Medical expert of the article
New publications
Signs of esophageal hernia
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Diseases of the digestive system have become so widespread in our time that they are usually discussed as often as colds or allergies. In this case, mainly diseases of the stomach and intestines are taken into account, and we forget about such an important organ as the esophagus - a muscular tube through which food passes from the oral cavity to the stomach. It would seem that nothing threatens it, except perhaps too spicy or sour food that passes by. However, for some reasons, even in the area of this organ, a hernia can form, which, if left untreated, can develop into cancer or cause inflammatory processes in the stomach. It is difficult to insure against this pathology, so it is useful for everyone to know the symptoms of an esophageal hernia in order to seek help from doctors in time, who will help stop the development of the disease and its complications.
What is a hiatal hernia?
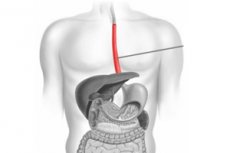
Before we begin to consider the symptoms of the disease, let us briefly mention what a hiatal hernia is and what causes it. Our body is a strictly structured system, where each organ has its own place, and any changes in location are considered a pathology (congenital or acquired). The abdominal and thoracic cavities have a common border, along which a muscular plate called the diaphragm runs.
The stomach and almost all other digestive organs, with the exception of the upper part of the esophagus, are located under the diaphragm. And in order for food to enter the lumen of the stomach through the esophageal tube, a small-diameter opening is provided in the muscular plate.
The lower part of the esophagus, like the stomach or intestines, is located under the muscular plate and normally never protrudes into the chest area. If the lower part of the esophagus, some parts of the stomach or even the intestines are found in the chest area above the diaphragm, they speak of a hernia. The diagnosis may sound like "esophageal hernia" or "hernia of the esophageal opening of the diaphragm."
The causes of this pathology may be rooted in both developmental defects of the child during the intrauterine period (shortened esophagus or so-called "chest" stomach), and in age-related changes in the tone of the ligamentous apparatus, which should not allow the displacement of organs (the disease most often affects people over 50-60 years old). But the displacement of organs, even with a healthy ligamentous apparatus, can cause increased intra-abdominal pressure. Increased pressure in the abdominal cavity can be caused by pregnancy, chronic flatulence or severe bloating due to intense gas release in the intestines, injuries and extensive tumor processes.
Displacement of the gastrointestinal tract organs relative to the diaphragm can also be caused by some pathologies accompanied by uncontrollable vomiting or severe, painful coughing (for example, food poisoning or obstructive bronchitis). Chronic inflammatory and ulcerative diseases of the gastrointestinal tract are often characterized by decreased peristalsis of individual structures of the digestive system, and dyskinesia is considered a risk factor for the formation of a hernia, i.e. displacement of organs relative to their normal position.
The incorrect arrangement of organs, as a result of which the process of digestion of food is disrupted, and the contents of the stomach can enter the esophagus, causes the symptoms of esophageal hernia characteristic of the pathology. If the size of the hernia is small, then it may not cause much discomfort to a person. In this case, we are talking about an asymptomatic course of the disease. But as the hernia increases, unpleasant sensations appear, which we will discuss in more detail in the next section.
How does a hiatal hernia manifest itself?
The distal part of the esophagus, the cardiac parts of the stomach, and sometimes even intestinal loops can protrude beyond the abdominal cavity through the gap in the diaphragm. It is clear that in these cases, not only the appearance and size of the hernia will differ, but also its symptoms. With a slight protrusion of the lower part of the esophagus, there may be no symptoms at all, because such a pathology does not affect the digestion process in any way.
But if the stomach or intestines begin to protrude into the chest cavity through the hole in the diaphragm, symptoms will not be long in appearing. After all, gastric juice, bile and other digestive enzymes in this case can be thrown back into the esophagus, as in reflux disease. But this organ is not designed for contact with such irritants, because it has no special protection. Regular throwing of caustic substances worsens the condition of its walls, causing pain and other unpleasant symptoms.
First, the gastric sphincter suffers, which stops performing its functions and passes the contents of the stomach back into the esophagus, and then irritation of the walls of the esophagus by gastric enzymes causes their inflammation. Gradually, the inflammatory process can spread to other organs of the digestive system.
Pain and its nature. Since there is irritation of the walls of the esophagus, and later the stomach, a person begins to experience pain. How does an esophageal hernia hurt? The pain syndrome depends on the type and size of the hernia. If the hernia is small (esophageal or cardiac, when only the lower part of the esophagus or a small part of the upper, cardiac part of the stomach protrudes into the sternum), there may be no pain at all, as well as other symptoms of the pathology. In this case, the disease is detected accidentally during fibrogastroscopy or ultrasound, after which the behavior of the hernia is monitored.
If the hernia is significant in size, but the gastric sphincter still functions normally and does not allow food to flow back into the esophagus, the patient will suffer from aching pains, which may become stronger after eating. Relief comes from taking a deep breath or passing air from the gastrointestinal tract (belching).
If the locking mechanisms at the boundary of the esophagus and stomach are damaged, and reflux is observed (cardia insufficiency syndrome is diagnosed), the pains become sharp and burning. They are directly dependent on food intake and the patient's body position. The pain becomes stronger in a lying position (horizontal) or when bending forward. An identical situation is observed after eating when the contents of the stomach are thrown into the esophagus.
The localization of pain is somewhat blurred. It can be the epigastric region and chest. Pain behind the sternum can resemble heart pain, and it can be relieved by the same nitroglycerin. Intercostal pain and pain syndrome in the abdominal cavity can suggest pathologies of the stomach and liver. Sometimes the pain radiates to the back between the shoulder blades, which makes diagnosis even more difficult.
