Appendicular abscess: clinic, autopsy
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Acute appendicitis is a very common surgical pathology. Such a disease requires urgent surgical intervention, otherwise serious and life-threatening complications may develop. One of such complications is an appendicular abscess - suppuration in the area of an inflamed appendix.
Epidemiology
Appendicular abscesses are diagnosed relatively rarely: approximately 0.1-2% of patients with acute appendicitis.
As a rule, an appendicular abscess develops in the first three days from the onset of an acute inflammatory process in the appendix, or occurs as a complication of the infiltrate (a few days or several weeks after its formation).
Causes of the appendicular abscess
The development of appendicular abscess occurs only when there is no correct or timely treatment of acute appendicitis. Unfortunately, it is impossible to predict acute inflammation in the appendix in advance. In addition, pathology is often mistaken for other types of inflammatory processes in the abdominal cavity. Delayed time and incorrect diagnosis lead to the destruction of inflamed tissues of the appendix, with the development of peritonitis or appendicular abscess. There are individual risk factors, the presence of which increases the risk of untimely detection of appendicitis, and, as a consequence, the formation of an appendicular abscess:
- Atypical localization of the appendix can lead to the formulation of an initially incorrect diagnosis - inflammation of the kidneys, uterus, ovaries, enterocolitis, cholecystitis. As a result, the patient is offered treatment for other diseases, instead of urgent surgical intervention. In this case, the diagnosis of appendicitis becomes clear only when forming an abscess.
- Strong antibacterial treatment at the time of the initial inflammation in the appendix can lead to a decrease in the inflammatory response and the formation of a so-called "cold" abscess - a slow process that can take place for several years without disturbing the patient.
- Late appeal for medical help for acute appendicitis often leads to the development of an appendicular abscess.
Pathogenesis
Isolate the primary abscess, which occurs immediately near the appendix, and the secondary, which develops at some distance. Formation of an abscess is preceded by the appearance of an appendicular infiltrate - a kind of fencing of an inflamed appendix from the space of the abdominal cavity.
The formation of the infiltrate is a consequence of the effusion of fibrin and the adhesion of the affected omentum, intestine, abdominal wall and appendix.
After the inflammation subsides, the appendix dissolves the infiltrate. But in the case when the purulent process diverges beyond the vermiform appendage, the infiltrate is suppressed.
The location of the appendicular abscess depends on the location of the appendix. More favorable for the patient, if the abscess is formed in the ileum zone against the background of the lateral location of the appendage: it is in this position that the maximum inflammation of the inflamed area from the abdominal cavity is observed.
The secondary appendicular abscess is formed somewhat differently. The purulent process, spreading to healthy tissues, affects the area of the mesentery of the small intestine, the zone near the liver, the diaphragm and the right kidney. By a similar scheme, secondary appendicular abscesses are formed after resection of the appendix with destructive inflammation.
Symptoms of the appendicular abscess
The beginning of appendicular abscess development by the nature of the clinical course differs little from acute appendicitis.
The first signs may look like this:
- the patient is sick, it may cause vomiting;
- there is a strong weakness;
- the pain in the abdomen is pulsating, it grows and becomes unbearable;
- observed bloating, increased gas formation;
- the body temperature rises.
When palpating the abdomen, the patient feels severe pain, but there are no symptoms of peritonitis. The body temperature is high (up to 40 ° C), accompanied by chills.
These symptoms may persist for 2-3 days.
Appendiceal abscess in children
During appendicular abscess in children, doctors distinguish several stages, by analogy with peritonitis:
- Reactive stage - lasts about a day from the onset of inflammation. The stage is characterized by the appearance in the child of common signs of an inflammatory reaction. It can be a change in mood, vomiting, increased heart rate, febrile temperature. There is a growing pain in the abdominal region, the muscles of the abdominal cavity are palpable during palpation.
- Toxic stage - lasts 1-3 days. There is symptomatology of severe intoxication and dehydration: the skin of the child is pale, eyes shine, bouts of vomiting become permanent.
