Medical expert of the article
New publications
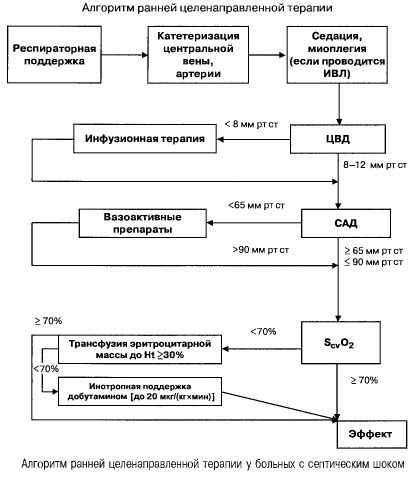
Treatment of severe sepsis and septic shock
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Effective treatment of sepsis is possible only with full surgical sanitation of the infection site and adequate antimicrobial therapy. Inadequate initial antimicrobial therapy is a risk factor for death in patients with sepsis. Maintaining the patient's life, preventing and eliminating organ dysfunctions are possible only with targeted intensive care.
Its main goal is to optimize O2 transport under conditions of its increased consumption, which is typical for severe sepsis and septic shock. This treatment is implemented through hemodynamic and respiratory support.
Hemodynamic support
Infusion therapy
Infusion therapy is one of the initial measures to maintain hemodynamics and, above all, cardiac output. Its main tasks in patients with sepsis are:
- restoration of adequate tissue perfusion,
- correction of homeostasis disorders,
- normalization of cellular metabolism,
- reduction in the concentration of septic cascade mediators and toxic metabolites.
In sepsis with multiple organ failure and septic shock, they try to quickly (within the first 6 hours) achieve the following values of important indicators:
- hematocrit >30%,
- diuresis 0.5 ml/(kgh),
- blood saturation in the superior vena cava or right atrium >70%,
- mean blood pressure >65 mm Hg,
- CVP 8-12 mm Hg
Maintaining these values at the specified level improves patient survival (category of evidence B). Hemodynamic monitoring using a Swan-Ganz catheter and PICCO technology (transpulmonary thermodilution and pulse wave analysis) expand the possibilities for monitoring and assessing the effectiveness of hemodynamic therapy, but there is no evidence that they improve survival.
The optimal preload value is selected individually, since it is necessary to take into account the degree of endothelial damage and the state of lymphatic drainage in the lungs, diastolic function of the ventricles, and changes in intrathoracic pressure. The volume of infusion therapy is selected so that the PCWP does not exceed the plasma COP (prevention of OL) and there is an increase in CO. Additionally, the parameters characterizing the gas exchange function of the lungs (paO 2 and paO 2 /FiO 2 ) and changes in the radiographic picture are taken into account.
For infusion therapy as part of the targeted treatment of sepsis and septic shock, crystalloid and colloidal solutions are used with virtually identical results.
All infusion media have both advantages and disadvantages. Today, given the results of experimental and clinical studies, there is no reason to prefer any particular type.
- For example, for adequate correction of venous return and preload level, it is necessary to administer a volume of crystalloids 2-4 times greater than that of colloids, which is associated with the peculiarities of solution distribution in the body. In addition, crystalloid infusion is associated with a greater risk of tissue edema, and their hemodynamic effect is shorter than that of colloids. At the same time, crystalloids are cheaper, do not affect the coagulation potential and do not provoke anaphylactoid reactions. Based on the above, the qualitative composition of the infusion program is determined depending on the patient's characteristics, taking into account the degree of hypovolemia, the phase of DIC syndrome, the presence of peripheral edema and the concentration of albumin in the blood serum, the severity of acute lung injury.
- Plasma substitutes (dextrans, gelatin preparations, hydroxyethyl starch) are indicated in cases of severe BCC deficiency. Hydroxyethyl starches with a substitution degree of 200/0.5, 130/0.4, and 130/0.42 have a potential advantage over dextrans due to a lower risk of membrane escape and the absence of a clinically significant effect on hemostasis.
- The introduction of albumin in critical conditions may increase the risk of death. The increase in COP during its infusion is transient, and then, under conditions of increased permeability of the capillary bed (the "capillary leak" syndrome), further extravasation of albumin occurs. It is possible that albumin transfusion will be useful only if its concentration in the serum is less than 20 g / l and there are no signs of "leakage" into the interstitium.
- The use of cryoplasm is indicated for consumption coagulopathy and decreased coagulation potential of the blood.
