Medical expert of the article
New publications
Presacral blockade
Last reviewed: 03.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A medical anesthetic procedure used in proctology and surgery is a presacral block. Let's consider the indications for its implementation, technique, complications.
Any part of the nervous system, when exposed to certain factors, can become a permanent or temporary source of neurodystrophic disorders in the body. Irritation causes parabiosis of nerves in the affected area, which complicates the transmission of impulses from receptors to nerves and back.
Advantages of therapeutic blockades:
- Possibility of multiple use for therapeutic purposes.
- Minimal risk of complications (the drug is administered locally, so it enters the general bloodstream in minimal quantities).
- Effective and rapid relief of pain (local administration of anesthetic reduces or completely eliminates discomfort).
Presacral or pararectal blockade is a method of local anesthesia, i.e. it anesthetizes the affected area. Due to this, the procedure is used in many operations and manipulations on the anus, injuries to the sacrum, coccyx and pelvis.
Indications for the procedure
The main indication for the use of presacral block is the relief of severe pain. The purpose of the procedure is to relieve acute pain in the coccyx and sacrum.
The technique is based on temporary blocking of nerve signals in a specific area. The anesthetic blocks the hypogastric and sacrococcygeal nerve plexuses. The procedure quickly eliminates physical and psycho-emotional problems. [ 1 ]
Presacral block is indicated in the following conditions:
- Acute hemorrhoids.
- Anal fissures.
- Sacral injuries.
- Prostatitis.
- Priapism.
- Cystalgia.
- Coccygodynia.
- Premature ejaculation.
- Injuries to the limbs, pelvis, chest.
- Renal and hepatic colic.
- Obstetric and gynecological pathologies.
The pain-relieving effect of the blockade occurs immediately. The anesthetic saturates the mucous membrane, blocks the surrounding nerve endings and the inflammation site. The procedure also reduces the permeability of the vascular walls, suppresses the growth of pathogenic microflora, reduces sensitivity to allergens and relieves smooth muscle spasms. [ 2 ]
Preparation
Local anesthetics affect the functional state of the nerve, disrupting its excitability and conductivity. A reversible process of so-called parabiotic inhibition develops in the nerve, which prevents the passage of impulses.
As before any medical procedure, before performing a presacral block, the patient undergoes special preparation. It consists of a cleansing enema on the day of the manipulation. If the block is performed due to severe pain syndrome, then no preparation is required. The doctor also asks the patient about the presence of contraindications to the use of medicinal anesthetics.
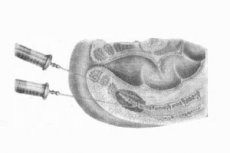
Technique of a presacral blockade
Presacral block involves the injection of anesthetic into the area in front of the first and second sacral foramina on one or both sides.
The technique for performing a presacral block includes:
- Before the procedure, the patient's allergy history should be clarified.
- Strict adherence to aseptic technique was observed.
- Before the puncture, intradermal anesthesia is performed in the area where the needle is inserted.
- For the blockade, long needles of 10-20 cm and syringes of 10-20 ml are used.
- The needle is inserted slowly to avoid damaging nerves and blood vessels.
- After the procedure, the patient is recommended to stay in bed for 1-2 hours.
The procedure is performed in the doctor’s office in a proctology/gynecology chair or on a couch (the patient is placed on her side, pulling her knees up to her stomach). [ 3 ]
The blockade is performed with a long needle, introducing anesthesia 2 cm to the side and ventrally from the top of the coccyx, in the direction of the first and second sacral openings. The needle's movement is controlled with a finger through the patient's rectum. About 50 ml of 0.5% novocaine solution is injected before the first and second sacrum, the maximum dose is 150 ml of 0.5% solution.
Presacral novocaine block
Novocaine is a local anesthetic drug. The drug blocks sensitive nerve fibers and endings, producing an anesthetic effect. The drug has a wide range of therapeutic applications. Its introduction and absorption into the bloodstream has the following effects on the body:
- Reduces the excitability of peripheral cholinergic systems.
- Reduces the formation of acetylcholine.
- Reduces smooth muscle spasms.
- Reduces excitability of the heart muscle and motor areas of the cerebral cortex.
- Toxic doses cause excitation and paralysis of the central nervous system.
Presacral novocaine block is prescribed to reduce or completely relieve pain. The procedure is performed for various neurological, surgical and traumatological pathologies.