When partially digested food with gastric enzymes is thrown into the esophagus, it can rise higher to the throat. In this case, patients begin to complain of a burning sensation and pain in the throat, caused by the irritating effect of gastric juice. Some even develop a slight cough, while the temperature against the background of the inflammatory process in the upper gastrointestinal tract with an esophageal hernia can rise to 37-37.5 degrees, which suggests a cold.
Dysphagia and a lump in the throat. The irritating effect of acid in the gastric juice and pain caused by the compression of the hernia can lead to difficulty in eating. With an esophageal hernia, patients note such a symptom as a lump in the throat, or rather a feeling of some obstacle in the path of food. In fact, we are talking about a nervous reaction that causes a spasm of the esophagus. It is the sensation of a lump along the esophageal tube that leads to the appearance of pain between the shoulder blades and in the heart area, radiating to the shoulder, as in angina.
Almost half of patients with a large axial hernia experience a condition called dysphagia, i.e. difficulty swallowing. An important point is the fact that it is easier for patients to swallow solid food than liquid or semi-liquid food. Dysphagia can occur due to nervous experiences, eating food that is too cold or too hot, or rushing while eating. An increase or strangulation of the esophageal hernia leads to spasms appearing not situationally, but on a permanent basis, which leads to an unpleasant feeling of a lump in the throat even outside of meals or when eating solid foods that have to be “pushed” with liquid.
Dyspepsia. One of the most popular symptoms of esophageal hernia is considered to be heartburn. The frequency of this symptom with axial hernia, which is considered the most common and is characterized by protrusion of the esophagus and cardiac part of the stomach, is even greater than that of pain. The appearance of this symptom is most often associated with food intake, although with physical activity and a sharp change in body position it can remind of itself on an empty stomach.
At night, heartburn with a hernia of the esophagus occurs even more often than during the day or in the morning. This is associated with an increase in the tone of the vagus nerve during this period, which goes from the brain to the abdominal cavity, and the general relaxation of the body and in particular the sphincter on the border of the stomach and esophagus, which is called the lower esophageal sphincter.
The intensity of the symptom may vary. In most cases, it is a mild form, which can be successfully treated with antacids. But sometimes heartburn can be so severe that it deprives a person of sleep and rest, and a strong, painful burning sensation in the chest interferes with work, negatively affects well-being, mood, and appetite.
The severity of heartburn is determined not so much by the size of the hernia as by the characteristics of the gastric juice (high, normal or low acidity of the stomach), the entry of bile from the duodenal region into the esophagus, the force of stretching of the esophagus during reflux (the amount of food thrown back, associated with the work of the lower esophageal sphincter).
During heartburn, a person may feel a sour or bitter taste in the mouth, characteristic of the contents of the stomach and duodenum. He may experience nausea and bloating. The latter symptom is not directly related to heartburn, although it often occurs in combination with it. Flatulence is often complained of by those patients who do not have severe pain, but only minor discomfort and a feeling of constriction in the epigastrium.
Another problem with a hernia of the esophagus is belching, and this can be either belching air or regurgitating food, even vomiting. The feeling of bloating does not appear in patients by chance. It is associated with increased intra-abdominal pressure due to compression of the stomach in the opening of the diaphragm, while sometimes spasmodic contractions of the esophagus can occur and lead to belching, i.e. involuntary release of air, and sometimes food. Belching can occur both during and after eating, accompanied by a specific sound, which is another cause of psychological discomfort in patients, especially since the use of antispasmodics in this case does not give the desired result.
It should be said that belching itself, despite the unaesthetic nature of its manifestations, in some sense benefits patients, easing their condition. After belching, pain and heartburn usually decrease. Therefore, it is not surprising that patients often provoke belching on their own, swallowing a large amount of air and trying to push it out of the esophagus by force.
Belching of food is most often observed immediately after eating or when taking a horizontal position, and sometimes with sharp bends. The amount of regurgitated food may vary, depending on the performance of the esophageal sphincter. With a greatly reduced tone, it can even lead to a single vomiting. In this case, such a symptom as nausea does not accompany belching, regardless of its strength.
A small percentage of patients also complain of hiccups, which torment them for several weeks or even months. Usually, the symptom is associated with food intake and is determined by spasmodic contractions of the diaphragm, for which the hernial sac is an irritant. The treatment does not affect the severity and frequency of hiccups.
Clinical picture of esophageal hernia depending on the degree and nature of the pathology
A hernia of the esophageal orifice of the diaphragm is a generalized concept, because the pathology can have various forms of progression and stages of development, depending on which the clinical picture of the disease changes. Thus, it is customary to distinguish between a floating and a fixed hernia of the esophagus. The latter is considered a rarer, but at the same time more dangerous pathology, which is characterized by frequent complications in the form of strangulation of the hernia, perforations of the esophageal tube and bleeding from the gastrointestinal tract, heart problems, and an increased risk of esophageal oncology.
A floating esophageal hernia (also called sliding or axial) is a protrusion of the distal part of the esophagus and some part of the stomach into the chest cavity. Sometimes almost the entire stomach can fall out into the opening, which indicates a large hernia that compresses the organs of the chest (lungs, heart), causing disruption of their functioning and corresponding symptoms in the form of coughing and heart pain.
The stretching of the diaphragmatic opening, into which the esophagus enters, is controlled by the esophageal-diaphragmatic ligament. With a decrease in its tone and degenerative processes, manifested in the form of thinning of dense connective tissue, the opening in the diaphragm can increase. With increased intra-abdominal pressure, pregnancy, obesity, age-related changes, congenital defects of the diaphragmatic opening, the cardiac part of the stomach can shift upward relative to the opening of the diaphragm, thereby forming a hernia.
