Ethylene glycol vapor poisoning
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
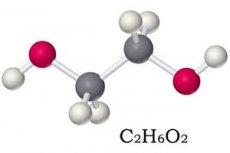
Although 1,2-dihydroxyethane (ethanediol-1,2) is classified as a third-rate toxicant of four by the degree of adverse effect on the body, ethylene glycol poisoning leads to very serious consequences and can result in death.
This slightly oily, sweet-to-taste clear liquid without color and odor is a dihydric alcohol. Worldwide, about two thirds of ethylene glycol is used as a chemical intermediate, as well as in the automotive antifreeze, brake fluid and anti-corrosion additives.
More details on the preparation of ethylene glycol, its properties and application in the publication - Ethylene glycol.
Epidemiology
According to Statistics Agency for Toxic Substances and Disease Registry (USA), from 2006 to 2013 inclusive, there were 45,097 cases of ethylene glycol poisoning among Americans, and in 154 cases the outcome was fatal.
Annually in the United States recorded more than 5.5 thousand cases of poisoning with this substance. In 84% of cases, poisoning occurs accidentally, two-thirds of the victims are men. And the death rate due to intoxication varies from 1 to 22% - depending on the amount of ethylene glycol that has entered the body, and the timeliness of the provision of medical care.
In the UK, up to 400 ethylene glycol poisonings per year are noted, but in 18% of the cases, the affected children are children under five years of age, and in 65% of cases among adults, poisonings were suicidal.
Causes of the poisoning with ethylene glycol
The minimum lethal dose of ethylene glycol for adults is 1.4-1.6 ml per kilogram of body weight, that is, with a weight of 80 kg it is 200-220 ml (according to other data, 90-100 ml). Causes of poisoning - accidental or deliberate use of a certain amount of ethylene glycol; for example, in alcoholics, replacing vodka with antifreeze or brake fluid, there can be a re-poisoning with ethylene glycol.
And the pathogenesis of the toxic effect of ethanediol-1,2 lies in the products of its metabolism, which disrupt the functioning of the kidneys, cardiovascular and nervous system.
Ethylene glycol is rapidly absorbed through the gastrointestinal tract, and its vapor or aerosol is absorbed through the respiratory tract. After absorption, ethylene glycol is distributed in internal fluids.
In the liver and kidneys, he undergoes enzymatic metabolism. First, with aldehyde oxidase and aldehyde dehydrogenase, it is cleaved to glycoldehyde, which rapidly converts to glycosyl acid (glycolate) and ethanedioic acid dialdehyde (glyoxal).
Further transformation of glycosyl acid leads to the formation of glyoxylate, which in turn is split into: formate (methanoic acid salt), ethanedioic or oxalic acid salt (oxalate), glycine (aminoacetic acid) and carbon dioxide dioxide gas.
As a result of the accumulation of acid metabolites, the acid-alkaline balance of the organism is disturbed (including the pH of the arterial blood), provoking a state of metabolic acidosis that negatively affects the functioning of the nervous system, lungs and heart.
Excretion of ethylene glycol occurs through exhaled carbon dioxide and excreted in the urine of ethylene, glycol and glycolic acid. It is believed that the elimination half-life for humans is in the range of 2.5-8.4 hours.
 [11]
[11]
Risk factors
The risk of ethylene glycol poisoning, as well as the cause, is its ingestion. This also applies to cases when a brake fluid is poisoned, in which 1,2-dioxoethane is present.
When this substance is poured out in an industrial plant or from a container in a residential area, there is no poisoning. But people working in industries where ethylene glycol is used can be contacted for a long time with raw materials or products containing it, which is why ethylene glycol can be poisoned in small doses. In particular, airport workers who are involved in processing runways and aircraft against icing in the winter (by spraying appropriate liquids) can be exposed to low levels of ethylene glycol on the respiratory tract. Therefore, now the ethylene glycol has been replaced with propylene glycol.
Experts note that factors that affect the risk of poisoning when exposed to ethylene glycol include its dose, duration and nature of contact. It is believed that background concentrations of ethylene glycol in air, soil, surface and groundwater do not lead to poisoning.
Symptoms of the poisoning with ethylene glycol
After ingestion of ethylene glycol, the first signs of CNS depression appear as alcohol intoxication - with dizziness, excitement or increased drowsiness. But this short latent period is quickly replaced by the first phase (stage or stage) of toxic effects, which can last up to 12 hours and is manifested by a disorder of the gastrointestinal tract (with nausea, vomiting and abdominal pain), as well as tachycardia, confusion, convulsions , headache, nystagmus and a reduction in urinary output.
In the second stage (12-36 hours after administration) metabolic acidosis and associated cardiac and pulmonary symptoms of ethylene glycol poisoning develop: superficial rapid breathing (tachypnea) with tachycardia, increased pulmonary ventilation (hyperpnoea), cyanosis, pulmonary edema and / or stopping heart.
Often in the second phase of poisoning, cardiopulmonary symptoms are not so obvious, therefore, attention should be paid to acidosis, acute renal failure and suppression of CNS functions, which may manifest neurological symptoms, including hearing loss and facial paralysis.