- The terminal stage is detected on the 3rd day and is characterized by the defeat of the whole organism. In the first place, internal organs suffer, signs of respiratory and cardiovascular insufficiency appear.
After the reactive stage, the child's condition can be mistakenly improved - the pain becomes less pronounced. However, after a while the baby feels very bad. There is a tendency: the older the child, the longer the period of false improvement can be.
Where does it hurt?
Complications and consequences
With the development of an appendicular abscess, the importance of how quickly medical care was first of all depends on the severity of the consequences.
If medical care was not provided at all, or had, but too late, then the death of the patient may occur.
Timely and qualified medical intervention provides every chance for complete recovery of the patient.
The most likely complications of an appendicular abscess can be:
- sepsis - systemic inflammatory reaction;
- gangrenous lesion of internal organs;
- adhesive process;
- peritonitis;
- liver failure.
Most complications of appendicular abscess are a serious danger not only for health, but for the life of the patient. The reason for this is a purulent infection that spreads throughout the body in a short time.
Diagnostics of the appendicular abscess
At the first signs of appendicitis, the patient must be immediately taken to a medical institution. The doctor will examine the patient without fail, will probe the abdomen and assess the condition of the patient as a whole.
Diagnostic measures for suspected appendicular abscess always include blood tests, urine tests.
A blood test will indicate the presence of a pronounced inflammatory process: an increasing leukocytosis with a shift of the leukocyte formula to the left, accelerated ESR is detected.
Instrumental diagnosis can be represented by ultrasound examination of the abdominal cavity, X-ray examination, and in complex cases - diagnostic puncture, laparocentesis (peritoneal perforation with removal of fluid) and laparoscopy.
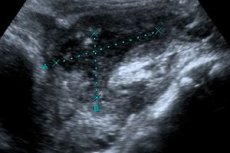
Sonographic evidence of appendicular abscess is the presence of anehogenous formation with irregular contours, with detection of detritus in its lumen. If the abscess is not large, then it is difficult to distinguish it from the bowel loops. To clarify the diagnosis, ultrasound is performed in dynamics to determine a clear intestinal configuration.
Differential diagnosis
Differential diagnosis of appendicular abscess is complex and is performed with the following diseases:
- with food poisoning (especially with the defeat of staphylococcal infection);
- with a preperforative state of peptic ulcer of stomach and duodenum;
- with perforation of the stomach ulcer;
- with a sharp attack of cholecystitis;
- with hepatic colic in cholelithiasis;
- with acute inflammation of the pancreas;
- with acute enterocolitis;
- with acute ileitis (nonspecific inflammation of the intestine);
- with diverticulitis and its perforation;
- with acute intestinal obstruction;
- with acute inflammatory process in the uterus and / or appendages, with intrauterine pregnancy;
- with pelvioperitonitis;
- with right-sided renal colic or right-sided pyelonephritis.
Treatment of the appendicular abscess
Delay in the treatment of appendicular abscess should not be, otherwise the abscess can break, which will invariably lead to the development of peritonitis. Categorically, it is impossible to drink laxatives, anti-inflammatory and pain medications with an appendicular abscess, and apply a warm water bottle to the stomach. At the pre-hospital stage, the patient should ensure peace with mandatory bed rest. You can apply cold to the stomach.
The only true and adequate treatment of appendicular abscess is urgent surgical intervention, which consists of removal of the abscess followed by the establishment of drainage. During surgery, the surgeon removes dead tissue and cleanses the purulent cavity.
In the period after the operation, antibiotic therapy is prescribed and the wound is washed with antiseptic solutions through the installed drains.