A floating hernia of the esophagus is said to occur when, with a change in body position and physical exertion, the stomach together with the esophagus can shift in the opening of the diaphragm. Thus, they sometimes protrude into the thoracic region, then return to their place in the abdominal cavity. With a small hernia and normal functioning of the sphincter, the sliding variant of the pathology is asymptomatic. But with a violation of the tone of the lower esophageal sphincter, a reflux of the stomach contents into the esophagus (gastroesophageal reflux) is observed, which is accompanied by belching, heartburn, pain syndrome, a burning sensation behind the sternum. A clear connection is seen between the unpleasant symptoms that appear with food intake (especially abundant) and a change in body position, on which the displacement of the esophagus and the cardia of the stomach depends. Incarceration of an esophageal hernia of this nature is not observed.
With a fixed hernia, which is often called paraesophageal, the middle and lower parts of the stomach and even the duodenum can protrude into the chest cavity, while the position of the esophagus remains fixed. That is, the hernia is formed not along the esophagus, but next to it, and it is not prone to changing its size and position. However, when the position of the body changes, the hernia can be compressed (incarcerated), which is fraught with overstretching of the walls of the prolapsed part of the stomach and their rupture. In this case, fluid accumulates in the pleural cavity, severe acute pain and signs of blood poisoning appear.
The most characteristic symptoms of this type of pathology are a pressing pain in the pit of the stomach and a feeling of heaviness that appears after a heavy meal, which forces patients to limit the amount of food, belching, regurgitation of food and vomiting. Disruption of food movement from the stomach to the intestine provokes the development of a peptic ulcer, which is complicated by perforation of the stomach tissue and active hemorrhages. With a sliding hernia, hemorrhages occur in the esophagus, but they are insignificant and do not appear externally.
Reflux is not observed with a fixed hernia, heartburn is rare. However, in the case of a combined hernia, the appearance of such symptoms is not excluded.
The symptoms of a hiatal hernia may vary depending on the stage of the disease, because this pathology is considered progressive, especially if it is caused by age-related changes that negatively affect the tone of the ligaments of the diaphragmatic opening and the lower esophageal sphincter. Each of the 3 stages of the disease has its own symptoms, but it is difficult to determine an accurate diagnosis based on them alone without an instrumental examination.
Esophageal hernia of the 1st degree is the initial period of the disease, when the lower part of the esophageal tube penetrates the opening, and the stomach remains on the other side of the diaphragmatic plate, tightly adjoining it and forming a kind of dome. Usually, at this stage of the disease, patients rarely complain of any symptoms of malaise. Minor discomfort and mild pain in the epigastrium may be mentioned.
The initial stage of hernia development is detected accidentally during instrumental diagnostics of other diseases. It is impossible to detect it by palpation. However, treatment of this pathology usually comes down to following a special diet and monitoring the behavior of the digestive organs.
A grade 2 esophageal hernia is characterized by penetration into the thoracic region of not only the distal esophagus, but also the lower esophageal sphincter and a small part of the stomach. Symptoms of the pathology begin to manifest themselves more clearly. Patients complain of pain behind the breastbone or in the epigastrium, discomfort (a feeling of compression or distension), the appearance of belching and burning in the chest area. A little later, a sensation of a food lump, difficulty swallowing, heartburn (with a sliding hernia) appear.
Treatment of the second stage of the disease, in addition to diet, involves drug treatment: taking antispasmodics, enzyme preparations, antacids and drugs that reduce the production of hydrochloric acid.
A third-degree esophageal hernia is not only an unpleasant but also a dangerous pathology that is fraught with various complications. In this case, a significant part of the stomach and sometimes intestinal loops are displaced into the sternum, which leads to a disruption of the digestive process. In addition to the symptoms described above, patients complain of severe heaviness in the stomach after eating, a lump in the throat, severe pain in the chest, frequent belching of air, and sometimes regurgitation of food. Patients with a combined hernia of the esophageal opening of the diaphragm mainly complain of heartburn attacks.
Diet and conservative treatment in this case are relevant only after surgical intervention (laparoscopic surgery to return the digestive organs to the abdominal cavity and suture the diaphragmatic opening, antireflux surgery - fundoplication).
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
Esophageal hernia in children and pregnant women
Many consider a hernia of the esophageal opening of the diaphragm to be an age-related disease due to the fact that this pathology is diagnosed in most cases in people over 50 years of age. Yes, a decrease in the tone of the esophageal opening can be facilitated by a metabolic disorder in muscle and connective tissues caused by diseases accumulated over many years of life, and a chronic course of ulcerative-inflammatory pathologies of the gastrointestinal tract. But according to statistics, there is a certain percentage of morbidity caused by congenital anomalies or temporary conditions leading to an increase in intra-abdominal pressure, which is already higher than the chest.
A hernia of the esophagus in a child, as in an adult, is a pathology characterized by the displacement of a section of the digestive tract from the abdominal cavity to the chest. But unlike adults, we are talking about a congenital pathology, and not an acquired disease, so the symptoms of a hernia of the esophagus in children can be observed already in the first days of their life.
The pathology is usually diagnosed at an early age, it is not typical for teenagers (congenital pathology reminds of itself much earlier, and for acquired it is still too early). Esophageal hernia in an infant can occur due to insufficient length of the esophageal tube or congenital weakness of the diaphragmatic opening, the causes of which are hidden in the intrauterine period of the child's development.
