Medical expert of the article
New publications
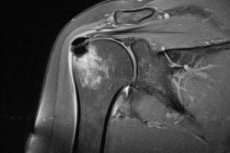
Shoulder MRI
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
It is not for nothing that MRI of the shoulder joint is one of the most effective and safe methods of diagnosing pathologies of bones, joints and soft tissues located in this area. X-rays, popular in the past, which affect the body with unsafe ionizing radiation, are no longer as relevant as magnetic resonance imaging, which does not use harmful rays. And although the danger of X-ray radiation used in modern X-ray and computer tomography devices is significantly exaggerated, human health is still put in the foreground.
And if we consider that in addition to undergoing an annual X-ray examination, we are exposed to dangerous radiation every day at home, at work, on vacation, while traveling by plane, etc., then the value of MRI is quite high, since the study makes it possible to obtain the information necessary for diagnosis without additional radiation.
Anatomy of the shoulder joint
The shoulder is commonly referred to as the uppermost part of the arm, adjacent to the shoulder blade. In fact, the shoulder is a structure formed by three bones: the shoulder blade, the collarbone, and the humerus, which is the upper half of the arm.
The human shoulder is a fairly mobile organ. Its movement involves two joints: the acromioclavicular joint (the junction of the collarbone and the scapula) and the humeral joint (the place where the rounded end of the humerus enters the cup-shaped cavity of the scapula). It is the humeral joint that is popularly associated with the shoulder, and thanks to this joint, we have the opportunity to perform a wide range of hand movements. And MRI of the shoulder joint allows us to examine this complex structure in detail and assess the degree of its functionality.
The bones in the joint area are covered with strong cartilaginous tissue, allowing the joint to move freely and serving as a kind of shock absorber during impacts. The joint itself is surrounded by connective tissue, which forms a protective capsule. Inside, the capsule is covered with a thin but fairly strong membrane called the synovial membrane. It is in this membrane that the synthesis of fluid occurs, which is intended to lubricate the joints and reduce friction when moving the hand (synovial fluid).
What other important components have we missed when considering the structure of the shoulder joint:
- Articular (or cartilaginous) labrum. This is the name given to the tissue consisting of collagen and elastic fibers covering the glenoid cavity. This is a type of connective tissue that is also called fibrous. It increases the surface of the cavity so that the cavity corresponds to the size of the humeral head. Fibrous tissue is necessary to stabilize the joint at the junction of different bones.
- Rotator cuff. It is represented by a complex of two types of soft tissues: muscles and tendons. These tissues are the covering for the shoulder joint. They also provide rotational movement of the arm and the bone-cartilaginous joint itself.
- Deltoid muscle. It is thanks to the presence of this powerful muscle that we have the ability to lift our arm and various weights.
- The tendon of the two-headed muscle of the arm, called the biceps (the pride of bodybuilders, because it is by the size of this muscle that the beauty of the physique and the strength of the arms are assessed). This strong tissue is responsible for bending the arm at the elbow and allows you to rotate the forearm.
During an MRI, the doctor has the opportunity not only to repeat the anatomy of the shoulder, but also to identify pathological changes in various parts of the shoulder joint.
Indications for the procedure
And yet, despite all the safety of magnetic resonance imaging, this diagnostic method is used in a limited framework. That is, MRI of the shoulder joint is performed only in certain cases when the doctor has difficulty making a diagnosis based on the results of a physical examination and the patient's complaints.
In what cases may additional research be required:
- if there is a suspicion of inflammatory-degenerative pathologies of the shoulder joint, such as arthritis or arthrosis,
- in case of fractures of the bones of the shoulder joint (not only to make an accurate diagnosis, but also to assess the location of bone fragments),
- if there is a suspicion of damage to the rotator cuff of the shoulder (this can be either a tendon rupture or compression of the joint and tendon bag, accompanied by pain in people over 40 years of age and called impingement syndrome),
- in case of traumatic injuries to the shoulder (tear of the cartilaginous labrum, ligament ruptures in the shoulder joint area, etc.),
- in case of sports injuries (for example, a severe bruise or dislocation of the shoulder),
- in case of injuries caused by the specifics of work activities (such injuries can result, for example, from working with tools that cause strong vibration),
- if there is a suspicion of infectious and inflammatory processes in the hard and soft tissues of the shoulder joint,
- in tumor processes (helps to determine the location and size of the tumor, as well as to identify metastases in bones and soft tissues),
- if pain, swelling and hematomas of unknown origin appear in the shoulder area,
- in case of progressive pain syndrome in the shoulder area if drug therapy does not produce results,
- with limited mobility of the shoulder,
MRI of the shoulder joint is one of the most effective diagnostic methods, allowing to detect even hidden pathologies. But this method is also used to evaluate the results of surgical treatment. In this case, tomography can be performed both with contrast (which is relevant for tumor processes and vascular pathologies) and without it.
