Medical expert of the article
New publications
Non-tuberculous mycobacteria
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
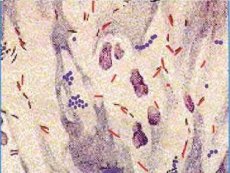
Non-tuberculous mycobacteria are independent species, widespread in the environment as saprophytes, which in some cases can cause severe diseases - mycobacteriosis. They are also called environmental mycobacteria, causative agents of mycobacteriosis, opportunistic and atypical mycobacteria. A significant difference between non-tuberculous mycobacteria and mycobacterium tuberculosis complex is that they are practically not transmitted from person to person.
Non-tuberculous mycobacteria are divided into 4 groups based on a limited number of characteristics: growth rate, pigment formation, colony morphology, and biochemical properties.
1st group - slow-growing photochromogenic (M. kansasii, etc.). The main feature of representatives of this group is the appearance of pigment in the light. They form colonies from S to RS-forms, contain carotene crystals, coloring them yellow. The growth rate is from 7 to 20 days at 25, 37 and 40 °C, catadase-positive.
M. kansasii are yellow bacilli that live in water and soil and most often affect the lungs. These bacteria can be identified by their large size and cruciform arrangement. An important manifestation of infections caused by M. kansasii is the development of disseminated disease. Skin and soft tissue lesions, the development of tenosynovitis, osteomyelitis, lymphadenitis, pericarditis and urogenital tract infections are also possible.
2nd group - slow-growing scotochromogenic (M. scrofulaceum, M. matmoense, M. gordonae, etc.). Microorganisms form yellow colonies in the dark and orange or reddish colonies in the light, usually S-shaped colonies, grow at 37 °C. This is the most numerous group of non-tuberculous mycobacteria. They are isolated from contaminated water bodies and soil and have low pathogenicity for humans and animals.
M. scrofulaceum (from English scrofula - scrofula) is one of the main causes of cervical lymphadenitis in children under 5 years of age. In the presence of severe concomitant diseases, they can cause damage to the lungs, bones and soft tissues. In addition to water and soil, microbes have been isolated from raw milk and other dairy products.
M. maimoense are microaerophiles, forming greyish-white, smooth, shiny, opaque, dome-shaped, round colonies.
Primary isolates grow very slowly at 22-37°C. Exposure to light does not cause pigment production. If necessary, exposure can be continued for up to 12 weeks. In humans, they cause chronic lung disease.
M. gordonae are the most common recognized saprophytes, scotochromogens of tap water, and cause mycobacteriosis extremely rarely. In addition to water (known as M. aquae), they are often isolated from soil, gastric lavage, bronchial secretions, or other material from patients, but in most cases they are nonpathogenic to humans. At the same time, there are reports of cases of meningitis, peritonitis, and skin lesions caused by this type of mycobacteria.
Group 3 - slow-growing non-chromogenic mycobacteria (M. avium complex, M. gaslri M. terrae complex, etc.). They form colorless S- or SR- and R-forms of colonies, which can have light yellow and cream shades. They are isolated from sick animals, water and soil.
M. avium - M. inlracellulare are combined into one M. avium complex, since their interspecies differentiation presents certain difficulties. Microorganisms grow at 25-45 °C, are pathogenic for birds, less pathogenic for cattle, pigs, sheep, dogs, and are not pathogenic for guinea pigs. Most often, these microorganisms cause lung lesions in humans. Lesions of the skin, muscle tissue, and skeletal system, as well as disseminated forms of diseases, have been described. They are among the causative agents of opportunistic infections that complicate acquired immunodeficiency syndrome (AIDS). M. avium subspecies paratuberculosis is the causative agent of Jones disease in cattle and, possibly, Crohn's disease (a chronic inflammatory disease of the gastrointestinal tract) in humans. The microbe is present in meat, milk, and feces of infected cows, and is also found in water and soil. Standard water purification methods do not inactivate this microbe.
M. xenopi causes lung lesions in humans and disseminated forms of disease associated with AIDS. They are isolated from frogs of the genus Xenopus. The bacteria form small, smooth, shiny, non-pigmented colonies that subsequently turn bright yellow. Thermophiles do not grow at 22 °C and grow well at 37 and 45 °C. When examined with bacterioscopy, they look like very thin rods, tapering at one end and arranged parallel to each other (like a picket fence). They are often isolated from cold and hot tap water, including drinking water stored in hospital reservoirs (nosocomial outbreaks). Unlike other opportunistic mycobacteria, they are sensitive to most anti-tuberculosis drugs.