At a later age, a hernia of the esophagus may be caused by trauma that has led to increased intra-abdominal pressure, frequent heart-rending crying, illnesses accompanied by a prolonged painful cough, overfeeding and obesity, a tendency to constipation, excessive physical activity (for example, lifting heavy objects).
The clinical picture of esophageal hernia in small children includes persistent vomiting and regurgitation after eating. In case of congenital pathology, these symptoms remind of themselves already during the first month, and often even in the first week of the baby's life. It is not possible to relieve the symptoms with medications, which gives reason to suspect an organic nature of digestive disorders, not related to the nature and amount of food.
In some cases, doctors diagnose hemorrhagic syndrome. Its symptoms are bloody vomiting and the presence of blood in the child's stool. Blood loss leads to tissue cyanosis and the development of anemia, which are considered one of the signs of pathology in an infant who cannot yet tell about pain in the abdomen or chest.
Doctors associate the chest pain that older children complain about and tissue cyanosis with developing reflux esophagitis (irritation and damage to the esophageal mucosa due to the reflux of acidic contents from the stomach), as well as with a partial strangulation of the hernia.
Unpleasant sensations after eating in a child can cause a decrease in appetite or refusal to eat, which only worsens the course of anemia. Vomiting can be accompanied by swallowing disorders and the development of aspiration pneumonia, i.e. inflammation of the lungs caused by food particles entering the respiratory tract. With a large hernia, even the symmetry of the chest can be disrupted due to the appearance of an unusual protrusion.
Nutritional and respiratory disorders due to aspiration pneumonia lead to the child starting to lag behind his peers in development. After eating, such children may experience shortness of breath, and their pulse may quicken, which indicates compression and disruption of the cardiovascular and respiratory systems.
The severity of symptoms in children may vary, so the disease is not always diagnosed at an early stage. The fact is that reflux and regurgitation in the first months of life are considered normal, which means that in the absence of vomiting and frequent burping, parents and doctors may not attach due importance to these symptoms, especially since esophageal hernia is very rarely diagnosed in childhood. Anxiety appears when the child himself already states that his throat is burning and his chest hurts. In the best case, the disease will be discovered by chance and it will be possible to stop its progression in time.
Esophageal hernia during pregnancy is not such a rare phenomenon, however, in many cases it occurs without pronounced symptoms, so it can be noticed after childbirth. Pregnancy itself becomes a risk factor for the development of hernia due to a decrease in the tone of the diaphragmatic plate and the lower esophageal sphincter (hormonal changes leave an imprint on the metabolism and characteristics of tissues), an increase in intra-abdominal pressure as the baby develops and the uterus increases in size, toxicosis of pregnancy, which is accompanied by vomiting and the development of reflex esophageal spasm.
True, not all pregnant and postpartum women develop esophageal hernia. The risk group includes women over 30 who have had more than one pregnancy and birth.
The symptoms of esophageal hernia in pregnant women are no different from those in other groups of the adult population. They may also suffer from heartburn and belching, pain behind the breastbone and in the upper abdomen, difficulty swallowing, and regurgitation of food. Some also note increased salivation due to irritation of the food receptors in the mouth by the acidic contents of the stomach getting there. With esophageal hernia and frequent vomiting caused by early toxicosis, women note that their voice becomes hoarse and the mucous membrane of the tongue becomes painful.
Toxicosis and vomiting in early pregnancy are nothing new, and this symptom usually has nothing to do with esophageal hernia. However, frequent vomiting in the last trimester of pregnancy may be one of the obvious symptoms of hernia. Anemia after 4 months may also indicate the development of pathology.
An axial hernia of the esophagus, characterized by a benign course and not prone to strangulation, is treated during pregnancy with conservative methods and is not an obstacle to independent childbirth. But a fixed hernia poses a danger to the life of the mother and fetus, requires special monitoring of the course of the disease and involves a cesarean section. After all, during childbirth, with high pressure inside the peritoneum, its strangulation may occur, accompanied by acute pain up to loss of consciousness.
Diagnosis of hiatal hernia
As we have already managed to understand, the symptoms of a hernia of the esophagus are not particularly specific. Those who have such diseases as gastritis, pancreatitis, stomach ulcers and some others can say that all the above symptoms are well known to them. Moreover, many patients with a hernia and who have not sought advice from a gastroenterologist, who first prescribes diagnostic tests and then makes a final diagnosis based on their results, independently treat a non-existent pathology, having diagnosed themselves with the same gastritis or stomach ulcer, and sometimes even heart and lung diseases.
Diagnosing a hiatal hernia based on external manifestations alone is a thankless task, since the symptoms of this pathology are typical for most diseases of the gastrointestinal tract. Questioning the patient and prescribing standard blood and urine tests can only nudge the doctor in the right direction.
The doctor pays attention to any of the symptoms listed below, but if they are present in combination, this clearly indicates an existing pathology of the digestive system:
- Dull, aching or sharp pain in the upper abdomen and chest, changing in intensity with changes in body position and depending on food intake.
- The appearance of painful heartburn, which is present for a long time, a burning sensation behind the breastbone.
- Regularly repeated belching of air and food, burping after a heavy meal or bending forward.
- Frequent episodes of hiccups lasting several minutes.
- The appearance of pain and burning in the throat and tongue, changes in the timbre of the voice, cough, not associated with colds and heart pathologies.
Any of the listed symptoms may indicate ill health, but it is impossible to say what disease exactly is being discussed, and even if the entire symptom complex is present, it is impossible to say with certainty that we are dealing with an esophageal hernia. And since the reason for the change in the patient's well-being is hidden inside the body, doctors focus on instrumental diagnostics, which allows them to examine internal structures hidden from the eye.