Medications for appendicular abscess
|
Ornidazole |
Enter intravenously, for 20 minutes, at a starting dose of 500-1000 mg every 12-24 hours. After normalization of the patient's condition, 500 mg of tablets are taken every 12 hours. During the administration of the drug, dyspepsia, drowsiness, and headaches may occur. |
|
Cefepim |
Usually Cefepime is administered 1-2 g intravenously every 12 hours, sometimes with the subsequent administration of metronidazole. When there are severe side effects in the form of skin rash, dyspepsia, fever, it is possible to change the dosage of the drug. |
|
Ciprofloxacin |
Take inside at 0.125-0.5 g twice a day, for 5-15 days. Ciprofloxacin is usually perceived by the body well, but it should not be ruled out that allergic reactions may develop. |
|
Ceftriaxone |
Assign 1-2 g daily. Duration of treatment is set individually. Sometimes during treatment with ceftriaxone there is an upset stomach, the picture of blood changes. As a rule, such phenomena occur after the drug is discontinued. |
Vitamins
After the operation, during the rehabilitation period, the doctor will prescribe vitamins to speed up healing and restore intestinal flora. To maintain the body, experts advise drinking compotes from dried fruits, rose hips, etc. Additionally, you can take B vitamins, ascorbic acid, vitamin A.
Rapid recovery after surgery is facilitated by the intake of vitamin-mineral complex preparations:
- Vitrum is a multivitamin complex which is most suitable for improving the state of the organism in the postoperative period, as well as intensive treatment with antibiotics and other potent drugs. Vitrum is taken immediately after a meal, 1 tablet daily for several months.
- The alphabet is a multivitamin and polymineral agent that perfectly compensates for the increased demand for minerals and vitamins in a critical period for the body. In day take three tablets of different color, maintaining a time interval between receptions in 4 hours. The alphabet is taken with food, for at least one month.
- Supradin is a drug recommended by doctors during illness and rehabilitation. Supradin is well absorbed in the body, thanks to the effervescent form - it is enough to take 1 effervescent tablet a day, before dissolving it in 100 ml of water.
- Perfectil is a vitamin and mineral complex preparation that accelerates the regeneration of cells, normalizing cellular metabolism, which possesses wound healing, antioxidant and dermatoprotective abilities. Perfectil take 1 capsule daily, after meals, preferably in the first half of the day.
Physiotherapeutic treatment
After surgery for appendicular abscess, a number of effective methods of physiotherapy are used, which helps to speed up the rehabilitation of patients. In this case, physical procedures that have a thermal effect are used very carefully.
First of all, physiotherapeutic procedures should be aimed at stimulating the healing process in the surgical intervention zone:
- infrared laser treatment;
- ultrasound treatment;
- peloidotherapy;
- low-frequency magnetotherapy;
- DMV treatment.
If the goal is to eliminate pain, then low-frequency electrotherapy, galvanization and medical electrophoresis are used.
In the future, spa treatment, balneotherapy, hydrotherapy are shown.
Alternative treatment
Alternative recipes are useful in the period of postoperative recovery. Proven means for years will help to establish digestion, eliminate constipation and diarrhea, restore appetite, strengthen immunity, and also stimulate the rapid healing of the wound.
- The root of ginger and fresh cloves of garlic are effective products for eliminating the effects of inflammation and for the normalization of digestive processes. If you add small amounts of grated ginger and garlic in the food 1-2 times a day, then you can quickly recover from serious diseases and surgeries.
- A huge benefit for the body will bring a mixture based on lemon juice and fresh honey. Such a mixture will improve digestion, strengthen immune defense. Daily enough to drink 2-3 cups of warm boiled water with the addition of 2 teaspoons of medicinal mixture.
- If you drink tea from burdock 3-4 times a day, you can prevent the development of the inflammatory process and improve overall health after the disease. Agrimony can be combined with a dandelion, but only if the patient does not take medications that lower blood pressure.
In a daily diet, it is recommended to inject fresh juices, especially from beets, carrots, spinach or cucumber, and also drink enough warm clean water to prevent constipation, which is highly undesirable during rehabilitation after an appendicular abscess.
 [43], [44], [45], [46], [47], [48], [49]
[43], [44], [45], [46], [47], [48], [49]
Herbal Treatment
In order to eliminate the effects of the inflammatory process and alleviate the pain, it is possible to apply the treatment with medicinal plants. Infusions and herbal teas are a good and affordable remedy that will bring invaluable benefits to the body.
- Tincture of wormwood can help at any stage of inflammation: in the morning before breakfast and at night should take 20 drops of tincture in 100 ml of water.