- The widespread use of donor red blood cell mass should be limited due to the high risk of developing various complications (APL, anaphylactic reactions, etc.). According to most experts, the minimum hemoglobin concentration in patients with severe sepsis is 90-100 g/l.
Correction of hypotension
Low perfusion pressure requires immediate activation of drugs that increase vascular tone and/or inotropic function of the heart. Dopamine or norepinephrine are the first-line drugs for correction of hypotension in patients with septic shock.
Dopamine (dopmin) at a dose of <10 mcg/(kg x min) increases BP, primarily by increasing CO, and has a minimal effect on systemic vascular resistance. At high doses, its a-adrenergic effect predominates, leading to arterial vasoconstriction, and at a dose of <5 mcg/(kg x min) dopamine stimulates dopaminergic receptors of renal, mesenteric, and coronary vessels, leading to vasodilation, increased glomerular filtration, and Na+ excretion.
Norepinephrine increases mean arterial pressure and increases glomerular filtration. Optimization of systemic hemodynamics under its action leads to improvement of renal function without the use of low doses of dopamine. Studies in recent years have shown that its isolated use, compared with a combination with high doses of dopamine, leads to a statistically significant decrease in mortality.
Adrenaline is an adrenergic drug with the most pronounced hemodynamic side effects. It has a dose-dependent effect on heart rate, mean arterial pressure, cardiac output, left ventricular function, and O2 delivery and consumption . However, tachyarrhythmias, deterioration of organ blood flow, and hyperlactatemia occur simultaneously. Therefore, the use of adrenaline is limited to cases of complete refractoriness to other catecholamines.
Dobutamine is the drug of choice for increasing CO and O2 delivery and consumption at normal or elevated preload. Due to its predominant action on beta1-adrenergic receptors, it is more effective than dopamine in increasing these parameters.
Experimental studies have shown that catecholamines, in addition to supporting blood circulation, can regulate the course of systemic inflammation by influencing the synthesis of key mediators with a distant effect. Under the influence of adrenaline, dopamine, noradrenaline and dobutamine, activated macrophages reduce the synthesis and secretion of TNF-a.
The selection of adrenergic agents is carried out according to the following algorithm:
- cardiac index 3.5-4 l/(min x m 2 ), SvO 2 >70% - dopamine or norepinephrine,
- cardiac index <3.5 l/(min x m 2 ), SvO 2 <70% - dobutamine (if systolic blood pressure <70 mm Hg - together with norepinephrine or dopamine).
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ]
Respiratory support
The lungs are among the first target organs involved in the pathological process in sepsis. Acute respiratory failure is one of the leading components of multiple organ dysfunction. Its clinical and laboratory manifestations in sepsis correspond to ALI, and with the progression of the pathological process - ARDS. Indications for mechanical ventilation in severe sepsis are determined depending on the severity of parenchymatous respiratory failure (ARF or ARDS). Its criterion is the respiratory index:
- <200 - tracheal intubation and respiratory support are indicated,
- >200 - readings are determined individually.
If the patient is conscious during spontaneous breathing with oxygen support, there is no high expenditure on the work of breathing and pronounced tachycardia (HR <120 per minute), the normal value of venous return S O 2 >90%, then it is possible to refrain from transferring him to artificial ventilation. However, it is necessary to carefully monitor the patient's condition. The optimal value of S O 2 is about 90%. It can be maintained by various methods of gas delivery (face masks, nasal catheters) in non-toxic concentrations (FiO 2 <0.6). Non-invasive artificial ventilation is contraindicated in sepsis (category of evidence B).
High-volume mechanical ventilation (MVV) modes (VO = 12 ml/kg) should be avoided, since in such cases the secretion of cytokines by the lungs increases, which leads to aggravation of MOF. It is necessary to adhere to the concept of safe mechanical ventilation, which is possible if the following conditions are met (category of evidence A):
- DO <10 ml/kg,
- non-inverted ratio of inhalation and exhalation,
- peak airway pressure <35 cm H2O,
- FiO 2 <0.6.
The selection of respiratory cycle parameters is carried out until adequate mechanical ventilation is achieved, its criteria are paO2 > 60 mm Hg, SpO2 > 88-93%, pvO2 35-45 mm Hg, SvO2 > 55%.
One of the effective methods for optimizing gas exchange is performing artificial ventilation in the prone position (Prone Positioning) (category of evidence B). This position is effective in patients in the most severe condition, although its effect on reducing mortality in the long-term period is statistically insignificant.
