Pneumocystis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Pneumocyst is the causative agent of respiratory disease of the lungs, which occurs in people at risk. This disease is not typical for healthy people, since the pathogen is opportunistic. The prevalence of pneumocystis pneumonia among the population is low, but among people with primary immunodeficiency states this pathology is very common: in patients with leukemia, lymphogranulomatosis, other oncopathologies, with congenital immunodeficiency, and with HIV infection. In patients with AIDS, pneumocystosis is a "marker" of the disease and occurs in more than half of the infected.
Structure of pneumocysts
Pneumocystis carinii is a microorganism that was isolated from the patient from the respiratory tract in the bronchi at the site of the bifurcation (carina), from which the name of this species originated. This pathogen naturally lives in the lungs of many animals, as well as in some people, from which the infection occurs. The path of infection is airborne. However, people with normal immune status may not be sick, but only carriers, since the pneumocyst is opportunistic. In immunodeficient conditions, clinical symptoms of the disease develop.
When studying the structure of this microorganism, there were many discussions as to which kingdom to include this species. Features of the structure of RNA, mitochondria, protein membrane structures allowed to classify as Fungi, but the absence of ergosterol and life cycle features confirm that the pneumocyst is the most sparing.
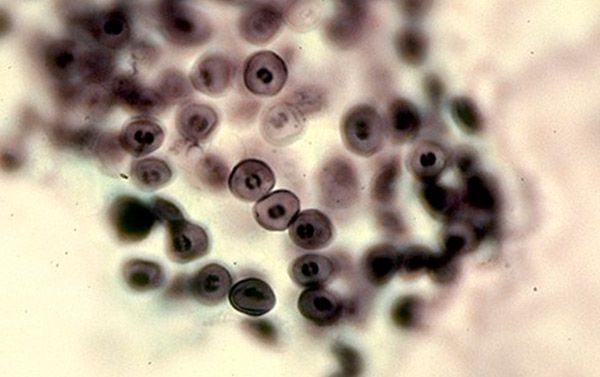
The structure of pneumocyst is not so simple. This is due to the inconstancy of the structure of cellular elements due to the complex cell cycle. The dimensions of the simplest range from 1 to 10 micrometers, depending on the stage of the cycle. Therefore, the microscope can take various forms - from small forms with a thin cell wall to large ones with a thicker wall.
Pneumocyst belongs to extracellular parasites and is localized mainly in alveolocytes of the first and second order. A microorganism can exist in four main forms: trophozoite, pre-cyst, cyst, and sporozoite.
Trophozoite is a form of existence that is characterized by a significant diameter of the cell and an irregular shape. The shell is thick and has outgrowths in the form of pseudopodia, therefore the form of trophozoite is unstable. These structures are designed for close contact of the pathogen with the alveolocyte cell. Inside the cell is a cytoplasm with organelles characteristic of many microorganisms: mitochondria, fish-farms, vacuoles with cell sap and lipid and carbon components. The core takes up enough space and is surrounded by two membranes to protect the genetic material.
Precesses are oval in shape without outgrowth, small size and thin cell membrane. In the middle of these structures, the nuclei are divided into cysts.
Cysts are also round in shape, but their size is larger, since there are special bodies inside - precursors of sporozoite. Cysts have a shell and a thick three-layer membrane, which after the rupture has an irregular shape and thus the cycle repeats.
The pneumocyst is multiplied by simply dividing the genetic material into two parts, and then dividing the contents of the cytoplasm with the envelope.
Life Cycle Pneumocystis
Pneumocyst is a post-cellular parasite, but at the same time, various forms of existence allow to penetrate and inside the cell. Infection occurs by airborne droplets. The human body gets a cyst, which, with a sufficient immune response, is rendered harmless by immunocompetent cells. If not, the cyst grows and continues its development cycle further with the formation of mature forms. The whole cycle can be divided into two phases - sexual and non-sexual.
The life cycle of the pneumocyst is quite complex and passes in stages several life forms: trophozoite, pretsist, cyst, sporozoite. Trophozoite is a vegetative form that attaches itself to the alveolocyte by its pseudopodia and closely interacts with the cell membrane. Then, by means of cell division, two mature cells are formed, and thus multiplication occurs. This is the so-called incomplete phase of pneumocyst development.
