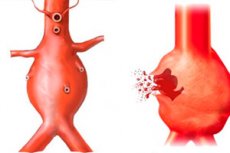
Ruptured aortic aneurysm
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Even with regular monitoring of the dynamics of aortic aneurysm development, it is impossible to predict the course of the pathological process in advance. Unfortunately, complications occur quite often, and the problem can be completely eliminated only by surgery. The most severe and unfavorable consequence can be the rupture of the aortic aneurysm. If the altered segment of the artery increases at a rate of 5 mm per year, and the diameter size of the vessel exceeds 45 mm, the risk of developing this complication increases dramatically, which serves as an indication for surgical intervention.
Epidemiology
Aortic aneurysm rupture occurs in about one out of ten thousand hospitalized patients (according to other data - aneurysm rupture occurs in 6 cases per 100 thousand people per year). But we should take into account the fact that more patients die before hospitalization.
The prognosis is more unfavorable in the elderly and women, due to frequent atypical manifestations and late diagnosis.
The most common risk factor for aneurysm rupture is arterial hypertension, which is diagnosed in 70% of patients. The average age of those admitted with aneurysm ruptures is 62-64 years, of whom men account for about 65%.
Approximately two cases of stratification are found per 800 postmortem medical examinations (autopsies), ten cases per 1,000 people with sudden death, and up to 4% of deaths from cardiovascular abnormalities.
In the absence of medical care, the early mortality rate for patients with stratification is estimated at 1% per hour - that is, one patient in a hundred dies hourly - in the first 24 hours, up to 75% die within 14 days, and more than 90% die over several months.
Aortic aneurysm rupture occurs more often between the ages of 60 and 70, in the male population more often than in women. [1]
Causes of the a ruptured aortic aneurysm.
The most common causative factor of aortic aneurysm rupture is high blood pressure, which is observed in 75-85% of patients with this pathology. Congenital diseases that can lead to rupture are Marfan, Ehlers-Danlos, Turner syndromes, as well as congenital bicuspid aortic valve, aortic coarctation, giant cell aortitis, recurrent polychondritis.
There have been cases of aneurysm rupture in pregnant women, particularly in patients under 40 years of age, mostly in the third trimester of gestation. Like acute myocardial infarction and sudden death syndrome, aortic rupture follows a seasonal and circadian rhythmicity, with the highest number of cases occurring in winter and in the morning hours (4-5 am). This relationship is explained by physiologic changes in blood pressure indices. [2]
A ruptured aortic aneurysm complicates such congenital abnormalities:
May act as complications of acquired pathologies:
- Aortitis;
- Aortic atherosclerosis, hypertension;
- Closed chest contusion;
- Toxemia of pregnancy, etc.
There are descriptions of arterial dissection with further arterial rupture after medical manipulations, in particular, after cannulation of the main vessel or its branches, insertion of a counterpulsation device. Iatrogenic dissection with rupture is more characteristic of elderly patients and is more often detected against the background of marked atherosclerotic changes.
In most cases, rupture results from aortic dissection, which, in turn, is caused by degeneration of the media. Aneurysms arise as a result of degenerative processes associated with atherosclerosis or as a reaction to structural disorders of the arterial wall with changes in the levels of tissue metalloproteinases.
Risk factors
Major risk factors:
- Genetics (if close male relatives have had aneurysms with or without rupture);
- Cardiovascular pathologies (arterial hypertension, ischemic heart disease, heart defects, myocardial infarction, arterial stenoses);
- Violation of lipoprotein levels in the blood, progressive atherosclerosis.
Other risk factors include:
- History of aortic or aortic valve disorders;
- Unfavorable hereditary history in terms of any aortic pathologies;
- Undergone coronary surgical interventions;
- Smoking, drug use (particularly amphetamine, cocaine);
- Chest contusions;
- Traffic accidents.
According to pathologic anatomic data, aortic rupture was present in 20% of cases in persons who died as a result of motor vehicle accidents. [3]
Pathogenesis
When the inner layer of the artery is torn, an aneurysm dissection forms. Blood, pushed by pressure, penetrates through this rupture and peels off the middle aortic sheath. Hemorrhage can be directed along the course of the vessel: in this situation, the hematoma occludes one of the branches - from the aortic arch to the intestinal arterial vessels. Retrograde detachment negatively affects the strength of the aortic valve flaps and to its insufficient functioning. The formation of the false channel occurs in the outer part of the middle aortic sheath. The outer wall is only ¼ of the original thickness of the aortic wall. This development is the most frequent mechanism of vessel rupture in patients with a dissecting aneurysm.