Gastroscopy is considered a standard diagnostic test for esophageal hernia and many other gastrointestinal pathologies. Fibrogastroduodenoscopy (abbreviated FGDS) is a study of the esophagus, stomach and part of the duodenum from the inside, by inserting a flexible tube with a mini-camera at the end through the patient's mouth. In other words, this is a low-traumatic endoscopic study that allows you to see the condition of the internal surfaces of the digestive organs without making incisions and identify inflammatory and erosive-ulcerative processes in them.
FGDS allows you to visually assess the condition of the mucous membrane, changes in the shape of the stomach and esophagus, their size, and contractile function. What signs during FGDS help to suspect an esophageal hernia:
- Insufficient length of the esophagus, which in adults ranges from 23 to 30 cm, a decrease in the size of its abdominal section and the distance from the lower incisors to the cardia of the stomach.
- The presence of foci of stenosis of the esophagus and stomach and hernial cavity.
- Poor functioning of the lower esophageal sphincter, which does not close completely or contracts inactively.
- Reflux of stomach contents into the lumen of the esophagus and associated unevenness of the surface of the mucous membrane of the lower part of the esophagus.
- Changes in the size and severity of the angle between the esophagus and the wall of the stomach (the angle of His increases and smooths out).
- Mild expression of the folds of the stomach at the point where it joins the esophagus.
- Increased acidity of gastric juice, which doctors can also measure during FGDS.
- The appearance in the epithelial lining of the esophagus of an uncharacteristic cylindrical epithelium, which is present in the intestinal mucosa (Barrett's esophagus or Barrett's metaplasia is a precancerous condition caused by gastroesophageal reflux, which occurs chronically with an esophageal hernia).
All of the above may indicate a hernia of the diaphragmatic opening of the esophagus only indirectly, but they are a reason for prescribing a more detailed examination. Changes in the location of the digestive organs relative to the diaphragmatic plate can be seen and assessed using radiography.
X-rays are mandatory for patients with suspected esophageal hernia, because this study allows for a high-precision diagnosis of this pathology and differentiation from stenosis, gastric ulcer, short esophagus, reflux disease, etc.
Doctors usually prefer conventional radiography, but since the soft tissues that make up the digestive organs are less visible on an X-ray than hard tissues, the examination is performed with a contrast agent (barium sulfate is usually used as a contrast agent).
An axial hernia is detected with high accuracy during fluoroscopy, since the image clearly shows the upward shift of the esophagus and stomach, with the lower part of the esophagus, the cardia of the stomach, and sometimes the entire stomach being above the diaphragm. Even with a general chest X-ray, a light spot in the shadow of the heart can be seen in the area of the posterior mediastinum. After the introduction of contrast, fluoroscopy in the supine position with increased intra-abdominal pressure in case of an esophageal hernia will show the reflux of the barium compound into the esophagus from the stomach cavity, thickening of the stomach vault, a change in the angle of His, and a shift of the esophagus at the moment of inhalation by more than three centimeters.
In the case of a less common fixed esophageal hernia, conventional radiography is of little information. In this case, a tomogram (computer or magnetic resonance) may be prescribed to clarify the diagnosis. CT of an esophageal hernia allows for the reconstruction of a three-dimensional image of the gastrointestinal tract using the same X-rays and contrast, so it is prescribed when the diagnosis is controversial or there are questions that cannot be resolved using conventional X-rays.
Most often, a hernia is diagnosed accidentally during a CT scan of the chest or abdominal region. This reveals protrusions of the gastrointestinal tract into the chest, an enlarged diaphragm opening, the presence of an omentum in the area of the hernial sac with a fixed hernia, an "inverted stomach" protruding into the chest (visible in a three-dimensional image).
MRI of esophageal hernia is also not a popular diagnostic test. Sometimes there is simply no point in conducting expensive diagnostics if the problem is detected during budget tests such as esophageal X-ray. However, it should be said that magnetic resonance imaging visualizes soft tissues better than X-rays and CT, and the test itself is considered safer.
Ultrasound of the esophagus and stomach in case of a hernia of the esophageal opening of the diaphragm is not a sufficient examination, although it allows one to suspect this disease in the patient. A final diagnosis can only be made after an X-ray, CT or MRI of the stomach and esophagus.
In case of fixed esophageal hernias, a study such as pH-metry is also necessary, which allows to evaluate the frequency and features of the reflux of stomach contents into the esophagus, to determine the acidity of gastric juice and the reasons for its increase. The study is conducted during the day using a probe inserted through the nose and a portable recorder attached with a belt on the waist. During the study, the patient can move freely, eat food that does not affect the acidity of the stomach, rest, etc.
Such a study in time allows to evaluate the work of the stomach and lower esophageal sphincter, and not only to record static sizes and location, as in X-ray. If increased acidity of gastric juice caused by gastritis or stomach ulcer is detected, then these concomitant pathologies are also treated.
Since the symptoms of a hiatal hernia include difficulty swallowing, patients may be prescribed a test called esophagomanometry, which allows one to evaluate the strength of contraction of the esophageal muscles during swallowing. This test is indicative of disorders of the upper gastrointestinal tract, since it allows one to evaluate the contractility and condition of the tissues of various sections of the esophagus and stomach. Manometry helps to diagnose the failure of the lower esophageal sphincter, which allows food to move in the opposite direction (reflux).
