitation of the uterus in chronic endometritis may be performed - exposure to low-frequency ultrasound waves in combination with drug solutions.
Surgical treatment includes curettage (scraping) of the uterine cavity and removal of intrauterine synechiae.
Prevention
To prevent infectious lesions of the uterine mucosa, one should protect oneself from STDs by using barrier contraceptives; treat sexually transmitted infections as early as possible, as well as diseases of the organs of the female reproductive system.
Forecast
In most cases (60% to 99%), chronic endometritis is cured with antibiotics, but if endometrial inflammation is prolonged, the possibility of malignization cannot be excluded. Cesarean section leads to a 25-fold increase in endometritis-related mortality. [24]