Indications for blockade:
- Limb injuries.
- Pelvic and chest injuries.
- Frostbite.
- Renal and hepatic colic.
- Acute hemorrhoids.
- Sacral injuries.
- Obstetric and gynecological diseases and others.
Once in the body, novocaine is rapidly hydrolyzed, forming pharmacologically active substances: diethylaminoethanol and para-aminobenzoic acid. The drug has a rapid and at the same time short-term effect. To reduce its absorption and prolong the effect, when performing local anesthesia, a 0.1% solution of adrenaline hydrochloride is added to the solution (1 drop per 2-10 ml of novocaine). [ 4 ]
If the drug is used for local anesthesia, its quantity and concentration directly depend on the nature of the surgical intervention, the method of administration, and the patient's body weight. The procedure is not performed in cases of allergic reactions to novocaine, peritonitis, systemic infections, terminal conditions, during pregnancy, and for patients under 18 years of age.
Novocaine blockade has a complex effect on both the central nervous system and the peripheral nervous system. Due to this, the cerebral cortex is freed from strong pain impulses. Strong irritation goes away, the reflex-trophic function of the nervous system is restored. As a result of the blockade, tissue trophism improves and the disease acquires a favorable course. [ 5 ]
Contraindications to the procedure
Pararectal blockades are placed in the area adjacent to the pain source, in some cases in the pain source itself. Despite the effective analgesic effect, the procedure has a number of contraindications:
- Inflammatory processes on the skin in the area where the anesthetic is administered.
- Individual intolerance to the drug/local anesthetics.
- Collapse, terminal states.
- Pathologies associated with the destruction of the sheath of nerve endings (myelin).
- Tissue abscess formation.
- Persistent hypotension, arrhythmia.
- Presence of inoperable neoplasms.
- Bleeding.
- Peritonitis, septicemia.
The procedure is performed in an outpatient setting, i.e. under complete sterility. Before performing the blockade, the doctor clarifies whether the patient has the above contraindications and assesses the risk of complications. [ 6 ]
Complications after the procedure
Pararectal therapeutic blockade is a low-trauma procedure with a minimal risk of complications. In most cases, problems arise when the rules of asepsis and antisepsis, the technique of implementation and individual reactions of the patient's body are violated.
The following complications are distinguished:
- Subcutaneous paraproctitis at injection sites.
- Overdose of local antiseptic and its toxic effect on the body.
- Injection of the solution into a blood vessel (risk of developing a toxic effect. An aspiration test is indicated to prevent this).
- Various anaphylactic reactions.
- Infection of deep tissues (infiltrates, abscesses, phlegmons).
- Bleeding.
The risk of complications increases significantly when administering combined solutions. To prevent anaphylactic, toxic and other reactions, an allergic history should be collected and the possibility of interactions between different drugs should be taken into account.
Consequences after the procedure
According to medical statistics, consequences after presacral block develop extremely rarely, but it is necessary to remember the risk of their occurrence.
Post-procedural consequences are divided into two groups:
1. Local:
- Severe pain.
- Swelling.
- Bruising.
- Tissue necrosis.
- Non-specific inflammatory processes.
2. General:
- Allergic reactions (low blood pressure, swelling, itching, rash, respiratory failure).
- Toxic (headaches and dizziness, tachycardia, coma).
- Traumatic (impaired sensitivity, hematomas).
- Inflammatory reactions.
Therapeutic blockade is a highly effective method of pain relief, but only the attending physician can prescribe and perform it. The doctor evaluates the patient's condition, the possible effectiveness of the blockade, introduces the technique of its implementation and the features of the post-procedural state. [ 7 ]
Care after the procedure
Pararectal blockade is performed in an outpatient setting using anesthetics. If the patient feels well, he or she can leave the hospital and return to their normal lifestyle immediately after the procedure.
Very rarely, patients complain of general weakness, dizziness and other painful symptoms. In this case, the patient is left in the hospital until the general well-being improves (this does not take more than an hour).
If the presacral block was performed for the purpose of surgical intervention, the patient may require longer observation and supportive therapy. In this case, the patient is informed that local anesthesia works for 1-1.5 hours, after which painful sensations may occur, which disappear within a few hours.
Reviews
According to numerous reviews, presacral block is an effective local anesthetic. At the same time, the procedure has a minimal impact on the body, unlike general anesthesia. That is, recovery after the block does not require effort, and the risk of complications is minimal.

