Medical expert of the article
New publications
Staphylococcus aureus in the smear: consequences, treatment with folk remedies
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
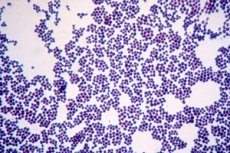
Today, one of the most discussed problems in medicine and laboratory diagnostics is staphylococcus in a smear. It is quite easy to detect, difficulties arise at the stage of interpreting the results. The fact is that staphylococcus is a representative of normal microflora and inhabits many biotopes of the human body, performing a number of useful functions. At the same time, under certain circumstances, it becomes the causative agent of many infectious diseases and pathological conditions. The emerging fine line between such conventional concepts as norm and pathology is increasingly becoming a subject of discussion for many doctors.
Staphylococcus in a smear in men
Staphylococcus in men is part of the normal microflora of the urogenital tract, respiratory tract, skin, and intestines. Microflora disorders in men are relatively rare, so autoinfections occur mainly if the body has been exposed to adverse effects from environmental factors. For example, microflora disorders can occur after taking antibiotics, after long-term hormone therapy, under the influence of stress, fatigue, and neuropsychic overstrain.
Another cause may be the entry of a pathogenic microorganism from outside. In order for an infectious process to develop in this case, the concentration of bacterial cells must be relatively high, and immunity must also be reduced.
Often men contract staphylococcal infections in hospitals and inpatient facilities, after surgeries, other invasive interventions, and in the presence of prostheses and catheters.
Staphylococcus in a smear in women
Women are more likely to have autoinfection, that is, an infection that develops inside the body. Since staphylococcus is part of the normal human microflora, it is always detected in a smear. It is important that its indicators are within the normal range. But under certain circumstances and conditions of the body, changes may occur that contribute to an increase in the amount of staphylococcus, which can cause an infectious and inflammatory disease.
Staphylococcus plays a leading role in maintaining the health of female reproductive organs. Vaginal biocenosis contains about 10% of the entire microflora of the body. Violation of normal biocenosis undermines the health of the unborn child.
Scientists have proven that it is staphylococcus that plays a leading role in pathology. One of the reasons is decreased immunity, endocrine disorders.
The vaginal microflora is largely determined by the hormonal status. It is they that significantly affect the selective advantages in the biotope of various representatives of the microflora. Under the influence of hormones of the estrogenic series, the vaginal membranes are saturated with glycogen, which is an optimal environment for the development of an anaerobic environment in which lactic acid bacteria, bifidobacteria, propionobacteria, and clostridial forms predominate. At the same time, the amount of aerobic and facultative aerobic microflora is limited. Thus, the degree of staphylococci does not exceed 103-104 in 1 ml of secretion. This is the composition of the obligate microflora, which is considered constant. It ensures the normal functioning of the system and protects against viral infections, inflammations, and tumor processes.
But, in addition to the obligate flora, the vaginal microflora also includes transient flora, which is formed by facultative microorganisms. Their species diversity is quite high, while the population level does not exceed 3-4%. Microorganisms are classified as opportunistic forms, since when the hormonal background, immune status, and various types of influences change, they act as pathogens of infectious and inflammatory processes. Staphylococcus aureus also falls into this group. A sharp increase in staphylococcus secretion can lead to the development of such pathological conditions as bacterial vaginosis, sepsis, genitourinary infections, and toxic shock syndrome.
Formation of microflora begins from the very birth of a girl. It is necessary to take into account that microbiocenosis is not a random set of microorganisms, but an evolutionarily formed defense system. Despite the fact that during various stages of a woman's life, the cenosis undergoes numerous changes, in general it remains homogeneous and genetically determined. The existing mechanism for regulating microflora depends on the level of hormones, and contributes to the fact that it changes, being in close connection with the phase of the menstrual cycle. Similar changes also appear during pregnancy, when the optimal species and quantitative composition of microbiocenoses is formed, manifested due to an intense "estrogen explosion".
Significant changes occur during childbirth, in the postpartum period, postmenopause. During this period of time, the amount of estrogen decreases sharply, which can lead to high susceptibility to infectious diseases and cause numerous infectious diseases. Negative effects from exogenous factors are also noted. Such factors include, for example, inadequate intake of medications, especially antibiotics. Tablets containing hormonal components, immunosuppressants, cytostatic drugs, and contraceptives also have a negative effect.