Nutritional support
Conducting artificial nutritional support is an important element of treatment, one of the mandatory measures, since the development of the syndrome of multiple organ failure in sepsis is usually accompanied by manifestations of hypermetabolism. In such a situation, energy needs are met by the destruction of one's own cellular structures (autocannibalism), which aggravates organ dysfunction and increases endotoxicosis.
Nutritional support is considered as a method of preventing severe exhaustion (protein-energy deficiency) against the background of a pronounced increase in cata- and metabolism. Inclusion of enteral nutrition in the complex of intensive therapy prevents the movement of intestinal microflora, dysbacteriosis, increases the functional activity of enterocytes and the protective properties of the intestinal mucosa. These factors reduce the degree of endotoxicosis and the risk of secondary infectious complications.
Calculation of nutritional support:
- energy value - 25-35 kcal/(kg body weight x day),
- amount of protein - 1.3-2.0 g/(kg body weight x day),
- amount of carbohydrates (glucose) - less than 6 g/kg/day,
- amount of fat - 0.5-1 g/kg/day,
- glutamine dipeptides 0.3-0.4 g/kg/day,
- vitamins - standard daily set + vitamin K (10 mg/day) + vitamins B 1 and B 6 (100 mg/day) + vitamins A, C, E,
- microelements - standard daily set + Zn (15-20 mg/day + 10 mg/day in the presence of loose stools),
- electrolytes - Na+, K+, Ca2+ according to balance calculations and concentration in plasma.
Early initiation of nutritional support (24-36 h) is more effective than on the 3rd-4th day of intensive therapy (category of evidence B), especially with enteral tube feeding.
In severe sepsis, there are no advantages of enteral or parenteral nutrition; the duration of organ dysfunction and the duration of respiratory and inotropic support are the same, and mortality rates are the same. Given the above, early enteral nutrition is a cheaper alternative to parenteral nutrition. The use of mixtures enriched with dietary fiber (prebiotics) for tube feeding significantly reduces the incidence of diarrhea in patients with severe sepsis.
For effective protein synthesis in the body, it is important to maintain the metabolic ratio "total nitrogen, g - non-protein calories, kcal" = 1-(110-130). The maximum dose of carbohydrates is 6 g / (kg of body weight per day), since the introduction of large doses threatens hyperglycemia and activation of catabolism in skeletal muscles. Fat emulsions are recommended to be administered around the clock.
Contraindications to nutritional support:
- decompensated metabolic acidosis,
- individual intolerance to nutritional support media,
- severe unrecovered hypovolemia,
- refractory shock - dopamine dose >15 mcg/(kg x min) and systolic blood pressure <90 mm Hg,
- severe intractable arterial hypoxemia.
Glycemic control
An important aspect of complex treatment of severe sepsis is constant monitoring of glucose concentration in blood plasma and insulin therapy. High glycemia and the need for its correction are factors of unfavorable outcome in sepsis. Given the above circumstances, normoglycemia (4.5-6.1 mmol/l) is maintained in patients, for which, when glucose concentration increases above acceptable values, insulin infusion is performed (0.5-1 U/h). Depending on the clinical situation, glucose concentration is monitored every 1-4 hours. When implementing this algorithm, a statistically significant increase in patient survival was noted.
 [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
[ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
Glucocorticoids
The results of modern studies regarding the effectiveness of glucocorticoid use in patients with septic shock are summarized in the following statements:
- it is inappropriate to use hormones in high doses [methylprednisolone 30-120 mg/(kg x day) once or for 9 days, dexamethasone 2 mg/(kg x day) for 2 days, betamethasone 1 mg/(kg x day) for 3 days] - increased risk of hospital infections, no effect on survival,
- The use of hydrocortisone at a dose of 240-300 mg per day for 5-7 days accelerates the stabilization of hemodynamic parameters, allows the withdrawal of vascular support and improves survival in patients with concomitant relative adrenal insufficiency (category of evidence B).
It is necessary to abandon the chaotic empirical prescription of prednisolone and dexamethasone - there are no grounds for extrapolating new information to them. In the absence of laboratory evidence of relative adrenal insufficiency, hydrocortisone at a dose of 300 mg per day (in 3-6 injections) is administered
- in refractory shock,
- if high doses of vasopressors are required to maintain effective hemodynamics.