- Grass clover in an amount of 1 tbsp. L. Pour 300 ml of boiling water and leave for 20 minutes. Drink three times a day for 100 ml after eating.
- Prepare a medicinal mixture from the same parts of the leaves of strawberries, raspberries and yarrow. Brew 2 tbsp. L. Mix in 1 liter of boiling water, insist for a quarter of an hour and drink throughout the day.
An anesthetizing and soothing effect is also enjoyed by teas based on mint, thyme, cumin, chamomile. Such teas are brewed instead of the usual black or green tea and drunk a little during the day. Such treatment can be continued for several weeks in a row.
Homeopathy
After surgery, you can connect homeopathic medicines:
- Lakhiesis - 6-hundredth dilution, 2 granules per 10 days;
- Bellis Perrenis - with severe postoperative pain, in low and medium dilutions, depending on the severity of the patient's condition;
- Hypericum - with severe postoperative pains and paresthesias, 6 or 30-hundredth dilution, depending on the severity of the patient's condition;
- Gepar Sulfur - to limit purulent inflammation and improve the evacuation of pus, 3 or 6-hundredth dilution, depending on the individual characteristics of the patient.
Of course, homeopathy can not and should not replace traditional medicine, but it effectively complements it, contributing to the rapid recovery of the body, without undue burden and side effects.
Operative treatment
Features of surgical treatment of appendicular abscess are determined depending on its localization.
Most often, a skin incision of about 10 cm is done above the right inguinal ligament near the iliac crest and the superior-anterior iliac bone. The skin, subcutaneous tissue, fascia and external oblique abdominal muscle are dissected. On the fibers, the internal oblique and transverse muscle is divided.
Using the finger, the volume and localization of the abscess are examined. The appendix is removed only with its absolute availability, since there is a risk of getting pus inside the abdominal cavity.
The purulent cavity is cleaned and drained by placing a tube wrapped in a gauze swab to prevent the formation of decubitus on the wall of the inflamed caecum. The tube is fixed to the skin, mainly in the lumbar region.
After the operation, the treatment is directed to prevent possible complications and activation of the body's defenses.
Dissection of appendicular abscess in Pirogov
As a rule, an appendicular abscess is opened with the use of extraperitoneal access according to Pirogov, or according to Volkovich-Dyakonov.
An autopsy according to Pirogov is used for an abscess located in the depth of the right iliac region. The surgeon dissects the anterior abdominal wall to the parietal peritoneum, in the direction from top to bottom and from the right to the left, about 10 mm medial to the upper horizontal awn of the ilium, or 20 mm lateral to the Volkovich-Dyakonov incision. After this, the parietal peritoneum is separated from the inner region of the ilium, exposing the external side of the ulcer.
Autopsy by Volkovich-Dyakonov is performed with an appendicular abscess adjoining the anterior abdominal wall.
After the abscess is opened and sanitized, if an appendix is found in it, it is removed. Install a tampon and drainage in the purulent cavity. The abdominal wall is sutured to the drainage tube.
More information of the treatment
Prevention
In order to prevent the development of appendicular abscess, it is important to seek medical help for any acute pain in the abdomen.
The inflammatory process does not always flow clearly, so it is necessary to pay attention to other suspicious symptoms: increased gas production, fever, nausea, or diarrhea.
You can not let your health go by itself. Sometimes simple precautions help save a person's life. If you contact doctors in a timely manner, you can treat any disease at an early stage, not allowing a number of possible adverse complications.
Forecast
In the course of the inflammatory purulent process, spontaneous dissection (rupture) of the appendicular abscess can occur in the lumen of the intestine, into the abdominal cavity or behind the peritoneum, less often into the bladder or vaginal cavity, and even less often outwards. Therefore, the course of acute illness can be complicated, and such complications are extremely unfavorable for the health and life of the patient.
Proceeding from this, the prognosis of such a pathology, as an appendicular abscess, is considered very serious. Its consequences completely depend on how timely and competent medical care was, how well and in a timely manner the operation was carried out.