From the trophozoite, a precyst is formed, which has a huge nucleus and nutrients around it necessary for the future cyst. When time passes, the nucleus is divided and a cyst is formed, which usually has 8 cores inside. Microorganisms - sporozoites - leave the cyst. They have a single set of genetic information, and when they merge with each other, it turns out again that trophozoite, and the cycle of development is repeated again. This is the sexual phase of development.
Cysts, when they enter the human body, are localized on the alveoli. With intensive multiplication of trophozoites and cysts, more and more alveolocytes are desquamated, then clinical manifestations occur. The first immune reactions to this process develop due to cellular immunity. Macrophages and T helper cells react to foreign agents and try to phagocyte them, but the cysts have the ability to be inside the macrophage and not be exposed to the action of its lysosomal enzymes. Therefore, the cellular immune response is not sufficient for a complex immune response and elimination of pneumocysts. When triggered by cascade mechanisms under the influence of T-helpers, the humoral link of immunity, immunoglobulins affect trophozoites and infected macrophages. That is why, in people with pathology of the immune response, this disease develops very quickly, because adequate protection requires a good level of both local cellular and humoral immunity.
Symptoms of Pneumocystis pneumonia
The incubation period of the disease is from one week to five. It depends on the age and the degree of immunosuppression of the body. Often the disease can proceed according to the type of usual acute respiratory disease, then the clinical signs are poorly expressed and a person can die on the background of an easy current.
Considering the morphological changes in the lungs, several clinical stages are distinguished:
- stage of edema - occurs during the onset of infiltrative changes and is characterized by symptoms of intoxication, an increase in respiratory disorders.
- stage atelectasis - a violation of the outflow of secretions from the alveoli promotes their adhesion and the development of lung atelectasis. Clinically, cough occurs, and respiratory failure increases.
- stage of emphysema - lasts indefinitely, which depends on the effectiveness of treatment. Symptoms decrease, but residual effects in the lungs in the form of emphysematous bulls give a boxed sound with percussion.
Symptoms of pneumocystis pneumonia are different in adults and children. Children can get sick in case of prematurity, pathology of the central nervous system, perinatal injuries, intrauterine infections. The disease in this case develops for 3-4 months of the child's life. Then the child loses weight, refuses from the breast, his sleep is broken, symptoms of respiratory distress and perioral cyanosis appear. The child coughs like a whooping cough sometimes with a sputum-spitting phlegm. On the roentgenogram, there may be changes in the type of interstitial infiltrates or by the type of "cloudy" lungs.
In adults, clinical signs develop one week after infection, in the case of patients receiving immunosuppressant treatment, and after 2-3 months in patients with AIDS. The disease begins with fever to subfebrile digits, mild cough, shortness of breath with physical activity and pain in the chest area. A week later, in the absence of treatment, the symptoms intensify, cyanosis, high fever. The severe course of the disease is due to the rapid diffuse spread of inflammation to both lungs. This increases respiratory failure and against the background of general immunosuppression is dangerous with pulmonary edema.
In HIV-infected features of pneumocystosis - a lingering development of the symptoms of the disease, which often contributes to the fulminant course with a fatal outcome. Therefore, patients with AIDS have definite indications for the beginning of preventive treatment of PCP even if there are no special clinical manifestations.
Diagnosis of pneumocystis infection
Given the fact that the symptoms of PCP are not specific and often the disease occurs without significant clinical manifestations, but with a fulminant course, etiologic verification is very important in this case for timely treatment.
Clinical manifestations are not pathognomonic, therefore, according to the history and objective examination, the doctor can determine only the presence of pneumonia, and its nature is difficult to suspect.
An important fact of the anamnesis is the presence of the patient oncopathology, treatment with cytostatics, HIV infection. This allows you to suspect this particular type of pneumonia against the background of a significant decrease in the reactivity of immunity. Therefore, it is important that such a contingent of patients carefully investigate and carry out preventive measures.