Treatment of esophageal hernia
If you pay attention to the pathology when its first symptoms appear and undergo the required examination, the treatment of the disease is much simpler and gives good results even without surgery. A very important role in this is played by the diet, which helps maintain a normal level of acidity of gastric juice, which reduces irritation of the esophagus walls during reflux, and also adjusts the volume of food consumed, which makes it possible to reduce the frequency of belching.
Since the bulk of unpleasant symptoms (chest and epigastric pain, heartburn, burning along the esophagus and in the throat, an increase in temperature to subfebrile values) is associated with reflux esophagitis (throwing up of gastric contents into the esophagus and associated inflammatory and destructive processes), the treatment of esophageal hernia is generally similar to the therapy of this pathology. The goal of such treatment is to reduce the irritating effect of stomach contents on the esophagus by neutralizing its aggressive components, facilitating the movement of the food bolus along the esophagus, increasing the tone of the stomach and lower esophageal sphincter.
Treatment is carried out in a comprehensive manner through:
- drugs that increase gastrointestinal motility (prokinetics) and help combat symptoms such as reflux, hiccups, regurgitation of food, vomiting,
- medicines that reduce stomach acidity (antacids),
- drugs that reduce the production of hydrochloric acid (proton pump inhibitors),
- histamine receptor blockers used in gastroenterology (they act similarly to the previous drugs and are prescribed when it is impossible to take them).
Sometimes, to prevent congestion and relieve heaviness in the stomach, it is recommended to take enzyme preparations: Mezim, Festal, Creon, Pancreatin and even Holenzym, which stimulates the production of bile and its transportation to the duodenum, and thereby speeds up the process of digestion.
But if other enzyme preparations are often prescribed for various stomach pathologies to facilitate its work, since they do not have an aggressive effect on the mucous membrane, then "Cholenzym" is mostly used for liver, gall bladder and pancreas pathologies and provokes the release of bile, which will be of dubious benefit in case of esophageal hernia. Especially if we are talking about reflux, when half-digested food can be thrown into the esophagus from the stomach and initial sections of the intestine, where it will be generously flavored with bile.
It is better to choose regular enzyme preparations to help the stomach, which are safer for stomach and esophageal pathologies. In case of constipation, which often accompanies various gastrointestinal pathologies, it is worth paying attention to the drinking regime, and if necessary, take laxatives, because straining with a hernia of the esophageal opening of the diaphragm contributes to an increase in intra-abdominal pressure, which should not be allowed.
Readers have probably noticed that there is no indication of analgesics among the medications prescribed for reflux and esophageal hernia. But pain in the chest and epigastrium is one of the main symptoms of the pathology. The similarity of these pains with heart pains is the reason why patients try to relieve them with nitroglycerin. This method works, but its side effect is that such treatment strengthens the patient's belief in the existing cardiovascular disease and distracts from the true cause of the deterioration in health.
How to relieve pain from a hiatal hernia? Pain from reflux and hiatal hernia is associated with stagnation of food in the gastrointestinal tract and its reflux into the esophagus. The irritating effect of digestive enzymes causes irritation and inflammation of the organ walls, which is accompanied by pain. It turns out that pain can be relieved with drugs that reduce the acidity of gastric juice and form a protective film on the walls of the stomach and esophagus. We are talking about drugs in the form of a suspension (Almagel, Phosphalugel, Maalox), which begin to act already during passage through the esophagus, while tablet forms of drugs require dissolution in the stomach. Drugs that are prescribed to combat increased acidity of gastric juice will also act as painkillers.
Many folk remedies also help to combat the unpleasant symptoms of esophageal hernia. Thus, natural flower honey, which is used in the treatment of many diseases, including gastrointestinal diseases, is very beneficial for esophageal hernia.
Honey is not a cure for reflux esophagitis, and during an exacerbation of the disease it can only increase irritation of the esophagus if consumed in its pure form. But in the chronic course of the inflammatory process in the esophagus, observed with a hernia, this natural medicine will have an antibacterial and anti-inflammatory effect. However, it is better to use it as part of multi-component recipes or diluted in water (up to 50 ml per day), giving preference to easily digestible linden honey.
For example, to combat heartburn, you can prepare a simple and tasty medicine from equal parts of honey and walnuts, which must be peeled and crushed in advance. The composition should be consumed after meals, 1 tbsp.
To treat heartburn, honey can be mixed with other ingredients:
- aloe juice (proportions 1:1, take 1 teaspoon before and after meals),
- warm milk (1 tbsp. honey per 1 glass of milk, drink an hour before the main meal, and also when painful attacks occur),
- potato juice (1 teaspoon of honey per ½ cup of juice, take one hour before meals).
In one recipe, you can combine the detoxifying and tonic properties of apple cider vinegar and the antibacterial, restorative and anti-inflammatory effects of honey. Mix 1 tbsp of natural apple cider vinegar with the same amount of honey and dilute in a glass of water. Take this unusual medicine regularly before meals, which helps prevent heartburn, pain and other symptoms of esophageal hernia.
To combat belching, a composition based on honey, cranberries and aloe juice, taken in equal quantities, is suitable. The berries and peeled aloe leaves should be minced or chopped in a blender, mixed with honey and poured with boiled water. The remedy is infused for at least 6 hours, after which it should be drunk little by little throughout the day.
Flax is also considered useful for esophageal hernia. Flax decoction (1 tbsp. per 0.5 l of water, boil for 3-5 minutes and leave for at least 2 hours) will create a protective film on the walls of the stomach and esophagus, thereby reducing the likelihood of irritation of the mucous membranes by digestive enzymes. This same remedy is considered an effective antacid, since it can reduce the acidity of gastric juice.