In the third phase of intoxication, which lasts an average of 24-72 hours, the nephrotoxicity of the metabolites of ethylene glycol-renal damage (with parenchyma necrosis and oxalate crystal precipitation) -is caused pain in the lumbar region and diuresis (anuria or oliguria).
Inhalation effects of ethylene glycol with an average concentration in the air up to 140-200 mg / cc. M within five minutes causes ethylene glycol vapor poisoning - a strong irritation of the upper respiratory tract, including a burning sensation in the trachea and cough, and also affects the lungs, heart, central and peripheral nervous systems, liver, hematopoietic and lymphoreticular systems.
At lower concentrations, chronic ethylene glycol poisoning is possible, accompanied by a feeling of weakness, dizziness, irritation of the mucous membranes of the nose and eyes, increased heart rate and blood pressure, and immunosuppression.
Complications and consequences
Intoxication with ethylene glycol occurs quite often, and without rapid detection and timely treatment, the risk of death from this substance remains high. The cause of this are such consequences and complications as acute renal failure, hemodynamic instability and brain damage leading to coma.
A decrease in the level of calcium in crocs - hypocalcemia - leads to severe seizures, tetany, a violation of the rhythm of heartbeats and blockade of the heart.
Diagnostics of the poisoning with ethylene glycol
Since many clinical symptoms of ethylene glycol poisoning are also manifested in other types of intoxication, diagnosis is often difficult.
In addition, in patients, especially children entering the hospital within an hour after ingestion of ethylene glycol, signs may not yet appear.
Helps to diagnose ethylene glycol poisoning tests:
- blood test for the content of ethylene glycol;
- the analysis of blood and urine at the osmolar interval, that is, the determination of osmolality of blood serum;
- biochemical blood tests for determination of pH, for serum electrolytes (calcium, potassium, chlorides), for glucose, urea and creatinine;
- urine analysis at pH, content of nitrogen and creatinine; on protein levels, β-N-acetylglucosaminidase and β-2-microglobulin;
- microscopy of urine for the detection of crystals of calcium oxalate.
Differential diagnosis
Differential diagnosis is carried out on the basis of the results of these analyzes, since the differential diagnosis includes poisoning with salicylates, metformin, methanol, isopropyl alcohol, chloroethanol, dimethyl sulfate, as well as alcoholic or diabetic ketoacidosis, lactacidemia or acute kidney failure.
Treatment of the poisoning with ethylene glycol
First of all, urgent help is required in case of ethylene glycol poisoning: emptying the stomach and washing it with a large amount of soda solution (tablespoon per liter of water), which is effective only after the ingestion of ethanol - during the first hour.
But to use activated charcoal does not make sense, since it does not adsorb 1,2-dioxyethane.
Further, the treatment of ethylene glycol poisoning is aimed at blocking the formation of its toxic metabolites and the development of acidosis, for which the intravenous antidote is injected with ethylene glycol poisoning - ethanol or 4-methylpyrazole.
In most cases, apply ethanol (ethyl alcohol): iv in 10 ml / kg 10% ethanol in 5% dextrose for 30 minutes; Oral - diluted 95% ethyl alcohol (at the rate of 1 ml / kg).
With a sufficient concentration of ethanol in the blood (up to 100 mg / dL), the biochemical transformation of ethylene glycol almost completely stops. In emergency situations, toxicologists recommend using an equivalent amount of any strong alcoholic beverage inside.
Rapidly reducing the metabolites of ethanediol-1,2 in the blood helps hemodialysis in acute poisoning.
Then the efforts of the doctors are directed:
- on the correction of acidosis and hyperkalemia by intravenous drip during the first few hours of a solution of sodium bicarbonate (150-200 ml / h) with monitoring the level of potassium in the blood;
- on excretion of the organism from acidosis states (at blood pH <7.25-7.3) - also by hemodialysis or peritoneal dialysis;
- on maintenance of an adequate diuresis (introduction of a liquid orally or intravenously);
- on the fight against hypocalcemia - infusions of calcium gluconate (10% solution with dextrose or saline solution).
Depending on the pathological consequences of intoxication - to maintain the functions of individual organs and systems - apply the appropriate medication.
Vitamins are also needed: thiamine (B1) 100 mg daily and pyridoxine (B6) 10-25 mg per day. The intake of these vitamins contributes to the cleavage of one of the toxic metabolites - glycosyl acid.
Outside the acute phase of poisoning, it is possible to use physiotherapeutic treatment, in particular, with the help of therapeutic hypothermia, as well as hyperbaric oxygenation.
Also read - Methods of stimulation of natural detoxification.
Forecast
It should be borne in mind that ethylene glycol poisoning is a potentially fatal intoxication. And a favorable prognosis of its outcome is largely correlated with early diagnosis and treatment.
When seeking medical help in later stages of poisoning, the prognosis may be unfavorable, especially if patients with severe acidosis. Even in case of survival, there is a high probability of developing chronic neurological disorders, as well as damage to the kidneys, often requiring continuous dialysis or kidney transplantation.

