Medical expert of the article
New publications
Preterm labor
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
According to WHO, premature birth is the birth of a child from the 22nd to the 37th full week of pregnancy (i.e. 259 days from the day of the last menstrual period). Triggers are premature rupture of membranes, infection and pregnancy pathology. The diagnosis is established on the basis of clinical data.
Treatment includes bed rest, tocolytics (if the pregnancy is prolonged), and glucocorticoids (if the gestational age is less than 34 weeks). Antistreptococcal antibiotics are given without waiting for negative culture results. Preterm labor may be caused by premature rupture of membranes, chorioamnionitis, or ascending uterine infection; the most common cause of such infections is group B streptococci. Preterm labor may occur with multiple pregnancies, preeclampsia or eclampsia, placental disorders, pyelonephritis, or certain sexually transmitted diseases; often the cause is unknown. Cervical cultures are performed to confirm causes identified during clinical examination.
In our country, premature birth is considered to be the birth of a child from the 28th to the 37th week of pregnancy (from the 196th to the 259th day from the beginning of the last menstruation). Spontaneous termination of pregnancy from 22 to 27 weeks is allocated to a separate category, not related to premature birth, and the child's data in the event of death are not included in the perinatal mortality indicators if the child did not survive 7 days after birth, which causes certain differences in the statistical data of Russian and foreign authors.
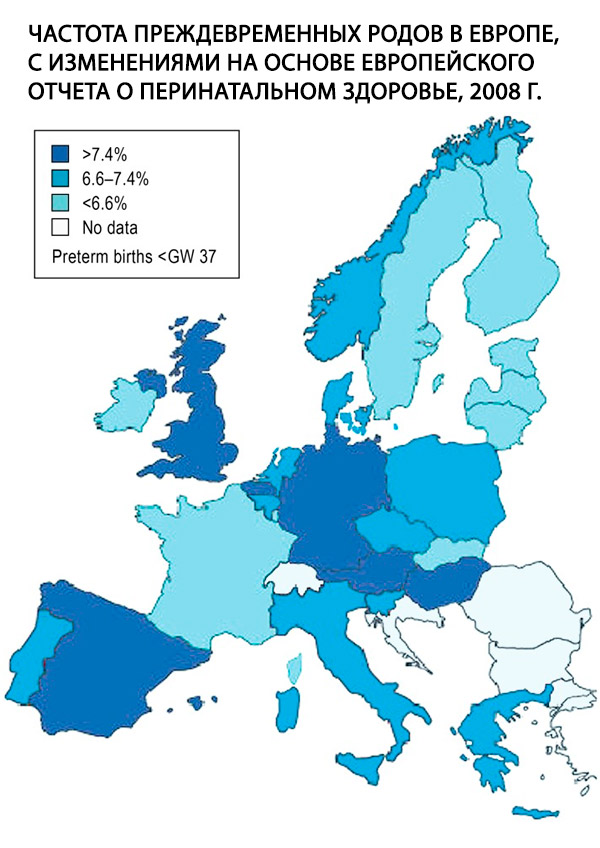
Preterm birth, defined as birth before gestational week (GN) 37+0, is a central problem in obstetrics and the single most important risk factor for perinatal morbidity and mortality. In 2011, 9% of all babies born in Germany were born before GN 37. This rate is high compared to most other European countries (Fig); it has remained stable over the past 10 years, but the rate of extremely preterm births, i.e. births before 28 years of pregnancy, has increased by 65%. Although the reasons for this development are not yet fully understood, it is largely explained by known demographic factors, such as the trend towards increasing maternal age at pregnancy and the increasing prevalence of diabetes mellitus. [ 1 ]
The incidence of premature births is 7–10% of all births, and, according to American authors, 9–10% of children are born before the 37th week, 6% before the 36th week, 2–3% before the 33rd week. The causes of perinatal mortality in 50–70% of cases are complications due to premature birth [4, 53]. Over the past 30 years, the incidence of premature births has remained stable, but an improvement in the prognosis for newborns has been noted due to the development of neonatal medicine.
In foreign literature, groups of newborns are distinguished:
- with a body weight from 2500 to 1500 g - low birth weight infants (LВW);
- with a body weight of less than 1500 g - very low birth weight infants (VLВW);
- with extremely low body weight, which constitute a risk group for developing paralysis, severe neurological disorders, blindness, deafness, dysfunctional disorders of the respiratory, digestive, genitourinary systems and are characterized by the highest mortality rate.
According to American authors, 50% of neonatal losses are registered among newborns weighing less than 2500 g, making up only 1.5% of all children born. According to British authors, the survival rate of children born weighing less than 1500 g, thanks to the success of neonatal services, is about 85%, but 25% of them have severe neurological disorders, 30% have hearing and vision disorders, 40-60% experience difficulties in the learning and education process.
Risk factors for premature birth include a woman's low socioeconomic standard of living, age (under 18 and over 30 years), unfavorable working conditions, heavy smoking (more than 10 cigarettes a day), drug use (especially cocaine), and obstetric history - a history of one premature birth increases the risk of its occurrence in a subsequent pregnancy by 4 times, and two premature births - by 6 times.