Another recipe for esophageal hernia based on flax seeds. For 1 tbsp. flax seeds take 3 tbsp. cool water, leave to infuse overnight. In the morning heat to boiling, but do not boil. Use the entire mixture completely, chewing the grains thoroughly.
Tea for esophageal hernia is a dubious medicine. But it depends on what kind of tea. If we are talking about strong hot black tea, then it is better to refuse such a tonic drink, because it will only stimulate the production of digestive enzymes and increase the acidity of the stomach, especially in those who already suffer from this disorder. But nutritionists even include warm green tea in the menu for esophageal hernia.
But herbal teas are especially useful for this pathology. The first on the list of useful drinks for gastrointestinal diseases is anti-inflammatory chamomile tea (1 tbsp. per glass of boiling water). You can drink it both before and after meals without any special restrictions.
A similar effect is provided by tea made from calendula flowers, which is prepared according to the same principle, but is drunk no more than 4 times a day an hour after meals. You can combine 2 plants in one drink: calendula and chamomile.
Linden tea, which many people are used to drinking when they have a cold or headache, is also useful for esophageal hernia. It can be consumed without restrictions as a healthy drink that does not increase stomach acidity. Linden tea with honey is especially tasty and healthy (1 teaspoon per glass of drink).
Patients with esophageal hernia can prepare vitamin tea from blackberry leaves and shoots (50 g of crushed plant material per 1 cup of boiling water), which can also be drunk without restrictions.
Teas made from mint and lemon balm, yarrow and St. John's wort, and licorice root help fight heartburn and hiccups. Tea made from raspberry leaves and fruits is a tasty vitamin drink. It is very useful to prepare drinks from the above-mentioned herbs, adding a little honey before drinking.
Living with a hiatal hernia
Perhaps, a hernia of the esophagus does cause some discomfort to patients, but life does not end with this diagnosis. Diet and drug treatment help to reduce the severity of the symptoms of the pathology. Breathing exercises and special physical exercises that train the abdominal and chest muscles help to restore the normal position of the stomach with a sliding hernia, eliminate dyspeptic symptoms, and reduce the likelihood of reflux. If these measures do not help, and the symptoms of the hernia of the esophagus do not subside, the patient is prepared for surgery.
Any disease leaves its mark on our life. So, a hernia of the esophagus requires certain restrictions from us. And this concerns not only nutrition, but also physical activity of a person, as well as the time of night rest.
A hernia of the esophageal orifice of the diaphragm is a pathology in which the esophagus and stomach are abnormally located, so it is not surprising that the symptoms intensify with a change in body position. So after the patient takes a horizontal position, the pain intensifies. But does this mean that a person should sleep in a sitting position? And if not, on which side can you sleep with an esophageal hernia?
There is no need to sleep standing or sitting with this disease, because proper rest is needed to maintain the body's strength and energy. But doctors recommend choosing a position lying on the right side, which reduces the load on the gastrointestinal tract due to their anatomical location and the likelihood of pinching. In addition, reflux usually does not occur with this body position, which means there will be no pain.
But no matter what position a person falls asleep in, they should not go to bed earlier than 2 hours after eating. This applies to healthy people, and is especially important for patients with a hiatal hernia.
There is also bad news for fans of alcoholic beverages. Esophageal hernia and alcohol are incompatible concepts. The fact is that alcoholic beverages, like coffee or black tea, are products that stimulate the secretion of gastric juice, and increased production of hydrochloric acid causes heartburn. In the case of reflux, this can play a cruel joke, causing severe irritation of the walls of the esophagus and even their perforation. And alcohol itself is an irritant, it is not for nothing that after taking it inside a person feels a burning sensation throughout the esophagus.
Another reason why you will have to give up regular alcohol consumption is the increased risk of developing inflammatory pathologies of the liver and pancreas, which become risk factors for increased intra-abdominal pressure, pushing the digestive organs through the opening of the diaphragm into the chest cavity.
Readers also have many questions on the topic of "esophageal hernia and the army." Most conscripts consider the presence of a hernia of the esophageal orifice of the diaphragm to be sufficient grounds for exemption from military service, and when this does not happen, the guys are very surprised. The fact is that only guys with the 3rd most severe degree of the disease are subject to mandatory exemption from military service (they are issued a military ID card based on their health condition), and for those diagnosed with the 1st degree, there are no restrictions, they serve on a general basis.
But there may be problems with the 2nd degree of esophageal hernia. According to the law, a conscript with such a pathology should be exempt from military service, he is enlisted in the reserve and issued a military ID for health reasons (Article 60 of the Schedule of Diseases, paragraph "b"). But in fact, to get such a conclusion, it is necessary to prove the presence of a 2nd degree hernia, i.e. undergo an X-ray with contrast, which is considered the "gold standard" for diagnosing an esophageal hernia. If there are no X-ray results, it will not be possible to get an exemption from military service.
Now, regarding physical activity and sports. Esophageal hernia is a pathology that does not require physical inactivity. On the contrary, for the digestive system to function normally, you need to move, otherwise you cannot avoid stagnation in the stomach and constipation, which are very dangerous with an esophageal hernia. Straining increases intra-abdominal pressure, which only complicates the situation, provoking the progression of the disease.
With a hernia of the esophageal opening of the diaphragm, walks in the fresh air, moderate physical activity, special exercise therapy, yoga, Pilates, and breathing exercises will be useful. But sports with a hernia of the esophagus are not available in full. For example, training the muscles of the chest press, running and swimming will not cause harm with a hernial protrusion, unlike weightlifting and other sports that involve stress on the abdominal muscles.