M. ukerans is the etiologic agent of mycobacterial cutaneous N (Buruli ulcer), grows only at 30-33 °C, colony growth is noted only after 7 weeks. The pathogen is also released when mice are infected in the pulp of the sole of the paw. This disease is common in Australia and Africa. The source of infection is the tropical environment and BCG vaccination against this mycobacteriosis.
Group 4 - fast-growing mycobacteria (M. fortuitum complex, M. phlei, M. xmegmatis, etc.). Their growth is observed in the form of R- or S-form colonies for 1-2 to 7 days. They are found in water, soil, sewage and are representatives of the normal microflora of the human body. Bacteria of this group are rarely isolated from pathological material from patients, but some of them have clinical significance.
M. fortuitum complex includes M. fortuitum and M. chcionae, which consist of subspecies. They cause disseminated processes, skin and postoperative infections, lung diseases. Microbes of this complex are highly resistant to anti-tuberculosis drugs.
M smegmatis is a representative of normal microflora, isolated from smegma in men. It grows well at 45 °C. As a causative agent of human diseases, it ranks second among fast-growing mycobacteria after the M. fortuitum complex. It affects the skin and soft tissues. Tuberculosis pathogens must be differentiated from M. smegmatis when examining urine.
Most often, mycobacteriosis is caused by representatives of groups 3 and 1.
Epidemiology of mycobacteriosis
The causative agents of mycobacteriosis are widespread in nature. They can be found in soil, dust, peat, mud, river water, ponds and swimming pools. They are found in ticks and fish, cause diseases in birds, wild and domestic animals, and are representatives of the normal microflora of the mucous membranes of the upper respiratory tract and the urogenital tract in humans. Infection with non-tuberculous mycobacteria occurs from the environment through airborne transmission, contact with damage to the skin, as well as through food and water. Transmission of microorganisms from person to person is uncommon. These are opportunistic bacteria, so a decrease in the resistance of the macroorganism and its genetic predisposition are of great importance in the development of the disease. Granulomas form in the affected areas. In severe cases, phagocytosis is incomplete, bacteremia is pronounced, and macrophages filled with non-tuberculous mycobacteria and resembling leprosy cells are detected in the organs.
Symptoms of mycobacteriosis
The symptoms of mycobacteriosis are varied. The respiratory system is most often affected. The symptoms of pulmonary pathology are similar to those of tuberculosis. However, there are frequent cases of extrapulmonary localization of the process involving the skin and subcutaneous tissue, wound surfaces, lymph nodes, genitourinary organs, bones and joints, as well as the meninges. Organ lesions can begin both acutely and latent, but almost always proceed severely,
The development of a mixed infection is also possible; in some cases, they can be the cause of the development of a secondary endogenous infection.
Microbiological diagnostics of mycobacteriosis
The main method of diagnosing mycobacteriosis is bacteriological. The material for the study is taken based on the pathogenesis and clinical manifestations of the disease. Initially, the question is decided whether the isolated pure culture belongs to the causative agents of tuberculosis or non-tuberculous mycobacteria. Then a set of studies is used to establish the type of mycobacteria, the degree of virulence, and the Runyon group. Primary identification is based on such features as growth rate, ability to form pigment, colony morphology, and ability to grow at different temperatures. To identify these features, no additional equipment or reagents are required, so they can be used in basic laboratories of tuberculosis dispensaries. Final identification (reference identification) using complex biochemical studies is carried out in specialized moratoriums of scientific institutions. In most cases, preference is given to their identification by biochemical facts such as modern molecular genetic methods are labor-intensive, have many preparatory stages, require special equipment, and are expensive. Determination of sensitivity to antibiotics is of great importance for the treatment. The criterion of simultaneous appearance of clinical, radiological, laboratory data and isolation of pure culture of non-tuberculous mycobacteria, conducting multiple studies in dynamics are of decisive importance for the diagnosis of mycobacteriosis.
Of auxiliary importance in diagnostics are the determination of antitheses using RNGA, RP, immunoelectrophoresis, RNIF and ELISA, as well as the performance of skin allergy tests with sensitins.
Treatment and specific prevention of mycobacteriosis
All types of non-tuberculous mycobacteria, with the exception of M. xenopi, are resistant to isoniazid, streptomycin and thiosemicarbazones. Treatment of mycobacteriosis with anti-tuberculosis and antibacterial drugs should be long-term (12-13 months) and combined. It is usually ineffective in MAC infections and diseases caused by fast-growing mycobacteria. In some cases, surgical treatment is used. Drugs for specific prevention of mycobacteriosis have not been developed.


 [
[