Preparation
MRI of the shoulder joint is considered a completely safe procedure, so it does not require any special preparation. On the eve of the examination, a person can safely consume various types of food and drinks. He or she is not required to limit his or her activities. A person can perform work and household duties as much as the injury or illness that was the indication for MRI diagnostics allows. There is no need to change the daily routine.
Even if MRI is performed with contrast, examination of the shoulder joint does not impose any restrictions on patients. The only thing that may be required is an allergy test to avoid intolerance reactions during intravenous injection of the dye. However, contrast agents are used for diagnostic purposes, which very rarely cause allergic reactions.
The doctor may advise the patient to skip breakfast on the day of the procedure and stick to a light diet the day before. This will help avoid nausea after the injection of the contrast agent.
As part of preparation for MRI diagnostics, a doctor conducts a physical examination of the patient and studies the patient's medical history. This allows a preliminary diagnosis to be made. At the same time, the doctor receives the necessary information about the patient's health condition, including the risk of adverse reactions to contrast.
If the person being examined has implants built into their body, it is essential to notify the doctor about this. After all, some metal alloys can distort the magnetic field of the device, introducing undesirable adjustments to the information it receives, and electronic stimulators themselves can experience malfunctions.
If the patient has had previous injuries or diseases of the bones and joints of the shoulder girdle, it is advisable to provide the doctor with previously taken X-rays or MRI results. This will help to avoid false conclusions when interpreting new results.
When prescribing a diagnostic method such as MRI to a patient, the doctor must explain in detail how the procedure will be performed, what can and cannot be done during it. If certain preparation is required, the patient must also be informed about this.
If the patient is a woman, she should be warned that makeup often includes components containing metal particles. Therefore, it is better to refrain from using it before the procedure. You should also avoid wearing jewelry made of different metals, because you will still be asked to remove them before the diagnostic procedures. In addition to jewelry, the patient will be asked to remove and leave all metal-containing items. This includes watches, keys, belts with metal buckles. This list can also include clothing with rivets and zippers, all kinds of pins used against the evil eye or as jewelry, a knife, ballpoint and fountain pens and rods with metal tips, glasses with metal parts. You will also have to leave bank cards with a ferromagnetic strip. Removable metal dentures are no exception.
In private clinics, patients are given a special robe, which a person must wear during the procedure. But it is not forbidden to take light home clothes with you to the diagnostics.
 [ 8 ]
[ 8 ]
Technique Shoulder MRI
It should be said that the MRI technique of the shoulder joint does not present any technical complexity. For diagnostics, universal devices are used that create a magnetic field inside, safe for humans, but sufficient to obtain information about the state of the hard and soft tissues of the body.
MRI of the shoulder joint allows you to get a clear image on a computer screen or film of ligaments, tendons, cartilage, bones, i.e. all structures of the shoulder girdle and makes it possible to record any changes in their condition.
The human body consists of more than 70 percent water, and one of the components of this substance is hydrogen molecules (we know this from our school chemistry course). The nuclei of hydrogen atoms placed in a magnetic field begin to absorb electromagnetic pulses coming from the device. The latter cause vibrations of the atoms. These signals are captured by the device. And since the reflection of signals in tissues of different density is not the same, a picture appears on the screen, individual elements of which have colors of different intensity.
In order to obtain such a picture, the patient (or rather the part of his body that is being studied) must be inside the device. The person is placed on a sliding table, where he will remain until the end of the study. During the procedure, the table will be inside the device, but the person always has the opportunity to contact the technician in another room via speakerphone in case questions arise or the condition worsens. The patient will receive instructions from the doctor in the same way.