It is possible that in conditions of systemic inflammation in septic shock, the effectiveness of hydrocortisone is associated with the activation of the nuclear factor kB inhibitor (NF-kB-a) and the correction of relative adrenal insufficiency. In turn, inhibition of the activity of the transcription nuclear factor (NF-kB) leads to a decrease in the formation of inducible NO synthetase (NO is the most powerful endogenous vasodilator), proinflammatory cytokines, COX and adhesion molecules.
Activated Protein C
One of the characteristic manifestations of sepsis is a disruption of systemic coagulation (activation of the coagulation cascade and inhibition of fibrinolysis), which ultimately leads to hypoperfusion and organ dysfunction. The effect of activated protein C on the inflammatory system is realized in several ways:
- reduction of selectin attachment to leukocytes, which protects the endothelium from damage, which plays a key role in the development of systemic inflammation,
- decreased release of cytokines from monocytes,
- blocking the release of TNF-a from leukocytes,
- inhibition of thrombin production (it potentiates the inflammatory response).
Anticoagulant, profibrinolytic and anti-inflammatory action
- activated protein C is due to
- degradation of factors Va and VIIIa - suppression of thrombus formation,
- suppression of plasminogen activator inhibitor - activation of fibrinolysis,
- direct anti-inflammatory effect on endothelial cells and neutrophils,
- protection of the endothelium from apoptosis
Administration of activated protein C [drotrecogin alfa (activated)] at 24 mcg/(kg h) for 96 h reduces the risk of death by 19.4%. Indications for administration: sepsis with acute MOF and high risk of death (APACHE II > 25 points, dysfunction of 2 or more organs, category of evidence B).
Activated protein C does not reduce mortality in children, patients with single-organ dysfunction, APACHE II < 25 points, in patients with non-surgical sepsis.
 [ 14 ], [ 15 ], [ 16 ], [ 17 ]
[ 14 ], [ 15 ], [ 16 ], [ 17 ]
Immunoglobulins
The advisability of intravenous administration of immunoglobulins (IgG and IgG+IgM) is associated with their ability to limit the excessive action of proinflammatory cytokines, increase the clearance of endotoxins and staphylococcal superantigen, eliminate anergy, and enhance the effect of ß-lactam antibiotics. Their use in the treatment of severe sepsis and septic shock is the only method of immunocorrection that increases survival. The best effect was recorded when using a combination of IgG and IgM [RR=0.48 (0.35-0.75), category of evidence A]. The standard dosing regimen is 3-5 ml/(kg x day) for 3 days in a row. When using immunoglobulins, the most optimal results were obtained in the early phase of shock ("warm shock") and in patients with severe sepsis (APACHE II score of 20-25 points).
Prevention of deep vein thrombosis
Prevention of lower extremity DVT significantly affects the treatment outcomes in patients with sepsis (category of evidence A). Both unfractionated and LMWH are used for this purpose. The main advantages of low-molecular-weight heparins are a lower incidence of hemorrhagic complications, a weaker effect on platelet function, and a long-lasting effect (can be administered once daily).
Prevention of the formation of stress ulcers of the gastrointestinal tract
This direction plays a significant role in a favorable outcome in the treatment of patients with severe sepsis and septic shock, since the mortality rate for bleeding from stress ulcers of the gastrointestinal tract is 64-87%. Without preventive measures, stress ulcers occur in 52.8% of critically ill patients. However, the use of proton pump inhibitors and histamine H2 receptor blockers reduces the risk by more than 2 times (the first group of drugs is more effective than the second). The main direction of prevention and treatment is maintaining pH within 3.5-6.0. It should be emphasized that in addition to the above drugs, enteral nutrition plays an important role in preventing the formation of stress ulcers.
Extracorporeal blood purification
Various biologically active substances and metabolic products involved in the development of generalized inflammation are targets for detoxification methods, which is especially important in the absence of natural hepatorenal clearance in conditions of multiple organ failure. Renal replacement therapy methods are considered promising, as they can affect not only uremic disorders in patients with renal failure, but also have a positive effect on other changes in homeostasis and organ dysfunctions that occur in sepsis, shock, and multiple organ failure.
To date, there is no data confirming the need to use extracorporeal blood purification methods as one of the main directions of pathogenetic therapy of sepsis and septic shock. Their use is justified in case of multiple organ failure with renal dominance.
