Histoplasm - the causative agent of histoplasmosis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Histoplasmosis is a natural focal deep mycosis characterized by a predominant airway disease. There are American (H. Capsulatum) and African (N. Duboisii) histoplasmosis, which is recorded only on the African continent. For the latter, lesions of the skin, subcutaneous tissue and bones in rural residents, as well as in persons in contact with soil and dust. In addition to humans, in natural conditions this mycosis is ached by baboon monkeys.
The causative agents of histoplasmosis are Histoplasma capsulatum and H, duboisii.
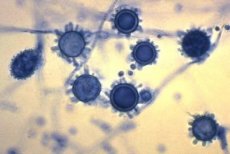
Histology of histoplasm
Dimorphic gibbs. The mycelial phase is represented by a septate mycelium with a thickness of 1-5 μm, microconidia spherical or pyriform in diameter 1-6 μm in diameter, tuberous macroconidia with a diameter of 10-25 μm. At 35-37 ° C, they grow in the form of yeast cells, the dimensions of which are in H. Capsulatum 1.5-2x3-3.5 μm: and in H. Duboisii - 15-20 μm.
The cultural properties of the histoplasm
Colonies yeast-glossy shiny, soft consistency. The optimal growth temperature is 25-30 ° C, pH 5.5-6.5, but it is possible to grow at wide pH ranges of 5.0-10.0. Biochemical activity is low.
Antigenic structure of histoplasm
Has common antigens with Blastomyces dermatitidis. Has antigen of yeast and mycelial (histoplasmin) phases. When growing on a liquid medium for 3 days, the mycelial form produces the antioxidants h, m, which can be determined by immunodiffusion in the gel. Pathogenicity factors are microconidia, hydrolases, cell wall polysaccharides.
Ecological niche of histoplasm
The natural habitat is the soil. The fungus grows well in soil polluted by droppings of birds and bats, where it grows in the form of a motel.
 [12], [13], [14], [15], [16], [17], [18], [19]
[12], [13], [14], [15], [16], [17], [18], [19]
Ecology
N. Duhoisii is insufficiently studied, reports on the isolation of this species from the soil are of a single nature.
Sustainability in the environment
Microconidia have high resistance in the external environment, retaining viability in dry soil for about 4 years, in water at 4 ° C - about 600 days.
Sensitivity to antibiotics
Sensitive to amphotericin B and ketoconazole. Sensitivity to antiseptics and disinfectants, Sensitive to the effects of commonly used antiseptics and disinfectants.
Epidemiology of histoplasmosis
Histoplasmosis is a sapronosis. The source of the causative agent of infection for humans and animals is the soil of endemic zones. Endemic areas are extinct in North, Central, South America, the Caribbean, South Africa, India, Southeast Asia, New Zealand and Australia. Sick people and animals are not contagious to others. The transmission mechanism is aerogenic, the transmission path is air-dust. The susceptibility of the population is universal. In case of epidemic outbreaks, contact of the diseased with the ground is detected. The epidemiology of African histoplasmosis has not been adequately studied.
Symptoms of histoplasmosis
Symptoms of histoplasmosis depend on the immune status of the body: acute forms are observed in children due to the peculiarities of their immune system, chronic disseminated forms, as a rule, develop against a background of insufficiency of the cellular link of immunity. Histoplasmosis manifestations can vary from acute pulmonary infection, resulting in spontaneous recovery, to chronic cavernous histoplasmosis and generalization of infection.
Laboratory diagnostics of histoplasmosis
The investigated material is pus from ulcerative lesions of the skin and mucous membranes, sputum, blood, urine, cerebrospinal fluid, punctate bone marrow, spleen, liver, lymph nodes, subcutaneous tissue.
For laboratory diagnostics use microscopic, mycological, biological, serological, allergological and histological methods. Work with the pathogen is carried out in laboratories of especially dangerous infections.
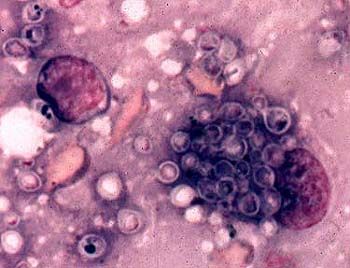
Microscopic examination of pus and exudate allows detecting histoplasm in hyperplastic cells of the system of mononuclear phagocytes in the form of oval yeast-like cells 10-15 μm in size, located extracellularly or inside monocytes and macrophages. Smears stained by Romanovsky-Giemsa.
To isolate a pure culture, the test material is inoculated on a Saburo medium, serum or blood agar, and also infects chick embryos. To stimulate growth in the medium, thiamine is added, to inhibit bacterial growth, penicillin and streptomycin. A part of the crops is cultivated at 22-30 ° C. And the other at 37 ° C for 3 weeks. The isolated culture is identified by morphological features and bioassay results in mice. Identification of a biphasic fungus with the characteristic morphology of the mycelial phase (thin septate mycelium, microconidia and bumpy macroconidia), and colonies consisting of small cells, makes it possible to identify H. Capsulation.
The isolation of only the mycelial form of the fungus requires proof of its dimorphism. Transformation is achieved either by cultivation of mycelial elements at 30-35 ° C, or by intraperitoneal infection of mice, which die at the 2-6th week, and small yeast is detected in the internal organs.
A pure culture is isolated by intraperitoneal infection of white mice or golden hamsters. After a month, the animals are slaughtered, the chopped liver and spleen are inoculated into Saburo's medium with glucose and the pathogen is grown for 4 weeks at 25, 30 and 37 ° C.
Isolation of culture in primary histoplasmosis is difficult due to minimal changes in the lungs, so in such cases it is necessary to focus on the results of serological reactions, of which RP and RSK with histoplasmin are most effective, RP, immunodiffusion and latex agglutination are positive for 2-5 weeks after infection. Later, a positive RSK, whose titers increase when generalizing the infection, is detected.
A positive intradermal test with histoplasmin (1: 100) appears at an early stage of the disease and persists for many years. Diagnostic value is only the transition of a previously negative reaction to a positive one. Histoplasmic intradermal test can stimulate antigenigenesis, so it is put after serological studies.
For histological examination, slice preparations are stained with Schiff's reagent, but the clearest results are obtained by the Gomory-Grokott method: yeast cells are stained black or brown. The causative agent can be found in the cytoplasm of lymphocytes, histiocytes in the form of small rounded single or budding cells.