Staphylococcus in a smear during pregnancy
Pregnancy, from the point of view of microbiology, is the most favorable period when an optimal, natural vaginal microenvironment is formed. There is a sharp increase in the amount of glycogen in the walls, which is due to a surge in estrogenic activity. This contributes to the effective growth of lactobacilli, bifidobacteria. According to the results of numerous studies, the available data, the most favorable microenvironment is established by the third trimester. There is a sharp decrease in the number of pathogenic and opportunistic flora. Of particular interest is the information that the microflora is normalized not only in the vagina and reproductive organs, but also in the intestines, and in many other biotopes, for example, in the area of the skin, mammary glands. All changes that occur in the body of a pregnant woman (with normal health, adequate nutrition) are aimed at protecting the developing fetus. First of all, protection from the development of perinatal infection is required. This is ensured by maintaining colonization resistance at a high level. This can provoke the development of many purulent, inflammatory and infectious processes. With advanced pathology, even signs of bacteremia and septic manifestations are possible. In the postpartum period, the protective properties of the natural microflora decrease, the number of opportunistic flora increases, especially staphylococci. There is a very high probability of developing a staphylococcal infection, the risk of other infectious and inflammatory pathologies increases. The condition is normalized within 6 weeks of the postpartum period.
Staphylococcus in a smear in a child
The detection of staphylococcus indicates a possible infection or accidental entry of the microorganism into the microbiocenosis. It is impossible to give a definite answer, since it is necessary to take into account many factors that are closely intertwined.
It is important to understand that staphylococcus may be part of the normal microflora of a child. Pathology can only be discussed with a high degree of contamination. It is also necessary to take into account the age of the child. Thus, in children, the microflora is not fully formed. In newborns and children up to 3 years of age, the mother's microflora is preserved for a long time.
The process of formation of the microbial ecological system begins from the moment the fetus passes through the mother's birth canal, therefore the key role in the formation of the physiological microbiocenoses of the newborn is played by the endomicroecological status of the mother, first of all, the state of the vaginal microflora.
The most complex mechanism of bioengineering of the microbial ecological system is activated from the moment of birth of the child and is based on the cooperative activity of the newborn's organism, protective and bifidogenic factors of the mother's breast milk and her physiological microflora.
During childbirth, such factors as genetics, birth conditions, mother's health, medical personnel microflora, hospital microflora, and medications play an important role in the formation of microflora. After birth, the composition of breast milk, the composition of artificial formula, the conditions in which the newborn is kept, the use of drug therapy, probiotics, and prebiotics are of great importance.
Staphylococci and streptococci in a smear
Both microorganisms are found in various biotopes. They are considered as aerobic and facultative-anaerobic life forms. Normally, staphylococcus should not exceed 10 3 colonies in 1 ml of the test fluid, streptococcus – no more than 10 4.
In the normal state of the immune system, hormonal background, they help protect the skin and mucous membranes from colonization by pathogenic forms of microorganisms. If microecological conditions are violated (under the influence of negative internal and external factors), they can cause disease.
Staphylococci cause bronchitis, pneumonia, bacterial vaginosis, sepsis, genitourinary infections of various localizations, toxic shock syndrome.
Streptococci are also capable of causing bacterial pneumonia and vaginosis, sepsis, peritonitis, pyelonephritis, cystitis, urethritis, oophoritis, catheter-associated and hospital infections. Causes chorioamnionitis, premature birth and miscarriage.
Enterococci and staphylococci in smear
Enterococci are streptococci of serological group D. They are isolated on a special medium, which includes triphenyltetrazolium chloride, which, when split, gives the colonies a characteristic pink, red, or brown color. A distinctive feature of enterococci is their ability to split esculin and iron citrate. They differ from all other streptococci in their ability to grow on a medium containing 0.65% sodium chloride.
Often found together with staphylococcus, form biofilms. Participate in the formation of catheter-associated infections, are dangerous hospital strains, colonize purulent wounds, postoperative surfaces. Are frequent pathogens of intestinal diseases, food toxic infections, enteritis, dysbacteriosis.
E. coli and staphylococcus in a smear
It all depends on the biotope and the quantity of the microorganism. E. coli is a representative of the normal intestinal microflora, while staphylococcus is found in acceptable concentrations in all biotopes (the norm is no more than 10 3 -10 4 CFU/ml).
When E. coli gets into another, unnatural biotope for it, inflammation can develop. Thus, getting E. coli into the oral cavity can cause the development of phageitis, tonsillitis, stomatitis. Getting it into the vagina causes gynecological diseases. The latter is observed especially often due to the close location of the intestine (rectum and anus) and the vagina.