Rupture in the region of the aortic arch is carried mainly into the mediastinal cavity, rupture of the descending aorta - into the left pleural cavity, and rupture of the abdominal aorta - into the retroperitoneal region.
Because the parietal pericardium connects to the ascending aorta, proximal to the brachial trunk outlet, rupture of any of the ascending segments can provoke pericardial tamponade.
Approximately 70% of cases of rupture occur in the ascending aorta, 10% of cases involve the arch, and 20% of cases involve the descending aorta. The abdominal aorta is the most rarely ruptured.
A dissecting aneurysm is formed predominantly after rupture or stretching of the internal aortic layer, against the background of intramural hemorrhage. Rupture of the inner layer is more often caused by increased pressure and/or stretching of the vessel. Under the influence of constant pulsation of blood flow, the vascular layers separate.
The ascending aorta can rupture at different sites:
- In 60% of cases there is a rupture of the convex surface;
- In 30% of cases - rupture of the distal segment from the left subclavian artery;
- 10% of cases, aortic arch rupture.
Fewer than 10% of patients have spontaneous ruptures.
In pathology, the following variants of the course of pathology are classified:
- Aortic rupture occurs without dissection.
- The inner aortic layers are torn, the layers are separated by the flow of blood, and then the intra-wall hemorrhage bursts into the tissues surrounding the aorta.
- The hematoma ruptures into the aortic lumen, and a chronic dissecting aneurysm is formed.
- An intra-wall hematoma forms with risk of rupture.
The complexity of the disorder lies in the fact that the aortic aneurysm itself can exist for many years without any obvious symptomatology. At the same time, the risks of developing a complication are present almost every minute. A rupture of an aneurysm causes severe bleeding, which, for the most part, ends in death. Even in countries with the highest medical capabilities, the pre-hospital mortality rate is up to 40%, and at the postoperative stage - up to 60%.
Symptoms of the a ruptured aortic aneurysm.
The clinical presentation of a ruptured aortic aneurysm usually includes the following signs:
- Sudden sharp pain in the chest or abdomen (depending on which part of the aorta is damaged);
- A sharp drop in blood pressure readings;
- Severe heart palpitations;
- Sudden onset of shortness of breath;
- Lividity of the skin;
- Motor and speech stupor;
- Increased sweating (cold, clammy sweat);
- Nausea, vomiting;
- Severe dizziness;
- Blurring and loss of consciousness.
Rupture of an aortic dissecting aneurysm is the final stage of the gradual separation of the vessel into layers, with rupture of the last, outer layer by blood flow. Specialists note that the imminent approach of rupture in many cases can be detected long before the development of the complication. Thus, some patients complain of increasing persistent pain (in the chest, abdomen, back - depending on the localization of detachment), an increase in blood pressure, false angina attacks that are not amenable to drug correction. If these problems are addressed in time to a competent cardiologist, it is possible to save not only the health, but also the life of the patient with an aneurysm.
Ruptured abdominal aortic aneurysm, ruptured abdominal aortic aneurysm are identical concepts indicating the violation of the integrity of a large section of the descending aortic vessel below the area of its intersection with the diaphragm. If there is a risk of complication, the patient feels a dull but increasing pain in the abdomen or under the ribs. Often a throbbing, or pulsating pain is felt. At the moment of rupture, all the signs of severe internal bleeding are noted. At the same time, even a few seconds of delay significantly reduce the patient's chances of life.
Rupture of a thoracic aortic aneurysm follows the same principle:
- Sharp, "tearing" pain in the chest;
- Symptomatology of hemorrhagic shock (sudden weakness, dizziness, nausea, dry mouth, darkened eyes, blurred and loss of consciousness).
Sharp pain may go to the back, shoulders and abdomen. In many cases, the pathology runs like an acute infarction, mesenteric thrombosis, pulmonary embolism, which requires careful, and at the same time rapid differentiation.
A ruptured aneurysm of the ascending thoracic aorta also reveals itself with signs of internal bleeding:
- Abrupt (collapsed) weakness;
- Fainting (collapse);
- Pale, blue skin;
- Drop in blood pressure readings (literally "before your eyes");
- Increased heart rate.
The intensity of the signs of rupture builds up almost immediately: the fatal blood loss is far from always replenished in time or the bleeding can be stopped. Therefore, the problem often ends with a fatal outcome.
Aortic arch aneurysm rupture is accompanied by a massive release of blood into the pleural or pericardial cavity. There is severe pain behind the sternum, radiating to the neck, shoulders, arms, back, shoulder blades. Possible bloody vomiting, coughing up blood. The patient loses consciousness and quickly dies if no help is rendered.