Therefore, laboratory and instrumental diagnostic methods are leading in the verification of the diagnosis.
Radiography of the lungs is an obligatory method of diagnosis and confirmation of pneumonia. Characteristic changes are a phenomenon of "white lung" or "cloud lung", but these symptoms are not so common and in the initial stages these changes do not yet develop. In children, pneumocystosis can be expressed on the roentgenogram according to the type of interstitial pneumonia.
Bronchoscopy is recommended for carrying out flushing from the bronchi and further investigation of the secret.
Pneumocysts in sputum can be detected with a significant amount in the alveoli. Sputum examination is one of the reliable methods for verifying the diagnosis. The material for research other than sputum may be broncho-alveolar flushing. Use a microscopic method with the coloring of the material by Romanovsky-Giemsa, and in this case violet cells with a red core are detected. But this method does not always give a result, since a sufficient number of pathogens could not get under the microscope objective. A more precise method is parasitological. The material obtained from the patient is sown on a life-giving medium and the pathogen grows in a few days, which confirms the diagnosis.
These methods are rarely used in modern conditions, since it takes a long time before the result is obtained, and a laboratory with equipment is needed, which is not available in every medical institution. Therefore, at the present time, methods of serological diagnosis are common.
An analysis of the qualitative definition of pneumocysts can be carried out with the study of not only sputum, but also blood. The polymerase chain reaction method is used - a molecular genetic method based on the detection of DNA in a patient's material.
A simpler serological method (blood serum test) is the detection of antibodies to pneumocysts. Since immunoglobulins are produced on the pathogen, their level or presence indicates the activity of the process. The level of immunoglobulins of class G and M is determined by the method of enzyme immunoassay or imunofluorescent method. An increased level of immunoglobulins of class M indicates an acute infection, and with an increase in immunoglobulin G - a prolonged chronic infection is possible.
Treatment and prevention of pneumocystis
Treatment of this disease is a complicated task, since antibiotics do not act on the pathogen. In addition, treatment should be started as early as possible and only specific. Before the beginning of therapy it is necessary to determine the severity of the disease, which is characterized by the degree of respiratory insufficiency by the level of the partial pressure of oxygen in the blood.
The etiological treatment of pneumocystis is the use of sulfamethoxazole / trimethoprim - biseptol. For mild purposes, oral administration of the drug or intravenous infusion at a dose of 100 mg / kg and 20 mg / kg, respectively. However, given the presence of concomitant immunodeficiency in patients, these drugs cause many side effects: skin rash, anemia, leukopenia, agranulocytosis, nausea, dyspeptic manifestations. Therefore, the optimal course of treatment is 2 weeks.
In severe course, Pentamidine is added to this drug, a drug that has a specific effect, as it damages the reproductive systems of pneumocysts. It is used in a dose of 4 mg / kg when diluted in 5% glucose. The course of treatment is 2-3 weeks.
This is only etiotropic therapy, but also symptomatically antipyretic agents, detoxification therapy, rehydration, antifungal drugs and antibiotics for HIV-infected people.
Prevention of pneumocystis is necessary due to the complexity of the disease and the complicated course of it in a contingent of patients. Methods of prevention can be nonspecific and specific - medicamentous. Nonspecific methods of prevention are characterized by conducting a survey of patients at risk in the case of epidemiological indications, as well as correct and correct antiretroviral therapy in patients with AIDS. For such people, the correct regime of the day, sufficient food, exclusion of bad habits is of great importance.
Specific methods of prevention - is the use of etiotropic medicines. Use for prophylaxis the same drugs as for treatment. Indication for such primary prevention is the level of CD4 cells below 300, since this is considered a level of risk of pneumocyst damage.
Pneumocyst is the causative agent of a very complex disease, which, without specific clinical signs, needs to be diagnosed at the initial stage and to prescribe the right treatment, since the consequences can be very serious. Pneumocystisia develops in people with primary or secondary immunodeficiencies and these conditions are mutually damaging. Therefore, in certain groups of patients it is necessary to prevent this disease both by specific and non-specific methods.


 [
[