Complications and consequences
The most dangerous complication of detecting staphylococcus in a smear is a violation of eubiosis. Eubiosis is understood as the equilibrium position of the human body and its microbiota. In this state, human health is at the highest level and ensures the full functioning of the body. Under the influence of various factors, eubiosis is violated - dysbacteriosis, manifested in the development of microbiocenosis disorders in various biotopes. Changes affect exclusively endogenous microflora. If high concentrations of staphylococcus are detected in a smear, we are talking about a violation of the balance between microbionts. An increase in the number of one microorganism leads to a decrease in the number of other microorganisms. If some microorganisms die, their place is immediately taken by other forms. Most often, these are pathogenic microorganisms that act as causative agents of many infectious diseases. As a result, infectious and inflammatory, purulent-septic diseases develop, which entails a change in the physicochemical parameters of the biotope. This results in damage to the processes of assimilation of individual food components, disrupts motor skills, and creates conditions for further increase in the pathogen population.
Deep changes in microbial-tissue relationships can lead to the fact that the altered microbiocenosis becomes an additional, and in most cases, a decisive factor in aggression towards one's own organism. The danger is that some bacterial endotoxins, products of bacterial activity, are able to "mimic" the body's own antigens. Therefore, it is quite difficult to destroy them, and it is difficult to select an effective bacterial remedy. The consequence is serious disruptions to the normal state of the immune system, as well as the emergence of a conflict between the indigenous microflora and the immune system.
Particular attention in pathology is paid to the state of the intestinal microflora, since 60% of all human microflora is concentrated in it. In addition, the digestive tract most actively interacts with the environment.
When microflora is disturbed, its individual representatives can change their form and properties. Many acquire cytotoxic properties, acting toxically on the cells of the host organism. Inflammation develops rapidly, which promotes the translocation of living cells and their metabolites to other biotopes. We can talk about the generalization of the inflammatory process, the development of septicemia.
Especially dangerous is the detection of microorganisms in fluids that should normally be sterile, such as blood, urine, and cerebrospinal fluid. A small amount indicates bacteremia, in which pathogens penetrate the blood, going beyond the affected organs that are the source of infection. If the disease is not cured at this stage, the process will begin to progress, leading to the development of sepsis - "blood poisoning".
The danger of the formation of microecological disorders consists in an unfavorable change in the composition and protective properties of the indigenous microflora, and the local symptoms associated with this, but also in the possible development of severe multiple organ failure with all its consequences, a possible fatal outcome.
Dysbiotic changes are in many ways the trigger mechanism for many somatic conditions, the etiopathogenesis of which is associated with dysbiotic disorders.
The main pathologies that arise from microbiota disorders with a predominance of staphylococcus and streptococci: colitis, irritable bowel, gastritis, duodenitis, ulcers, coagulopathy, arterial pathologies, arthritis, malignant neoplasms, caries, bronchial asthma, encephalopathy, opportunistic infections, gout, diabetes mellitus, infertility, premature birth, anemia, cachexia.
Treatment staphylococcus aureus in the smear.
Various folk remedies are widely used to treat dysbacteriosis and eliminate staphylococcal infections.
A mixture that increases immunity and body resistance has proven itself well. Due to propolis and aloe juice, the microflora is normalized. Take 100 grams of dried apricots, prunes, dates, and mince. Separately squeeze the juice of 3-4 large aloe leaves. Melt the propolis over low heat while stirring constantly, remove from heat, add the squeezed aloe juice. Mix thoroughly until a homogeneous mass is formed. Then mix with the mass passed through the meat grinder, mix thoroughly, let it brew for 10-12 hours. You can take up to 3-4 tablespoons a day.
Another vitamin mixture is also used, which quickly restores the microbiocenosis, normalizes the immune system. Take 100 grams of viburnum, sea buckthorn, lingonberry. Mash with a spoon until a homogeneous gruel is formed. Separately, melt 50 grams of honey, add a third of a teaspoon of ground cinnamon, ginger and nutmeg. Stir until a homogeneous mass is formed, slowly pour into the previously prepared berry mass.
To improve overall well-being, increase performance, eliminate symptoms of bacterial infection and intoxication, use juice of the following composition: freshly squeezed juice of 1 lemon, juice of 1 pomegranate, 50 ml of rosehip syrup. Mix all this, leave for an hour, drink 1-2 glasses per day.
Herbal treatment
Many herbs have antiseptic properties, the main thing is to know how to use them correctly.
Lingonberry is used to treat many diseases, including bacterial infections and dysbacteriosis. It has antiseptic properties due to the high content of flavonoids, tannins, and organic acids. Ripe berries and leaves are mainly used. They contain atrubin, hydroquinone, and carotene, which gives the plant diuretic, astringent, and anti-inflammatory properties. The berries are collected in October, and the leaves in May and June. It is used as a decoction, infusion, in various mixtures, and as an additive to tea. An aqueous infusion of berries is used as the main drink for patients with fever.
Oregano also has an antiseptic effect, relieves inflammation, normalizes the condition and microflora of the female reproductive system. It is used primarily to treat gynecological diseases caused by microflora disorders.