Complications and consequences
Aortic aneurysm rupture is associated with a high mortality rate and an equally high incidence of adverse effects and complications, even with timely surgical intervention. The mortality rate, according to different information, reaches 60-80%.
Additional danger is posed by such complications that pose a direct threat to the patient's life - these are cardiovascular and respiratory complications, ischemia of the digestive tract and lower extremities, thromboembolism, compartment syndrome. These disorders are typical for the hospital and postoperative period.
Despite the fact that the quality of therapeutic measures in emergency and critical conditions is regularly improved and perfected, the results of treatment of acute aneurysm rupture continue to remain at an unsatisfactory level. This point is especially true for regions that do not have specialized vascular centers and specialized hospitals with appropriate equipment and qualified surgical and anesthesiological staff.
The most common postoperative complications are ischemic colitis and vascular embolism. The most dangerous life-threatening disorders are acute renal failure, pneumonia and wound infection.
Diagnostics of the a ruptured aortic aneurysm.
Diagnostic manipulation is performed immediately in a facility with surgical capabilities. Differentiate with other likely causes of internal pain and massive blood loss. The following findings are required:
- Laboratory tests:
- Determination of blood group, Rh factor;
- Evaluation of platelet level;
- Evaluation of platelet aggregation function;
- Study of plasma hemostasis;
- Study of fibrinolysis.
- Instrumental diagnostics is represented by imaging studies (angio-computed tomography, transesophageal echocardiography, chest radiography, magnetic resonance imaging).
Differential diagnosis
Limited rupture of an aortic aneurysm can be suspected if the diagnosis identifies pathologic dilation of the artery with a preserved wall, and the patient notes the appearance of sharp pain. In this situation, there is a high risk of further rupture, which is usually indicated by recurrence or persistence of pain syndrome, fluid accumulation in the abdominal or pleural cavity.
During visualization, a ruptured aortic aneurysm is often difficult to distinguish from a limited rupture. It differs from the violation of the integrity of the free wall, in which all wall layers are destroyed and a massive hematoma is formed: a limited rupture with or without the formation of a false aneurysm is characterized by the formation of perivascular hematoma, which "hides" behind the periaortic structures - in particular, pleura, pericardium, mediastinum, retroperitoneal space, or nearby organs. Patients with limited aortic rupture are characterized by stable hemodynamics.
Treatment of the a ruptured aortic aneurysm.
A ruptured aortic aneurysm is an absolute indication for emergency surgery. If there is a suspicion of rupture, it is necessary to immediately call an emergency team: any delay will cost the patient's life.
Before the paramedics arrive, these steps should be followed:
- The patient should be placed in a horizontal position with the headrest elevated;
- We need complete rest, with absolutely no movement;
- Before the arrival of the ambulance, it is necessary to constantly talk to the patient, if possible to reassure him, preventing the appearance of panic and shock attacks;
- Under no circumstances should food or drink be offered to the victim;
- To reduce pain, it is allowed to give the patient a tablet of nitroglycerin.
First medical aid is carried out against the background of hospitalization by the cardiac resuscitation team in the surgical department and includes:
- Pain control (administer non-narcotic and narcotic analgesics (Promedol, Morphine, Omnopon);
- Shock control (cardiopulmonary resuscitation);
- Normalizing blood pressure.
Medications
Emergency care for aneurysm rupture involves emergency delivery of the patient to a specialized surgical facility for emergency surgery. At the same time, provide vigorous administration of crystalloid solutions (approximately 3 ml per 1 ml of blood loss) or colloid solutions (approximately 1 ml per 1 ml of blood loss), but only until it is possible to administer the preparation of red blood cells. Determine the blood group, transfused red cell mass, blood from a universal donor or preparation of the appropriate group. Observe hematocrit, not allowing it to fall below 30%. In addition to the red cell mass transfused fresh frozen plasma, platelet concentrate and cryoprecipitate. Thromboconcentrate is used when the platelet count is less than 50 thousand / μL, and cryoprecipitate in the amount of 1 unit / 10 kg m. T. At a concentration of fibrinogen less than 1.5 g / L. Transfuse 1 unit of fresh frozen plasma and 1 unit of thromboconcentrate for each unit of red cell mass transfused.
Control body temperature, correct acidosis and hypocalcemia. It is possible to use tranexamic acid (intravenously, in a loading dose of 1 g for 10 minutes, further as indicated), transfusion of blood components, the use of recombinant activated factor VII.