During the examination of bones and joints, a person must remain motionless throughout the procedure, which is at least 15-20 minutes. Overly excitable patients and children are recommended to undergo sedation (taking sedatives) before the procedure. It is also possible to fix certain parts of the body with belts provided for this purpose.
The procedure of being in the confined space of the device is most difficult for people with claustrophobia. It is recommended to put them into a drug-induced sleep beforehand, which will help to avoid panic and movements.
If an MRI of the shoulder joint is performed with contrast, the patient will be injected with a contrast agent in advance. When examining the structures of the shoulder, this is an intravenous injection. After a few minutes, diagnostic procedures can be performed.
What does an MRI of the shoulder joint show?
Magnetic resonance imaging is a unique method of obtaining information hidden inside the body, which is necessary for making an accurate diagnosis. Quite often, laboratory tests, physical examination and patient complaints about pain and limited movement in the shoulder do not provide enough information for a specialist to understand what pathology is causing such symptoms. Only instrumental studies can obtain more accurate and specific information about the condition of the shoulder joint, the nature of its damage and even the degree of development of the pathological process.
The patient is prescribed one of the examination methods: radiography, ultrasound, computed tomography, magnetic resonance imaging. Sometimes these examinations are prescribed in combination. The relevance of such diagnostics is especially evident when it comes to simultaneous damage to various joint structures.
But for the study of the shoulder joint, the safest and most informative method is considered to be Magnetic Resonance Imaging (MRI). This is a non-invasive and painless method of obtaining information about the internal structures of a person without the use of dangerous ionizing radiation.
The previously popular X-ray diagnostics is not only dangerous in itself due to the use of X-rays, which are ionizing radiation, but also does not provide enough information about the soft tissues in the shoulder girdle. But MRI, in addition to hard tissues, allows you to visualize soft tissue structures: muscles, ligaments, tendons, cartilage, synovial bag of the joint. Any changes in them (ruptures and cracks in tendons, changes in the shape and density of various tissues, bone fractures, the appearance of unusual neoplasms, etc.) can be seen on the computer screen to which the tomograph transmits information. MRI also allows you to diagnose pathologies of the nerves and blood vessels of the shoulder.
The doctor gets the opportunity not only to distinguish inflammatory-degenerative changes in structures from fractures and sprains, but also to establish the nature of these changes, as well as to say how serious the situation is and what treatment methods will be most effective in this case.
If surgery is required, it is useful to have a repeat MRI of the shoulder joint after surgery. This will help the surgeon understand whether he did everything correctly, whether additional surgeries are required, and, if possible, prescribe further treatment.
It should be said that ultrasound also provides sufficient information about the condition of soft tissues, but MRI is considered more informative, since it allows recording the slightest pathological changes in soft and hard tissues, which makes it possible to diagnose the disease at an early stage. And when it comes to tumor processes, this point is vital. At the same time, visualization of bone tissue on MRI is more detailed than on ultrasound.
If the question arises about what is better CT or MRI of the shoulder joint, it is necessary to understand that, despite the high information content of both methods, each of the methods has its pros and cons. For example, MRI provides more information about soft tissue damage, while a CT scan is more informative when it comes to bone pathologies.
In principle, both CT and MRI provide the doctor with enough information to diagnose various shoulder girdle pathologies. But it should be taken into account that X-rays are used during CT scanning, which means that this examination can be considered less safe than MRI. This is especially important when diagnostics are prescribed to children.
Contraindications to the procedure
Although MRI of the shoulder joint is considered the safest method for diagnosing shoulder diseases, like any other method, it has its contraindications. It should be said that there are few such contraindications, and most of them are still associated with metal implants.
Recalling the information about the properties of metals from the school physics course, you can understand that the most dangerous will be the interaction of a magnetic field with ferromagnets. Metals called dia- and paramagnets interact with a magnetic field much weaker, so they are considered practically safe.