Used in the form of decoctions and infusions, for external use. Used for washing, douching, lotions, compresses. Effective for medicinal baths, has anti-inflammatory, soothing, relaxing effect. Normalizes emotional state.
Marsh wild rosemary is a good bactericidal plant, which is used mainly in the therapy of respiratory tract of viral and bacterial etiology, as well as for the treatment of infectious diseases, cough. It can relieve the condition even of eczema, neoplasms. The main components are dried around May. Stems, leaves and flowers are used. Bactericidal properties are provided by glycosides, tannins. Also, the plants contain a large amount of palustrol, ledol, and other substances, which provides its main properties.
Red clover is used in the treatment of purulent, inflammatory, septic processes of bacterial origin. It is effective against anemia, colds, diphtheria. It helps to eliminate pain (due to antiseptic, anti-inflammatory methods). For rapid healing of wound surfaces, a powder of crushed leaves is also used. It blooms in June, at the same time the medicinal raw materials are collected. It is used mainly in the form of decoctions, less often - in the form of infusion.
Homeopathy
In the treatment of bacterial diseases, infections, and dysbacteriosis, probiotics play an important role. They are products based on bacterial cultures that are included in the microflora and normalize its condition. They provide reliable prevention and treatment of microecological disorders, eliminate various types of autoinfection, including staphylococcal.
It is important to take precautions: never take the medications yourself, they should be prescribed only by a doctor. Even a doctor prescribes medications only after receiving the results of a bacteriological study and an analysis for dysbacteriosis, which will show the state of the microbiocenosis. This will allow you to choose the right drug. Incorrect use of the drug can provoke numerous side effects, such as further disruption of the microflora and the development of autoinfection, generalization of the infection, the spread of purulent-septic phenomena.
A-bacterin consists of a lyophilized culture of aerococci, which are antagonists of staphylococcal infection. One dose of the preparation contains 2×108 viable aerococci. It is available in vials.
Used internally or externally. For internal use, it is used to combat dysbacteriosis and intestinal infections, especially those that developed after antibiotic therapy, as a result of past infections.
When applied externally, it is used to treat purulent wound infections of staphylococcal etiology caused by other forms of microorganisms.
Apibact consists of live biomass of probiotic bacteria cells of fairly high concentration. Contains bifidobacteria, lactic acid, propionic acid bacteria, and lactobacilli. Available in bottles or sachets. Used for the prevention and treatment of dysbiosis and associated diseases in children over 2 years of age and adults.
Acidophilus consists of acidophilic lactobacilli. It is produced in the form of capsules. One capsule contains 2.5 billion lyophilized cells. It is used for dysbacteriosis of various origins, fungal infections of the intestines, vagina, and skin. It is also prescribed for acute colitis, constipation, diarrhea, lactose intolerance, hypovitaminosis, high cholesterol, and decreased immunity.
Baktisubtil consists of bacillary forms of microorganisms, and also includes additional components. It is used for diarrhea, dysbacteriosis, enteritis, enterocolitis. It is often prescribed to eliminate the negative consequences caused by chemo- and radiotherapy. It has a therapeutic effect on pyelonephritis caused by enterobacteria, proteus, other opportunistic forms, staphylococcus. It is effective for the treatment of infected varicose wounds.
Surgical treatment
Surgical methods are rarely used for treatment. Surgical methods are not suitable for eliminating the direct cause of the disease – staphylococcal infection, since they do not directly affect the infection. Only antibiotic therapy is effective in this regard. But surgical methods can be used to eliminate the consequences of infection, such as severe inflammation, abscesses, purulent exudates that formed as a result of exposure to bacteria and their toxins.
Surgical methods can be used to treat peritonitis, acute appendicitis, neoplasms, purulent accumulations, and areas of necrosis.
Prevention
The essence of prevention is to avoid conditions under which staphylococcus will multiply intensively. It is also necessary to maintain a normal level of immunity and avoid stress. It is important to have a balanced diet, to have all the necessary components in food, and to have a sufficient amount of vitamins and minerals. You must not overcool, be nervous, or overwork yourself.
Forecast
If staphylococcus is detected in a smear in a timely manner and all necessary measures are taken to normalize its quantitative indicators, as well as to normalize all accompanying microflora, the prognosis is quite favorable. It is possible to achieve a balance in the microbiocenosis, and it itself will act as a homeostasis regulator, will provide protection for the body, and maintain colonization resistance. If the infection is not treated and the microbiocenosis is not normalized, the prognosis can be extremely unfavorable. One should expect the development of infectious and inflammatory diseases, sepsis, which can progress to a fatal outcome.


 [
[