It is clear that in connection with the above, the question of whether it is possible to pump the press with an esophageal hernia disappears by itself. Such a load increases intra-abdominal pressure, which in turn provokes reflux and even greater protrusion of organs into the chest. To increase the tone of the abdominal muscles, the DFC complex includes special exercises that will not provoke complications of the disease.
For the same reason, patients are not recommended to wear bandages, tight elastic bands in pants, or tightly tightened belts and straps.
Can you squat with an esophageal hernia? This is a controversial issue. In general, according to gastroenterologists, squats, cycling and training on a stationary bike are not prohibited if you do them within reasonable limits. But squats with a load (with a load in your hands) are a completely different matter. With such exercises, as well as with lifting weights, the pressure in the abdominal cavity increases, which should not be allowed with a hernia. Any exercise should not provoke an increase in intra-abdominal pressure - this is an important requirement for all athletes and fans of a healthy lifestyle.
If a person wishes to continue playing sports after being diagnosed, they should first consult with a doctor who will help develop a safe training program and determine the types of sports permitted for this pathology.
And another important question: is disability possible with an esophageal hernia? On the one hand, if the hernia is not treated, over time it can progress and cause serious disruptions in the process of eating. Long-term irritation and inflammation of the esophagus lead to the appearance of esophageal strictures, which make it difficult for the food bolus to pass. But on the other hand, as long as this does not affect a person's ability to perform work, no one will give him disability.
Disability is possible only with esophageal stenosis, which limits vital functions and work performance in full. For example, the need for fractional meals with an esophageal hernia complicated by stenosis of the organ may be the reason for assigning Group 3 disability, which is considered working. Those who have been diagnosed with Grade 2 esophageal stenosis or have undergone organ reconstruction surgery (for the adaptation period) can count on Group 2.
And for the 1st group of disability, it is necessary to limit not only life activities, but also self-care, which is extremely rare with a hernia of the esophagus. The cause may be a strong narrowing of the esophagus and an extreme degree of exhaustion of the body caused by a nutritional disorder, as well as an operation in which 2 holes (stomas) are made in the neck and stomach, necessary for the communication of organs and the passage of food.
Usually, with appropriate treatment and diet, the prognosis for axial hernia is favorable. The symptoms of esophageal hernia subside after a course of treatment and the disease does not actually affect the quality of life of patients. However, the risk of complications of paraesophageal hernia remains even with active conservative treatment, so such patients are recommended to undergo surgical intervention.
Complications of hiatal hernia
A hernia of the esophageal orifice of the diaphragm is a progressive pathology, the symptoms of which become pronounced when the disease becomes complicated. The displacement of the peritoneal organs into the chest cavity itself is not a reason for the appearance of severe pain, so most patients indicate discomfort in the epigastrium and dull, aching pain behind the breastbone. But the appearance of sharp, cutting pain indicates inflammation of the hernia of the esophagus and the development of erosive and ulcerative processes.
Inflammation of the walls of the esophagus is associated with reflux esophagitis. Regular throwing of acidic contents of the stomach and duodenum into the lumen of the esophageal tube causes irritation of the walls of the esophagus and inflammation of the tissues. A long-term inflammatory process becomes a risk factor for the formation and increase in the volume of fibrous tissue, due to which the lumen of the esophagus narrows. And this becomes an obstacle to the consumption of solid food.
Hydrochloric acid and pepsin in the gastric juice can corrode the unprotected walls of the esophagus, causing erosions and ulcers (peptic ulcer of the esophagus). The irritating effect of these substances again leads to narrowing of the esophagus (peptic strictures).
Erosive and ulcerative damage to the walls of the esophagus can lead to their perforation, and then such symptoms of esophageal hernia as bloody vomiting and chocolate-colored stool appear. Frequent bleeding against the background of the chronic course of the disease in turn causes the development of iron deficiency anemia.
Chronic inflammatory-erosive changes in the esophagus increase the risk of degeneration of the organ wall cells and can cause esophageal cancer. No less dangerous is the strangulation of a hernia, in which the patient feels severe pain caused by a disruption in the flow of nutrients and oxygen to the organ and damage to nerve fibers.
During strangulation, the movement of food along the esophagus is limited, which passes with difficulty through the reduced lumen of the organ or cannot enter the stomach compressed by the diaphragm. This increases pain, causes nausea and vomiting, and does not allow a person to eat normally. With complete strangulation of the esophagus or stomach in the opening of the diaphragm, the patient cannot even drink, although this happens extremely rarely and requires emergency care.
During diagnostic procedures, a change in the color of the hernia can be seen. It becomes darker or grayish due to necrotic processes occurring in it, caused by tissue starvation and poisoning of the body with cell decay products. Necrotic changes in the tissues of the esophagus and stomach lead to a disruption of their functionality and can cause a serious condition provoked by sepsis.
Surgical treatment of the disease gives good results, but cannot completely exclude the recurrence of esophageal hernia, which, according to various data, occurs in 12-30% of cases in the late period after surgery. Plastic surgery of the diaphragmatic orifice helps prevent such a complication.
Many patients, noting the absence of previously observed symptoms, may think that the disease has passed, so on the Internet you can sometimes find questions on the topic of whether an esophageal hernia can disappear on its own? You should not count on it. The periodic disappearance and appearance of hernia symptoms is characteristic of the axial type of pathology, when the stomach and esophagus can shift in the opening of the diaphragm. Depending on this, symptoms may appear and disappear, which does not mean getting rid of the disease.
No medications can help restore the diaphragmatic opening to its original size and tone, they only prevent complications caused by reflux and spasm of the esophagus. Without treatment and non-compliance with the diet, the hernia will not only not disappear, but will continue to progress.

