Vestibuloplasty
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
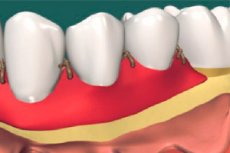
Surgical correction of the vestibulum oris, which is the space separating the lips and cheeks from the alveolar processes of the jaws and teeth, is defined in medicine as vestibuloplasty.
This operation involves deepening this space by changing the attachment of soft tissues - by lowering the muscles that attach to the cheek, lip and lingual sides of the jaw. This not only reduces the tension of the gingival margin (created by the fibers of the muscular plate of the alveolar mucosa), but also restores the height of the upper part of the alveolar bone bed (alveolar ridge), which is necessary to support the denture. [1]
Indications for the procedure
Surgical intervention in such a pathology of the dentoalveolar system as a shallow vestibulum of the oral cavity is aimed at deepening it, because the insufficient size of the vestibulum oris can lead to periodontal disease, malocclusion, defects of tooth rows; it can increase the accumulation of dental plaque, which can further lead to inflammation and gingival recession, as well as the formation of periodontal pockets. [2]
Specialists note such basic indications for vestibuloplasty as:
- Abnormally shallow oral vestibule;
- Focal periodontal lesions with denudation of tooth necks and roots in progressive periodontal disease;
- Preventing vertical displacement of the soft gingival tissues, i.e. Recession or gingival recession;
- Preparation for orthopedic treatment - implantation and dentures - in case of insufficient depth of the oral vestibule and/or alveolar bone resorption;
- The elimination of certain diction disorders.
Vestibuloplasty can be performed on children for the same indication.
Preparation
Preparation for this surgery includes an examination by a dentist, orthodontist, and oral surgeon; an X-ray or CT scan of the jaw is required; and a general blood test and coagulogram are taken.
You should stop taking anticoagulants (drugs that reduce blood clotting) one week before your surgery appointment.
The last meal before surgery should be at least 6-7 hours before surgery.
Technique of the vestibuloplasty
Depending on the indication, vestibuloplasty of the lower or upper jaw is performed.
The technique depends on the chosen technique: with mucosal advancement, with secondary epithelialization or with the use of mucosal-gingival autograft.
The main stages of vestibuloplasty include: antiseptic treatment of the oral cavity; local anesthesia; dissection of the transitional fold - a section of the gingival mucosa between its mobile part (near the base of the alveolar process of the jaw) and the immobile part; making additional incisions - for separation of the mucosal periosteal flap (from the nearest part of the gingiva); moving the flap to form a deeper vestibulum oris; suturing.Sutures in vestibuloplasty are non-absorbable knotted sutures. [3]
A mucosal autograft can also be obtained from the mucosa of the palate or cheeks. The graft from the palate is cut in the shape of a horseshoe in the periosteal plane, the place of the taken flap is most often left open (healing occurs by re-epithelialization). A spindle-shaped flap is cut from the mucosa of the inner side of the cheek, and the graft site is closed with absorbable flat sutures.
In the case of ankyloglossia - short frenulum (Latin: frenulum) - vestibuloplasty of the oral vestibule and frenuloplasty (by cutting the frenulum) can be performed at the same time.
Methods of vestibuloplasty
There are different techniques or methods of vestibuloplasty.
Edlan-Mejcher vestibuloplasty (Edlan A., Mejcher B.) allows to expand the gingival attachment ligaments and deepen the vestibule of the oral cavity. It is a vestiboplasty of the mandible, in which the mucosa is dissected below the lip in a direction parallel to the curve of the bony arch; the mucosa flap (the so-called free mucosal graft) is cleaned from fibers and shifted from the incision line towards the jaw and fixed with suture materials; a protective dressing is applied to the wound.
However, the main disadvantage of this method is the exposure of the inner lip area in the vestibulum oris. Therefore, a variant of the operation was developed - the Schmidt modification, in which the periosteum is not peeled off the alveolar process, but the tissues near the periosteum are dissected and their free edges are immersed deep into the anterior mouth cavity, where they are fixed with sutures.
Vestibuloplasty according to Kazanjian (Kazanjian V.), developed in the first third of the 20th century by an American maxillofacial surgeon, consists of separating the labial flap on a pedicle and removing the muscle layer between the mucosa and periosteum. In this technique, the tissues are restored by re-epithelialization, which over time led to postoperative scarring and reduction of the depth of the vestibulum oris. [4]
This disadvantage of the Casagnan technique was overcome by its modification - vestibuloplasty according to Clark, which consists in separating the flap for transfer to the gingival periosteum not from the lip side, but from the alveolar side. [5], [6]
Vestibuloplasty is performed according to Glickman - with dissection of soft tissues in the place of lip attachment and placement of the newly formed free edge in the depression of the vestibule of the mouth (and fixing it with sutures).
Tunnel vestibuloplasty is suitable for correcting the gum on both jaws, which is considered a more gentle method due to the minimal wound size. To reach the mucosa, the doctor makes three small incisions: the first one along the frenulum, the second and third ones horizontally towards the small molars. [7]
Laser vestibuloplasty can be performed: a diode laser is used to dissect the tissue and remove muscle fibers to widen the vestibule. This surgery minimizes scarring, and healing is also faster. [8]
Contraindications to the procedure
The following conditions may be contraindications to the procedure:
- Extensive tooth decay;
- Oral infections (stomatitis, gingivitis);
- Periodontitis and pulpitis;
- Bleeding gums;
- Inflammation of the periosteum of the jaw - periostitis;
- Inflammation of the submandibular salivary glands;
- Blood disorders;
- Collagenoses;
- Osteomyelitis;
- Malignant tumors of any localization and radiation therapy of the head and neck.
Consequences after the procedure
Possible complications after the procedure may manifest themselves in the form of bleeding, swelling of the gum, inflammation (in case of infection of the postoperative wound) with increased pain and fever.
The most likely adverse effects include scar formation and scar tissue deformation, paresthesia of the area from which the mucosal periosteal flap was taken, and spasm of the masseter muscle after healing.
The effect of vestibuloplasty on the face is not excluded, in particular, thickening or sagging of the chin may be observed, as well as a decrease in the height of the lower lip and anterior facial height.
Care after the procedure
To ensure that the care after the procedure is carried out correctly, and the rehabilitation is not prolonged and was successful, you should follow the medical recommendations after vestibuloplasty.
After the procedure, the oral surgeon may prescribe a combination of antibiotics, painkillers, and mouthwashes to prevent pain and plaque buildup.
Patients should not:
- Physical exertion (for one week after the procedure);
- About the same amount to brush your teeth;
- Eat hard, hot, salty and spicy foods;
- Smoking and drinking alcohol.
Patients need:
- Rinse your mouth with antiseptics recommended by your doctor;
- Brush your teeth (when authorized by your doctor) with a soft toothbrush.
After about four weeks, the vestibuloplasty site should heal noticeably.