Surgical treatment
The peculiarity of surgical interventions for ruptured aortic aneurysm is that they are carried out as urgently as possible, since every minute of delay significantly increases the likelihood of a lethal outcome. Preparation of the patient for surgery is practically absent and should not delay the start of manipulation regardless of the conditions. It is important to provide venous access (any type - peripheral, central-venous) and start infusion and transfusion therapy. If the initial systolic pressure is less than 70 mm Hg, then prior to induction anesthesia, infusion of norepinephrine to a systolic pressure of 80-90 mm Hg is performed. Antibiotic prophylaxis is represented by 2-3 generation cephalosporins.
In the process, blood pressure, heart rate, oxygen saturation, electrocardiogram, diuresis, hemoglobin level, INR, APTV, fibrinogen and platelet count are monitored.
The following operations can be performed:
- Aortic valve excision surgery with prosthesis of the aortic valve and ascending aorta with a single combined implant.
- Supracoronary aortic prosthesis.
Surgery for aortic aneurysm rupture is lengthy, labor-intensive, and is performed against the background of large blood loss. It is performed under conditions of artificial circulation. With special care during the intervention provide protection of the heart muscle, using saline cardioplegic and alternative solutions. The patient is hypothermic, which against the background of high blood loss and prolonged artificial circulation leads to a large number of postoperative complications, including the development of DIC.
In prosthetics with reimplantation of neck and head vessels, blood circulation is completely stopped and retrograde perfusion of the brain is performed via the internal jugular veins. In this case, the brain is protected by providing deep hypothermia up to 12-14°C and administering drugs such as Seduxen, Propofol (reduce the brain's oxygen consumption). Prolonged and retrograde perfusion, inhibition of blood circulation cannot favorably affect the functionality of the central nervous system, so the percentage of postoperative complications is quite high.
During the intervention for the rupture of the descending thoracic aorta, a prosthesis with reimplantation of the intercostal vessels into the implant is performed. One of the peculiarities of the operation is bypassing the area of prosthesis installation with complete blood flow stoppage and retrograde cerebral perfusion. One-lung intubation and brain protection are performed.
Prevention
Aneurysm rupture can be avoided if the problem is detected and treated in time, without waiting for the complication to develop. Aneurysms can only be cured by surgery: conservative therapy is symptomatic and can only slightly improve the patient's quality of life without eliminating the pathology. Surgery can be performed in the classical way - as a cavity intervention, or by endoprosthesis.
Skilled surgical treatment of aortic aneurysm patients is safe in most cases, especially for young patients. During surgical intervention, the aortic vessel is clamped below and above the pathologically altered area, replacing the aneurysm area with a polyester section.
The risks of perioperative complications (cardiac and respiratory complications, postoperative hernias, limb paralysis and death) are higher in elderly patients. Endovascular treatment with an implantable stent is considered a safer procedure for such patients.
Other mandatory preventive measures to prevent aneurysm rupture include:
- Smoking cessation;
- Regular monitoring of blood pressure readings;
- Regular checkups;
- Control of body weight, blood cholesterol levels;
- Adherence to a low-cholesterol healthy diet.
An aneurysm detected and operated on early in its development is the best way to prevent aortic rupture.
Forecast
Aortic rupture is a formidable complication of the already insidious and unpredictable disease - aneurysm. The aorta is the main blood vessel that supplies blood to all organs and systems. This main artery comes from the heart and runs in the middle part of the chest and abdominal cavity, passing through itself a huge volume of blood under high pressure. Any violation of the integrity (rupture) of this vessel can provoke a life-threatening hemorrhage. The aneurysm itself is often practically unaware of itself and is detected incidentally during routine preventive examinations.
The risks of rupture are particularly high in large and rapidly enlarging aneurysms: in such situations, surgery should be seriously considered, even urgently. Emergency surgery for aortic rupture carries a much higher risk of mortality. Moreover, most patients with ruptured aneurysms die before the doctors arrive.
Cause of death in a ruptured aortic aneurysm
When an aneurysm ruptures, help must be provided not just quickly, but urgently, and it is exclusively surgical intervention. Without immediate surgery, there is massive blood loss and, as a consequence, death. Most patients die before reaching a medical facility. However, the chances of survival after surgical treatment are also not one hundred percent.
Massive blood loss is accompanied by a sharp decrease in circulating blood volume, the subsequent development of hypoxic and hypoxemic state, hypotension, a sharp deficit of blood supply to internal organs and increasing metabolic acidosis. DIC may also occur.
Already at a rate of blood loss of 150 ml per minute, the lethal outcome occurs within 15-20 minutes. Rupture of aortic aneurysm is accompanied by a lack of blood supply to the organs for their normal work, the development of hemorrhagic shock, loss of consciousness, cardiac arrest.