 [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
Hemodialysis
The essence of the method is the diffusion of substances of low molecular weight (up to 5x10 3 Da) through a semipermeable membrane and the removal of excess fluid from the body along a pressure gradient. Hemodialysis is widely used to treat patients with both chronic and acute renal failure. The rate of diffusion of substances depends exponentially on their molecular weight. For example, the removal of oligopeptides is slower than their synthesis.
Hemofiltration
Hemofiltration is an effective method for removing substances with a molecular weight of 5x10 3 - 5x10 4 Da and the only way to remove a large group of biologically active substances and metabolites from the body. The method is based on the convection method of mass transfer. In addition to adequate correction of azotemia, hemofiltration effectively removes anaphylatoxins C3a, C5a, proinflammatory cytokines (TNF-a, IL-1b, 6 and 8), ß2-microglobulin, myoglobin, parathyroid hormone, lysozyme (molecular weight - 6000 Da), a-amylase (molecular weight - 36,000-51,000 Da), creatine phosphokinase, alkaline phosphatase, transaminases and other substances. Hemofiltration removes amino acids and plasma proteins (including immunoglobulins and circulating immune complexes).
Hemodiafiltration
Hemodiafiltration is the most powerful method of blood purification, combining diffusion and convection (i.e., GD and GF). An additional contribution to the detoxification process is made by the sorption of pathological substances on the filter membrane.
Plasmapheresis
Plasmapheresis (plasma exchange, plasma filtration) is also considered as a possible method for correcting generalized inflammation in patients with sepsis and septic shock. The optimal method is considered to be the use of plasma exchange in a continuous mode with the removal of 3-5 volumes of plasma and its simultaneous replacement with fresh frozen, albumin, colloidal and crystalloid solutions. With a sieving coefficient of 1, plasma filtration ensures good removal of C-reactive protein, haptoglobin, complement fragment C3, 1-antitrypsin, IL-6, thromboxane-B2, granulocyte-stimulating factor, TNF. The use of sorbents to purify the patient's plasma reduces the risk of infection and reduces the cost of the procedure, since there is no need to use foreign proteins.
The use of prolonged infusion of sodium selenite (selenase) 1000 mcg/day in severe sepsis leads to a decrease in mortality.
Selenium is an essential microelement, the importance of which is associated with its key role in the antioxidant systems of cells. The level of selenium in the blood is maintained within 1.9-3.17 μM/l. The need for selenium is 50-200 μg per day, and it depends on the availability of other antioxidants and microelements.
Selenium is a powerful antioxidant, a component of glutathione peroxidase, phospholine glutathione peroxidase, other oxidoreductases and some transferases. Glutathione peroxidase is the most important link in the endogenous antioxidant system.
The effectiveness of selenium in critical conditions has been studied in recent years. These studies have shown that the main mechanisms of action of selenium are:
- suppression of NF-kB hyperactivation;
- decreased complement activation;
- its action as an immunomodulator, antioxidant and anti-inflammatory agent
- maintaining peroxide utilization;
- suppression of endothelial adhesion (reduced expression of ICAM-1, VCAM-2,
- E - selectin, P - selectin);
- protection of the endothelium from oxyradicals (using selenoprotein P, which prevents the formation of peroxynitrite from O2 and NO).
To summarize the above, we can define specific tasks of intensive care for severe sepsis:
- Hemodynamic support: CVP 8-12 mm Hg, mean BP >65 mm Hg, diuresis 0.5 ml/(kg h), hematocrit >30%, mixed venous blood saturation >70%.
- Respiratory support peak airway pressure <35 cm H2O, inspiratory fraction of oxygen <60%, tidal volume <10 ml/kg, non-inverted inspiratory to expiratory ratio.
- Glucocorticoids - "low doses" (hydrocortisone 240-300 mg per day).
- Activated protein C 24 mcg/(kg h) for 4 days in severe sepsis (APACHE II >25).
- Immunocorrection replacement therapy with pentaglobin.
- Prevention of deep vein thrombosis of the lower extremities.
- Prevention of the formation of stress ulcers of the gastrointestinal tract: use of proton pump inhibitors and H2-histamine receptor blockers.
- Replacement therapy for acute renal failure.
- Nutritional support: energy value of food 25-30 kcal/kg body weight x day), protein 1.3-2.0 g/(kg body weight x day), glutamine dipeptides 0.3-0.4 g/(kg x day), glucose - 30-70% of non-protein calories, provided that glycemia is maintained <6.1 mmol/l, fats - 15-50% of non-protein calories.