Ferromagnets that actively interact with the tomograph field are capable of changing the field itself, heating up under its influence, changing their shape, etc. This is unacceptable, both from the point of view of distorting the readings of the MRI machine (the accuracy of the diagnosis depends on this), and due to the fact that the heated metal can lead to tissue burns, and changes in its shape will not allow the implant to perform its assigned function. Again, the health, and sometimes the life of the patient, depends on this.
The MRI procedure cannot be performed if the patient has:
- inner ear prostheses (cochlear implants, which are a kind of hearing aid),
- vascular clips (especially in the head area),
- metal stents in blood vessels,
- artificial heart valves,
- implanted pumps (insulin pump),
- joint and bone prostheses made of metal,
- nerve stimulants,
- pins, screws, surgical staples, shell fragments and other small objects,
- fixed metal dentures and fillings
- tattoos using materials (colorants) containing ferromagnetic particles.
Not all of the above-described devices and objects interact with a magnetic field. We are talking about ferromagnetic implants. It is best if the patient knows in advance what material the device implanted in his body is made of.
X-rays help to detect small metal parts. Therefore, you should not neglect this method of examination before an MRI, especially if you have any doubts.
The magnetic field also affects electronic devices. Therefore, the presence of an implanted pacemaker and other electronic devices, on the operation of which a person's life depends, is also considered a contraindication to MRI.
It is believed that such a safe technique as MRI can worsen the condition of patients with heart failure in the decompensation stage. The decision on the possibility of examination in such patients is made by a cardiologist. In the acute stage of the disease, such manipulations should be abandoned.
It is also undesirable to conduct MRI during pregnancy, but since we are talking only about the upper part of the body, and this method is considered the safest, if necessary, diagnostics are still carried out in open-loop devices. If there is no urgent need for diagnostics, it is better to wait until the birth of the child.
MRI of the shoulder joint with contrast, which allows to detect tumor processes at different stages of their development and to assess the condition of blood vessels, is not prescribed for various skin thickenings, kidney pathologies (because the contrast is excreted from the body with their help), asthmatic status, blood diseases. It is undesirable to administer contrast during pregnancy (especially in the 1st trimester) and breastfeeding. In the latter case, the woman will have to stop breastfeeding for a while.
Normal performance
MRI diagnostics are designed to avoid negative consequences of the device operation as much as possible. For example, the device is equipped with a speakerphone, and the patient can notify the doctor of any unpleasant sensations remotely during the diagnostics. So, in devices with a closed circuit, a person may begin to feel anxious, there may be a feeling of lack of air, etc. Usually, it is enough to calm the patient down to complete the procedure. But in some cases, the study may even be interrupted.
During the procedure, the patient is under the supervision of a physician and relatives, who are allowed to be present during the diagnostics as support.
Tomographs have a small drawback. During operation, they produce a noticeable noise that can irritate the patient's hearing. To avoid this, subjects are given earplugs or headphones. During the shoulder joint MRI procedure, they can listen to light music or enjoy the silence.
Complications after the procedure
There are usually no complications after an MRI procedure. The exception is situations when a person did not know about the presence of metal objects in the body or deliberately hid it. There have been cases of skin burns and people with tattoos made using metal-containing paints.
Ferromagnetic implants can theoretically move and heat up under the influence of a magnetic field, but the heating temperature is usually relatively low, and the implants themselves are attached very firmly, and it is unlikely that the tomograph will be able to move them from their place.
Some unpleasant sensations may accompany patients during MRI with contrast. This includes skin irritation, slight itching, and a slight decrease in blood pressure. However, only two out of a hundred patients complain of such side effects from the use of contrast agents. Usually, this is an intolerance to the contrast itself.
Patients may also complain of slight nausea and headaches. But these symptoms are also not related to the magnetic field. This is a reaction to chemicals (contrasts). If you avoid eating and drinking before the procedure, nausea usually does not appear. And the headache goes away fairly quickly, but you can take analgesics if necessary.
Care after the procedure
MRI diagnostics of the shoulder joint is also attractive because no care is required after the procedure, because the technique does not imply a violation of the integrity of tissues or interference in the functioning of the body. The patient only needs to follow the doctor's orders, undergo surgical treatment if necessary, and not neglect restorative procedures to solve the problem that provoked the visit to the doctor.