Complications that contribute to the development of premature birth:
- intrauterine infection (chorioamnionitis);
- premature rupture of membranes, with or without chorioamnionitis;
- isthmic-cervical insufficiency;
- detachment of normal or low-lying placenta;
- factors leading to overstretching of the uterus (polyhydramnios, multiple pregnancy, macrosomia in diabetes);
- malformations of the uterus, uterine fibroids (disruption of spatial relationships, ischemic degenerative changes in the node);
- upper urinary tract infections (pyelonephritis, asymptomatic bacteriuria);
- surgical operations during pregnancy, especially on abdominal organs;
- injuries;
- extragenital diseases that disrupt metabolic processes in a pregnant woman and lead to intrauterine suffering of the fetus (arterial hypertension, bronchial asthma, hyperthyroidism, heart disease, anemia with a hemoglobin level of less than 90 g/l);
- drug addiction, heavy smoking.
About 30% of all cases of spontaneous preterm birth are caused by infection, and among children born before 30 weeks of pregnancy, histologically verified chorioamnionitis is noted in 80% of cases.
Spontaneous premature birth
In terms of labor management tactics, it is important to distinguish between spontaneous premature labor, which begins with regular labor activity with the amniotic sac intact (40–50%), and premature labor, which begins with the rupture of amniotic fluid in the absence of labor activity (30–40%).
Induced preterm labor (20%)
They arise in situations requiring termination of pregnancy for reasons related to the health of the mother or fetus. Indications from the mother are related to:
- with severe extragenital pathology, in which prolongation of pregnancy is dangerous to the woman’s health;
- with complications of pregnancy: severe gestosis, hepatosis, multiple organ failure, etc.
Indications from the fetus:
- fetal malformations incompatible with life;
- antenatal fetal death;
- progressive deterioration of the fetus's condition according to CTG and Doppler ultrasound data, requiring delivery, resuscitation measures and intensive care.
The purpose of the diagnostic examination is to identify conditions that predispose to premature birth (ascending infection, placental insufficiency, changes in amniotic fluid, etc.), as well as an objective assessment of the degree of premature birth that has already begun (characteristics of contractions, the effect of contractions on the cervix, premature rupture of membranes). In addition, it is necessary to assess the condition of the fetus to determine whether there is a need for labor.
How to recognize premature birth?
 [ 13 ]
[ 13 ]
The goal of all interventions is not simply to prolong the pregnancy itself, but rather to give the newborn baby the best chance of survival with as few complications as possible. Thus, depending on the specific clinical situation, the method of choice may be either prolongation of the pregnancy or delivery of the baby.
However, as a rule, the important goal is to prolong the pregnancy for at least 48 hours so that the pregnant woman can be transferred to a high-level perinatal center and fetal lung maturation can be induced with glucocorticoids. These two measures have been shown to improve survival in infants born before 34 gestational ages.
Premature birth is treated with the following measures:
- inhibition of uterine contractions with drugs - tocolysis (for indications and contraindications, see the box)
- administration of glucocorticoids to stimulate fetal lung maturation
- treatment of local or systemic infection with antibiotics
- avoidance of physical activity - bed rest and hospitalization.
Read more: Premature Birth - Treatment
Primary prevention
The goal of primary prevention is to reduce the overall incidence of preterm birth by improving overall maternal health and eliminating risk factors before or during pregnancy. [ 14 ]
Quitting smoking by itself significantly reduces the risk of preterm birth. On the other hand, underweight or obese mothers, with a body mass index (BMI) above 35, have a significantly higher risk of preterm birth. Mothers should seek nutritional counseling. Women with stressful jobs may be advised by their doctors to reduce their workload or even stop working temporarily to reduce the risk of preterm birth.
The goal of secondary prevention is the early identification of pregnant women at increased risk of preterm birth in order to help these women carry their pregnancies to term.
Main risk factors
- Poor nutrition and inadequate nutrition.
- Multiple pregnancy.
- Mother's age.
- Unfavorable life situation.
- History of premature birth or miscarriage.
Secondary prevention measures
Self-measurement of vaginal pH
As originally described by E. Saling, vaginal pH can be used as a marker for bacterial vaginosis, which in turn increases the risk of preterm birth by 2.4 times. [ 15 ] If the pH is elevated, antibiotics are prescribed.
Measuring cervical length using transvaginal ultrasound
The usefulness of transvaginal cervical length measurement for assessing the risk of preterm birth has been well documented in a structured analysis of 14 studies involving a total of 2258 pregnant women.[ 16 ] The accepted cutoff value for cervical length is ≤ 25 to 24 years of gestation. The negative predictive value of a negative test is high (92%), meaning that pregnant women found to have a normal short cervix can be reassured and unnecessary therapeutic measures can be avoided.
Cerclage and complete closure of the birth canal
Cervical cerclage is a commonly performed procedure to stabilize and mechanically close the cervical canal, much like a purse-string suture. Prophylactic early complete closure of the birth canal, as described by Seiling, is intended to prevent ascending infection, but its benefit has not been documented in prospective randomized trials. German and foreign obstetric societies have not issued any binding recommendations on the indications and/or technique of either of these interventions. A meta-analysis has shown that, at least for a certain group of high-risk pregnant women with a history of preterm birth and a short cervix, perinatal morbidity and mortality can be significantly reduced. [ 17 ]
The goal of secondary prevention is...the early identification of pregnant women at increased risk of preterm birth in order to help these women carry their pregnancies to term.
Progesterone supplements
The most important advance in the last decade has been the introduction of progesterone supplements to prevent preterm birth. The likelihood of preterm birth can be reduced by more than 30% in both women with a history of preterm birth [ 18 ] and those with a shortened cervix. [ 19 ]
Progesterone can also be used successfully for secondary prophylaxis after tocolysis, although no benefit has been demonstrated in twin pregnancies. Available data support the recommendation that all pregnant women with a history of increased risk or current asymptomatic cervical insufficiency should receive progesterone supplementation until the end of 34 GA.

